1. Background
Health promotion hospitals (HPHs) integrate health promotion and disease prevention into their core functions, addressing the root causes of illnesses and improving population health. Preventive clinics within HPHs employ evidence-based strategies to identify risk factors and deliver personalized interventions, thereby reducing the burden of chronic diseases such as diabetes and hypertension. In Iran, despite advancements in healthcare access, the integration of preventive care remains underdeveloped due to limited infrastructure, cultural barriers, and fragmented workflows (1, 2). However, opportunities exist through the adoption of international best practices, strengthening policy support, leveraging digital health technologies, and increasing public awareness (3). Prioritizing preventive care can lower healthcare costs, improve community health, and build a resilient healthcare system aligned with global goals (4, 5).
Currently, 60 to 80 major public and academic medical centers in cities such as Tehran, Mashhad, Isfahan, Shiraz, and Tabriz, along with 20 to 30 private facilities, offer specialized preventive services (6, 7). These clinics, located in hospitals such as Imam Khomeini, Shariati, Milad, Rasul Akram, Sina, Ali Ibn Abi Talib, and Ganjavian, provide essential services including screening, health education, counseling, and occupational health exams (8). However, the number of hospitals with active preventive clinics remains insufficient. Challenges such as resource limitations, low public awareness, and inefficient workflows hinder expansion. Yet, growing public awareness and the integration of health information technologies offer opportunities for improvement (9, 10).
2. Objectives
The present study emphasizes optimizing workflows in preventive clinics and advocates for a community-centered approach tailored to local population needs. By adopting advanced technologies and innovative strategies, it aims to evaluate current workflows and design effective interventions to enhance health outcomes. Prioritizing preventive care and addressing systemic challenges can create a sustainable healthcare system, reduce disease burdens, and improve social health in Iran.
3. Methods
3.1. Study Design
The present study adopted a descriptive, cross-sectional design to evaluate and enhance the clinical process flowcharts of preventive clinics. The primary objective was to identify gaps in service delivery and propose evidence-based interventions to optimize preventive care workflows. The study was conducted from August to October 2019 and focused on four preventive and health promotion clinics in Tehran, Iran.
3.2. Study Setting and Sampling
Four preventive and health promotion clinics were selected using a convenience sampling method, ensuring diversity in operational capacity, service offerings, and geographical representation. The selection criteria prioritized accessibility, operational capacity, and the diversity of services provided. The selected clinics included: (1) Shahid Rajaei Cardiovascular Training, Research, and Treatment Center; (2) Imam Khomeini Hospital; (3) Baharloo Hospital; (4) Valfajr Prevention and Family Physician Clinic under the supervision of West Health Center.
These clinics were chosen due to their accessibility, operational capacity, and the diversity of preventive services they offer, ensuring a representative sample of preventive care facilities in Tehran.
3.3. Data Collection
Data were collected through:
(1) Observations: Direct observation of clinic operations was conducted to assess workflow efficiency, service delivery, and patient interactions.
(2) Checklist assessment: A checklist, divided into three sections with 14 criteria, was used to evaluate key aspects of service delivery, including: (A) Information and content production (e.g., educational media, active websites); (B) supportive programs (e.g., insurance services, official support); (C) service provision (e.g., patient admissions, specialized software, follow-up visits).
3.4. Data Analysis
(1) Strengths, weaknesses, opportunities and threats (SWOT) analysis: A comprehensive SWOT analysis was conducted to evaluate the current state of preventive services. The SWOT table was reviewed and validated by specialists in community and preventive medicine, internal medicine, and geriatrics to ensure accuracy and relevance.
(2) Process flowchart development: Using Microsoft Visio software, standardized process flowcharts were created to visualize and optimize clinic workflows. These flowcharts were designed to align with national health guidelines and community health priorities.
(3) Compliance assessment: Activities and sub-activities were mapped against national health system guidelines to ensure compliance. Each activity was assigned a direct manager to oversee implementation and adherence to standards.
4. Results
In the first section, findings from the visits (Table 1) indicate that only 25% of clinics actively advertised prevention services. Most visitors to preventive and health promotion clinics were existing patients, with only 25% being apparently healthy individuals seeking screening. Clinicians provided educational services to patients and their companions during initial appointments in 25% of cases, with no follow-up. Only one clinic complied with standard guidelines, while 75% had access to specialists, psychologists, and nutrition experts. In one clinic, a community and preventive medicine specialist worked in isolation without collaboration with other specialties.
| Main Sections and Criteria | No. |
|---|---|
| Information and content production | |
| Existence of advertisements | |
| Yes | 3 |
| No | 1 |
| Presence of clinic signboards | |
| Yes | 4 |
| No | - |
| Location of the clinic | |
| In clinics main hall | 2 |
| In separate building | 2 |
| Produce educational media | |
| Yes, a lot | 1 |
| Yes, limited | 3 |
| No | - |
| Active website | |
| Yes | 2 |
| No | 2 |
| Supportive programs | |
| Official support | |
| Completely | 3 |
| Relatively | 1 |
| Insurance services | |
| Yes, completely | 1 |
| Yes, relatively | 2 |
| No | 1 |
| Specific software | |
| Yes | 1 |
| No | 3 |
| Providing services | |
| Admitted patients | |
| All patients | 1 |
| Some patients | 2 |
| Seemingly healthy people | 1 |
| The main task of the preventive physician | |
| Only patient education | 1 |
| Student education | 2 |
| Patient visit | 1 |
| Screening clients | 2 |
| Existence of a specialized team | |
| Medical specialists | 1 |
| Some of experts | 2 |
| No team | 1 |
| Use of specific guidelines | |
| Yes, completely | 1 |
| Yes, relatively | 2 |
| No | - |
| Without screening | 1 |
| Measuring clients satisfaction | |
| Yes, completely | 1 |
| Yes, relatively | 2 |
| No | 1 |
| Subsequent follow up | |
| Yes | 3 |
| No | 1 |
Insurance utilization for certain prevention services was unclear, and only two clinics (50%) had active websites. One site disseminated educational media, while the other was used for screening questionnaires. Only one clinic (25%) employed specific software for screening. In the second section, a SWOT analysis for preventive services was developed based on the perspectives and observations of clinic officials, augmented by insights from five specialists (Table 2).
| Variables | Results |
|---|---|
| Strengths | Existence of young and motivated faculty members |
| Support of most senior university officials to activate clinics | |
| Relatively high number of people referring to the university hospital clinics | |
| Weaknesses | Lack of integrated software system |
| The failure of most specialists to attract people to prevention clinics | |
| Most related documents were not up to date | |
| Different processes and activities of prevention clinics | |
| Incomplete referral process | |
| Opportunities | Sensitivity of members of society to public health |
| Existence of new guidelines and resources in the field of prevention | |
| Ability to use the capacity of municipalities and other institutions | |
| Possibility of using technology in the field of prevention | |
| Increasing life expectancy and the need to improve the quality of life | |
| Threats | Some officials are doubtful about the efficiency of clinics |
| High cost of some tests and para clinics | |
| High rate of inflation in the above costs | |
| Lack of insurance coverage for prevention services | |
| Not considering the need for preventive counseling in patients admitted to ICU and CCU wards |
The third section delineated activities for target groups, including:
- Special services for employees, discharged patients, and hospitalized patients, with an emphasis on risk factor identification and management.
- Population-based services for municipal employees and factory workers, offering screening and educational services.
- Research services that support knowledge-based activities in prevention and health promotion.
- Educational services for community and preventive medicine specialists, medical interns, and clerkships.
In this context, Table 3 serves as a comprehensive summary of specific interventions tailored for each disease, categorized by age and sex. This table enhances the understanding of the diverse needs of patients, emphasizing the importance of personalized approaches in healthcare.
| Titles/Actions | Frequency of Intervention | Description | Age of Starting of Intervention (y) |
|---|---|---|---|
| Prevention of chronic diseases (SNAP) | |||
| Cigar S | First opportunity/at each visit | - | 13 - 18 |
| Overweight N | Once every 2 years | - | 13 - 18 |
| Nutrition | Once every 2 years | In people with increased risk: Every 6 months | 13 - 18 |
| Diagnosis of alcohol consumption A | - | Provide educational brochures | 13 - 18 |
| Physical activity P | Once every 2 years | In high-risk people, at every visit | 13 - 18 |
| Sexual health | |||
| STD and Chlamydia | First opportunity/every year | If there is sexual activity (marriage) | 13 - 18 |
| Prevention of vascular disease | |||
| Absolute risk assessment CV | Once every 2 years | - | 40 - 45 |
| blood pressure | Once every 2 years | In people at increased risk of CVD every 6 to 12 months/in high-risk people every 6 to 12 weeks | 13 - 18 |
| Cholesterol and other fats | Once every 5 years | In people at higher risk: Once every 1 to 2 years | 45 - 49 |
| Type 2 diabetes | Once every 3 years | In IGT and IFG every 12 months | 40 - 45 |
| Stroke | Every year | Recommended for people at increased risk | - |
| Kidney disease | Once every 1 to 2 years | Recommended for people at increased risk | - |
| Cancers | |||
| Skin cancer | Occurs at every opportunity | In high-risk individuals every 2 to 3 months | - |
| Cervical cancer | Once every 2 years | To be done until the age of 69 | Marriage-the beginning of sexual activity |
| Breast cancer | Once every 2 years | To be done until the age of 69 | 50 |
| Colon cancer | Once every 2 years | High-risk people with shorter distances | 50 |
| Psycho-social | |||
| Depression | High risk: Every visit | Every opportunity has come | 13 - 18 and elderly |
| Domestic violence | Occurs at every opportunity | Pregnant women should also be considered | 13 - 18 and elderly |
| Elderly | |||
| Danger of falling-falling | Every year | With a history of falls: Once every 6 months | 65 |
| Sight and hearing | Every year | - | 65 |
| Oral health | At least every year | With an emphasis on people at increased risk | - |
| Osteoporosis | |||
| Women | Every year | By specific risk assessment | 45 - 49 |
| Men | Every year | By specific risk assessment | 50 |
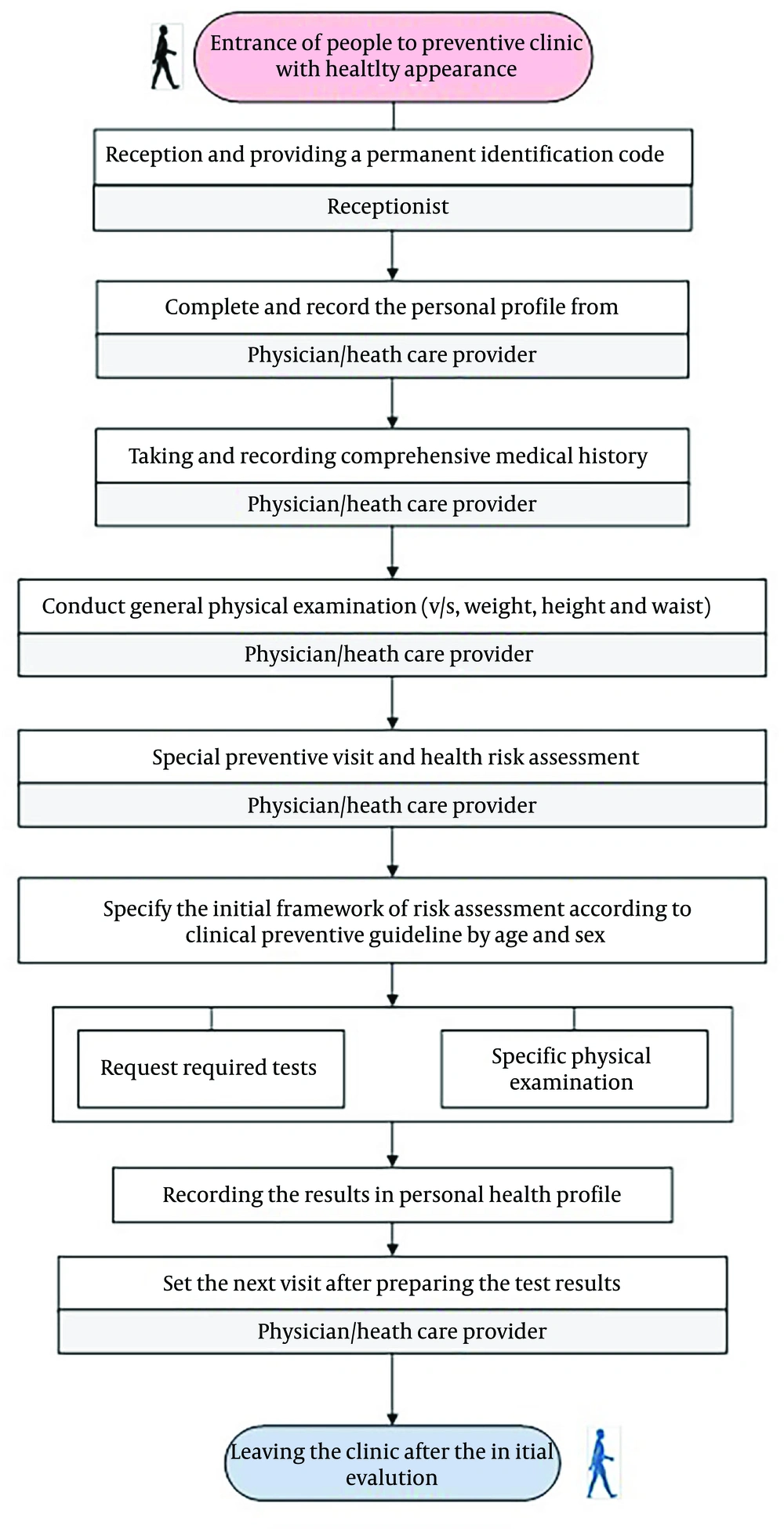
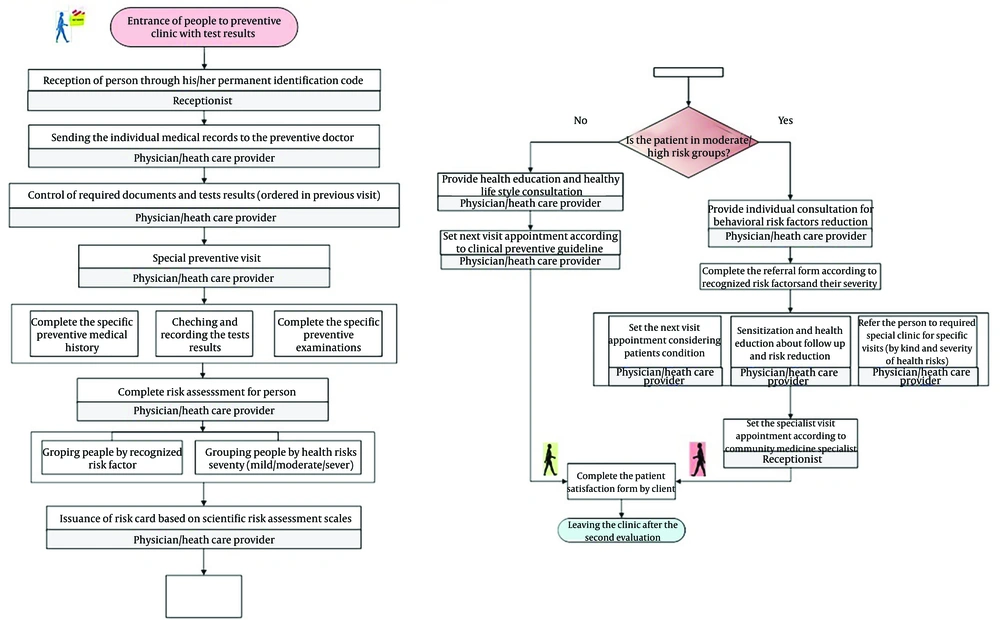
In the fourth section, several key process flowcharts related to clinic activities were revised and finalized by experts using Visio software (Figures 1 and 2).
5. Discussion
The present study critically evaluates and proposes strategies to enhance the flowcharts governing preventive clinics and family physician services. Initial process flowcharts and risk assessment tables tailored to age-gender groups were designed and presented (11). Clinics operating under the titles of preventive care or family medicine provide services based on predefined objectives, but their prioritization of core prevention principles remains questionable (12). These clinics should function as nexus points between health promotion and medical treatment, directing clients through established referral processes.
Comprehensive policy frameworks by the Ministry of Health are essential to ensure a systematic approach to preventive care. Research by Parsaye et al. (13) in Iran, along with Shewade and Chinnakali (14) in India, highlights actionable strategies for health-promoting hospitals. A key challenge is the insufficient concern among senior hospital officials regarding preventive health measures, as identified by Thanh et al. (15) and Hudon et al. (16). Barriers to preventive care can be alleviated through targeted training and empowerment initiatives for physicians and managers, supported by senior officials. Disseminating information about preventive services and attracting healthy individuals to health centers remain significant challenges. Patients are often referred only after symptomatic disease onset (16). While one hospital’s website demonstrated effective information dissemination (17), extending this to all centers is crucial. Parsaye et al. (13) recommend strategies like dedicated websites and educational materials to enhance awareness. Outreach initiatives beyond clinical settings, such as collaborations with organizations, can facilitate employee screening.
A four-stage referral system is recommended: Enhancing public awareness, identifying health needs, developing an electronic referral system, and monitoring quality through patient feedback. An integrated model for preventive services enhances care quality and fosters networking among centers. Patients referred to other clinics are often overlooked for preventive evaluations, highlighting the need for opportunistic screening (14). Community and preventive medicine specialist practitioners oversee preventive services in hospitals, but studies emphasize the involvement of primary care physicians and community health professionals (18, 19). Preventive clinics should operate as collaborative teams integrating specialists, general practitioners, and other relevant fields. The lack of an integrated framework based on clinical guidelines leads to varied approaches among clinics. Evidence-based guidelines and electronic health records (EHR) can enhance service delivery, though challenges like user information protection must be addressed (20). Insurance coverage for preventive services is another concern, as high costs hinder accessibility (20, 21). Comprehensive insurance solutions at macro policy levels are essential to support preventive care.
5.1. Conclusions
Based on this study, by leveraging potential opportunities both inside and outside the system, obtaining the support of health managers for preventive services, providing a screening approach, and using standard and up-to-date process flowcharts in accordance with community priorities, the services of these clinics can be significantly improved.
5.2. Limitations
The use of convenience sampling may restrict the generalizability of the findings to other contexts. Future research should consider employing a randomized sampling approach to enhance external validity.