1. Background
Non-specific low back pain (NSLBP) is one of the most common complications and disabilities, with a lifetime prevalence of approximately 40% of the general adult population worldwide. It is also known as the second most common reason to see a doctor (1, 2). The NSLBP involves pain in the back and sacroiliac joint area, with or without lower limb discomfort. Objective examination is not able to determine its origin. It is associated with a reduction in life quality for the affected individuals and can cause limitations of activity, functional impairment, fear of movement, depression, work absenteeism, negative social relations, and somatization (3).
Changes in the fascia structure can cause limited function of the back and deep trunk muscles (4, 5). Notably, the etiology of back pain can be attributed to the superficial back line, comprising structures such as the sacrolumbar fascia, plantar fascia, hamstring muscles, gastrocnemius muscle, erector spinae muscle, and epicranial fascia (6). A theory suggests that there is a link between lower extremity dysfunction and back pain, indicating that back pain can be caused by lower extremity dysfunction.
Studies investigating the effectiveness of conservative, surgical, and pharmacological interventions for NSLBP have been continuously conducted over numerous years. However, a considerable number of these strategies may incur high costs and exhibit occasional inefficacy (3). In the present study, this is the first time that compares two common conservative interventions of cupping therapy (CT) and myofascial release (MFR) on low back pain symptoms.
The CT is a common traditional therapy used for thousands of years, which could be used to decrease back pain symptoms (7). Those interested in using CT to treat back problems and reduce pain are encouraged by its perceived safety and effectiveness compared to common therapeutic programs. Despite CT’s general safety, pigmentation on the local skin may occur, which gradually fades within a few days. However, complications such as anemia have been reported following excessive CT by an unqualified therapist (8).
According to the standards set by Zhang et al., several cases in CT technique, including the type of CT and method of implementation and application, must be considered (9). Various types of CT include wet CT, dry CT, CT with retention, shaking CT, moving CT, and balance CT. In China, all types of CT are used frequently, while dry CT and wet CT are widely used in Asian and Middle Eastern countries (10). Dry CT involves sucking the skin into the cup without drawing blood by using the negative pressure conditions of the cup. The CT with retention means that the cup stays on the skin after the dry CT process is finished. Moving CT involves moving the skin using oil to facilitate movement. Wet CT requires penetrating the skin to draw local blood into the cup. Balance CT combines CT with retention, shaking CT, quick CT, and moving CT (1).
Moura et al., in a systematic review, examined the effect of CT on back pain and indicated that the cause of pain reduction as a result of CT has not been fully determined (11). Although they presented different hypotheses such as metabolic, neurological, or Chinese medicine effects, limitations such as quality reduction in some cases, lack of control groups, and lack of reference to effective protocols were noted. Despite the effectiveness of these measures on back pain, it is unclear how effective they are, whether the treatment’s effectiveness is active, fabricated, or indoctrinated, whether the treatment follows therapeutic standards, or whether the treatment is not performed at all. They recommended that differences such as age, sex, diagnosis, and the techniques used can impact the results. In conclusion, they recommended that CT is a promising method for the treatment of NSLBP in patients, and there is a need to establish standardized application protocols for this intervention (11).
In contrast, in recent years, MFR has been introduced to improve musculoskeletal injuries and alleviate pain, with clinical application and MFR-related experiments showing an increasing trend (3). Recent research indicates the reduction of fibrous adhesion and relief of symptoms in acute and chronic conditions when MFR is applied (3). Moreover, MFR relaxes and expands soft tissue, improves local circulation, and restores the restricted joints’ range of motion (ROM), which helps improve stiffness, muscle pain, or extreme fatigue (12, 13).
2. Objectives
Given the significance of employing evidence-based appropriate clinical interventions to ameliorate the symptoms of NSLBP, the objective of this study was to ascertain whether CT and MFR interventions could enhance the health-related quality of life in patients with NSLBP. Evidence supports the use of CT and MFR in managing NSLBP. However, no studies have compared the efficacy of these techniques together yet. Notably, we evaluated the effect of the interventions on pain, functional disability, balance, and quality of life in females. It was also hypothesized that both interventions would improve the health-related quality of life in patients with NSLBP.
3. Methods
3.1. Participants
This study required 26 female participants with NSLBP according to G*Power software version 3.1 (Franz Faul University of Kiel, Germany). This study required an alpha level of 30 female participants, accounting for a 15% dropout rate/loss in follow-up. Participants were randomly allocated to the MFR (mean age, 41.45 ± 7.27 years; height, 161.48 ± 3.31 cm; and mass, 68.93 ± 3.45 kg) and CT (mean age, 40.27 ± 6.64 years; height, 160.15 ± 3.87 cm; and mass, 65.47 ± 2.79 kg) groups in a 1:1 ratio. A non-participating investigator used a computer-generated random allocation number to accomplish this. There was no investigator involved with the study. The present study recruited participants through the board and the nearby physiotherapy clinic of the university.
Inclusion criteria were: The significance of employing reputable, clinical interventions to alleviate the signs and symptoms of NSLBP is evident in this study, which sought to determine whether cupping therapy and myofascial release therapies could enhance the health-related well-being of individuals with NSLBP. Females aged 25 - 45 years with chronic NSLBP (pain lasting > 3 months), Visual Analog Scale (VAS) score ≥ 3, no specific pathological diagnosis for back pain, and no physical therapy in the previous 3 months. Participants were excluded if they had specific spinal pathologies (e.g., herniated disc, spondylolisthesis), neurological deficits, pregnancy, skin conditions preventing CT/MFR, history of spinal surgery, or systemic inflammatory diseases.
The Sport Sciences Research Institute obtained ethical approval before the test. The participants provided written informed consent.
3.2. Procedures
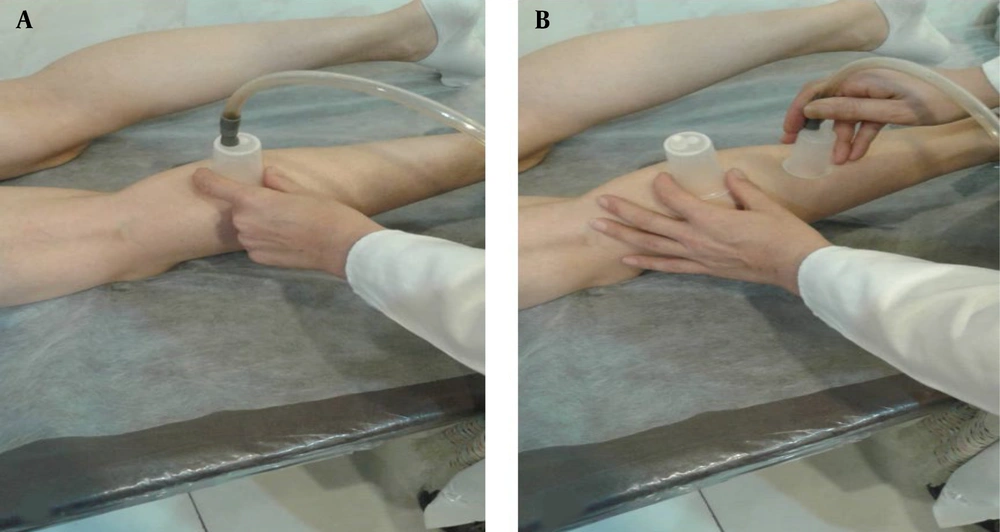
In the present study, subjects in the CT group received the cupping interventions, and subjects in the MFR group received the MFR intervention programs, which were performed for four weeks, three sessions a week on even days. The CT intervention program was performed for approximately 40 minutes per session. Using the Maxxi model suction device with a negative pressure measurement of 400 mm Hg, the device was turned on, and with a gentle pull on the skin, the cupule was moved in a circular motion to stretch all the muscles of the back of the leg. At the end of the CT on one leg, similar actions were performed on the opposite leg (Figure 1).
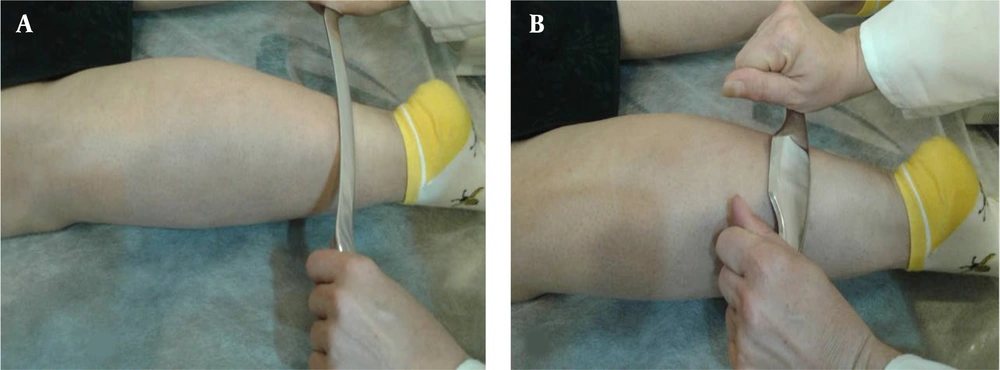
In contrast, the MFR intervention program was performed for approximately 30 minutes per session for each subject. After preparing the subjects to apply MFR, they were asked to lie on the examination table. A suitable lubricant was used to facilitate the movement of an instrument on the skin to prevent skin injuries when MFR was applied. First, using the GT1 Graston instrument, the muscles were gently pressed from the distal to the proximal, focusing on trigger points (Figure 2A). After that, a larger part of the muscle was pressed using the GT2 Graston instrument (Figure 2B). These procedures were done for the opposite leg too.
Each participant was provided with written instructions describing the interventions and program specifics. The intervention was designed following the FIIT principles:
- CT group: Frequency - 3 sessions/week; intensity - 400 mmHg negative pressure; time - 40 minutes/session; type - moving cupping on posterior lower extremity muscles with 5 passes per muscle group.
- MFR group: Frequency - 3 sessions/week; intensity - moderate pressure (subject-reported 5/10 discomfort); time - 30 minutes/session; type - instrument-assisted MFR using GT1 and GT2 Graston tools with 3 sets of 30-second strokes per muscle group.
Notably, all interventions were performed by the same licensed physical therapist with 8 years of musculoskeletal experience and certifications in both CT and instrument-assisted soft tissue mobilization.
In this study, we measured Oswestry Disability Index (ODI), VAS, Berg Balance Scale (BBS), and WHO Quality of Life (WQL) before and after the intervention. Both of these measurements were checked at the beginning and end of the 4 weeks of treatment.
3.3. Outcome Measures
(1) Oswestry Low Back Pain Disability Questionnaire: The Disability Index of NSLBP was evaluated using the ODI to assess the Disability Index. The modified ODI includes 10 condition-specific measures of pain and disability for individuals with NSLBP. Each question is scored from 0 to 5, and the total score is then multiplied by 2 and expressed as a percentage (14).
(2) Visual Analog Scale: A VAS (0 - 10 cm) was used to assess the degree of discomfort, with zero representing no discomfort and 10 representing the most intense pain. A VAS score of 1.7 cm is reported as a minimal clinically significant difference (15).
(3) Berg Balance Scale: To measure balance using the BBS, subjects were asked to perform tasks ranging from sit-to-stand to standing on one leg. The subjects’ performance in completing each task was assessed based on their quickness, stability, and the amount of assistance required. The BBS consists of 14 balanced activities rated on an ordinal scale of 0 to 4, for a total of 56 points, indicating a lower risk of falling and the capability of accomplishing the task independently (16, 17).
(4) WHO Quality of Life: The WQL Questionnaire includes 26 items with a five-point Likert scale response format, representing four different domains that assess quality of life: Physical health (7 items), psychological health (6 items), social relationships (3 items), and environmental health (8 items) (18, 19).
3.4. Statistical Analysis
Descriptive analysis was performed on all variables. The normality of data distribution was confirmed using the Shapiro-Wilk test. Consequently, a two-way mixed model analysis of variance was conducted. The between-subjects factor was the group (massage, cupping), and the within-subject factor was time (pretest, posttest). Effect size was determined using the Cohen d coefficient, interpreted as follows: d = 0.80 for large, d = 0.50 for medium, and d = 0.20 for small. The significance level was set at P < 0.05. All statistical analyses were conducted using SPSS version 22.0 (Microsoft Corp., Redmond, WA).
4. Results
The results of a mixed model analysis of variance indicated that the group-time interactions and the main effect for the group were not significant for all measurement outcomes (P > 0.05). Nonetheless, there was a significant main effect of time (VAS, P = 0.001; ODI, P = 0.001; BBS, P = 0.001; WQL, P = 0.001). The results of the Bonferroni post hoc test showed that all parameters improved after the intervention in both groups (P < 0.05) (Table 1).
| Variables | Group | Outcome measures | |||||
|---|---|---|---|---|---|---|---|
| Massage | Cupping | ||||||
| Pre-intervention | Post-intervention | Pre-intervention | Post-intervention | Time Main Effect | Group Main Effect | Group × Time Interaction | |
| VAS (cm) | 4.78 ± 1.43 | 3.83 ± 1.46 | 5.00 ± 1.45 | 3.72 ± 1.52 | P = 0.001; F = 32.458; ES = 0.448 | P = 0.902; F = 0.015; ES = 0.001 | P = 0.399; F = 0.730; ES = 0.021 |
| ODI (%) | 50.22 ± 11.60 | 46.22 ± 12.12 | 49.72 ± 11.55 | 47.55 ± 12.21 | P = 0.001; F = 19.378; ES = 0.363 | P = 0.915; F = 0.011; ES = 0.001 | P = 0.199; F = 1.713; ES = 0.048 |
| BBS (%) | 48.61 ± 8.46 | 53.89 ± 8.34 | 49.00 ± 6.69 | 52.11 ± 7.93 | P = 0.001; F = 38.371; ES = 0.530 | P = 0.053; F = 4.033; ES = 0.106 | P = 0.490; F = 0.488; ES = 0.014 |
| WQL (%) | 69.05 ± 21.99 | 74.89 ± 23.98 | 76.78 ± 19.51 | 83.33 ± 19.06 | P = 0.001; F = 46.184; ES = 0.576 | P = 0.257; F = 1.327; ES = 0.038 | P = 0.694; F = 0.157; ES = 0.005 |
5. Discussion
We investigated the effect of four weeks of CT and MFR on pain, functional disability, balance, and quality of life in females with NSLBP. The results of the study indicated improvement in all evaluated parameters in both groups; interestingly, no between-group difference was observed. Previous studies have reported that lower extremity stiffness is associated with injuries, including NSLBP (20). It has been reported that hamstring stiffness is higher in patients with NSLBP than in healthy adults. Hamstring stiffness can limit pelvic lumbar ROM, leading to posterior tilt and reduction of the lumbar curve, contributing to NSLBP (21). Therefore, hamstring muscle release is important to reduce the load on the lumbar region during daily activities. Additionally, due to the juncture between the hamstring and gastrocnemius through the deep fascia in the popliteal region, gastrocnemius stiffness can affect lumbar motions (22).
In the present study, we observed improvement in the evaluated parameters after CT and MFR intervention on lower extremity muscles. It would be logical to infer that NSLBP may be partially associated with the stiffness of the lower extremities. Furthermore, hamstring stiffness also reduces pelvic motility (20). The altered kinetic chain shows inadequate energy transfer from the lower to the upper limb in subjects with hamstring stiffness. Subjects engage in excessive compensatory movements due to defective biomechanics, which tend to increase the force produced by the lower limb.
In the CT group, the results of the current study showed improvement in VAS, ODI, BBS, and WQL after applying CT for 4 weeks. There are many physiological changes thought to occur with CT that affect tissue change. Increased blood flow is one of the orthopedic effects of CT (23). Furthermore, it has been suggested that CT can release connective tissue, leading to increased flexibility (24). It is assumed that any physiological changes due to CT are sufficient to improve muscle stiffness and NSLBP symptoms, even though the current study did not directly measure these potential physiological effects.
In the MFR group, similar to the CT group, subjects exhibited improved VAS, ODI, BBS, and WQL after the four-week intervention. These results suggest that MFR of the lower extremity increases the range of muscle by changes in muscle fibers and fascia structure, which helps improve the lumbar ROM. Additionally, from a physiological perspective, pain relief as a result of the MFR effect may be related to the removal of the obstruction of deep fascia and promoting fluid circulation in and around tissues (3).
Overall, the results of the current study suggest that MFR and CT of lower extremity stiffness improve NSLBP symptoms, which can be interpreted with the superficial back line effect of the anatomy trains suggested by Myers (25). The implemented interventions were scrutinized by various researchers. In a systematic review, Webb and Rajendran demonstrated that MFR reduces hamstring pain and increases joint mobility. The systematic review demonstrated that MFR reduces hamstring pain and increases joint mobility (26). Hyong and Kang found that stretching the hamstrings without moving them helped improve neck mobility and balance (27).
Interestingly, we found no statistical significance in group differences in relation to evaluated parameters. This might be because both the CT and MFR treatments affect NSLBP symptoms in some way. As an evidence-based clinical guideline for the management of NSLBP, a comprehensive understanding of the CT and MFR interventions' effect on back pain symptoms is necessary.
Limitations of this study should be considered. Our data cannot be generalized to all ages and sexes because the age and gender of the subjects were restricted to females aged 25 to 45. Some subjects may experience pain during the pre- and post-intervention phases because the menstrual cycle of the subjects in the present study was not considered. Third, the effects of both interventions were compared with themselves pre-intervention rather than a placebo condition. The observed improvement in the assessed parameters may be attributed to random chance.
5.1. Conclusions
Based on these findings, both CT and MFR can be recommended as effective treatment options for NSLBP in clinical practice. Future studies should investigate longer-term effects and include male participants and different age groups to enhance generalizability. Additionally, it would be reasonable to infer that NSLBP might be partly related to lower extremity stiffness.