1. Introduction
Gastric cancer is a life-threatening condition with unfavorable survival rates globally. The World Health Organization (WHO) classified gastric cancer histologic patterns into subtypes including papillary, tubular, mucinous, poorly cohesive (signet ring cell carcinoma), and mixed (1, 2). In the early stages, most individuals may not display any particular symptoms, leading to a diagnosis in the advanced stages of the disease. Nonetheless, symptoms such as weight loss and weakness, which are commonly observed in most malignancies, as well as abdominal pain and dysphagia, are usually reported (3). According to data from stage distribution of SEER incidence cases, 2012 - 2021, about 33.7% of cases with gastric cancer show distant metastasis involvement (4). The liver is the most common site of metastases (48%) and the bone accounts for 12% of metastatic cases (5).
Colorectal cancer is a malignancy that starts in the colon or rectum, which are part of the digestive system. It is the third most commonly diagnosed cancer and the second mortality cause with adenocarcinoma being the most prevalent type (6, 7). Screening and treatment developments have improved survival rates for this malignancy in recent years. Unfortunately, metastatic cases still have a poor prognosis (8). Approximately 20% of patients present distant metastasis, with a higher prevalence noted among younger individuals (9). Bone marrow involvement is rare and usually brings survival under one year (10).
Cytopenia is a condition characterized by a reduction in the quantity of blood cells, affecting one or multiple cell types. The effects of decreased cell types can manifest in various ways, including thrombocytopenia, anemia, neutropenia, or leukopenia (11). The situation may arise from hematological or other factors; therefore, workup depends on the underlying condition (12). When reduction is observed in two cellular elements, the condition is referred to as bicytopenia (13). There are very few reports of patients with gastrointestinal (GI) cancers having bicytopenia as an initial manifestation (14). We discuss 2 patients with gastric and colorectal cancer showing bicytopenia without any related GI symptoms. Diagnosis in these cases can be a challenge and requires a multidisciplinary approach.
2. Case Presentation
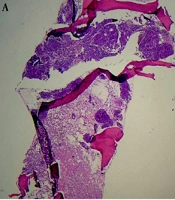
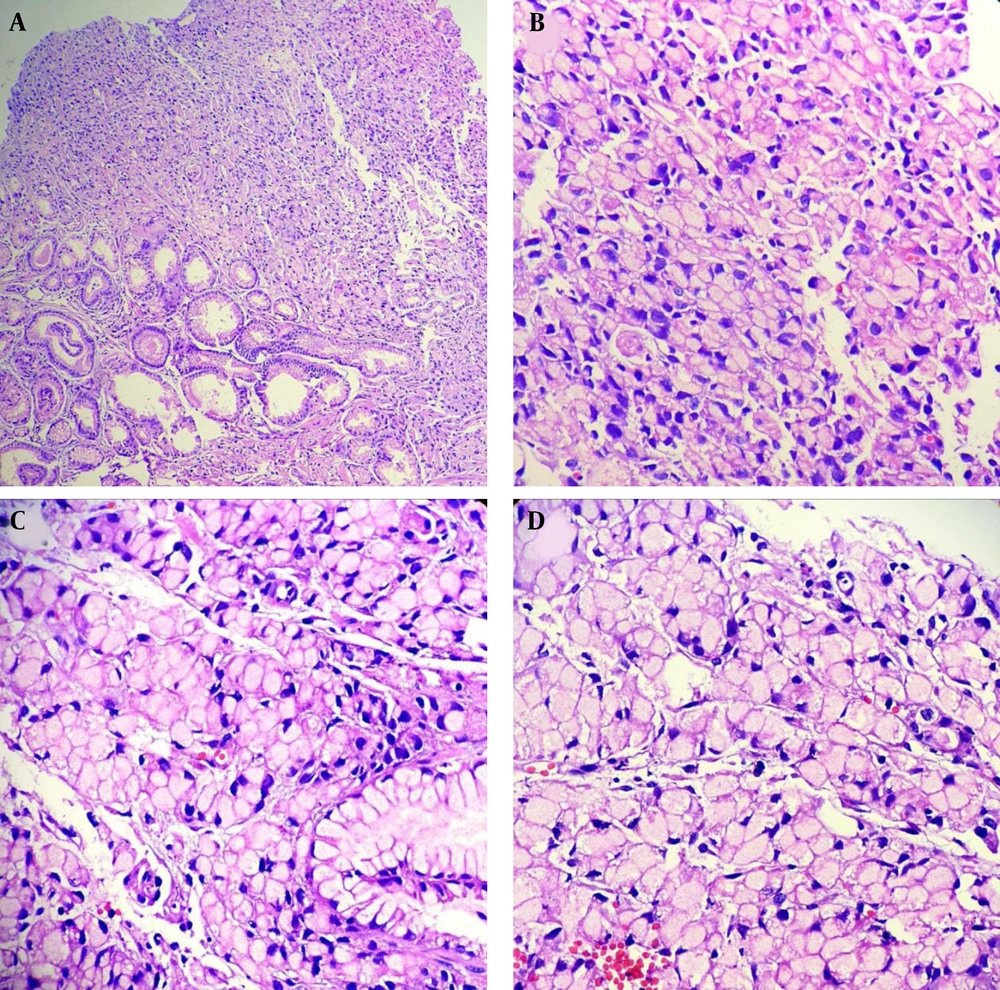
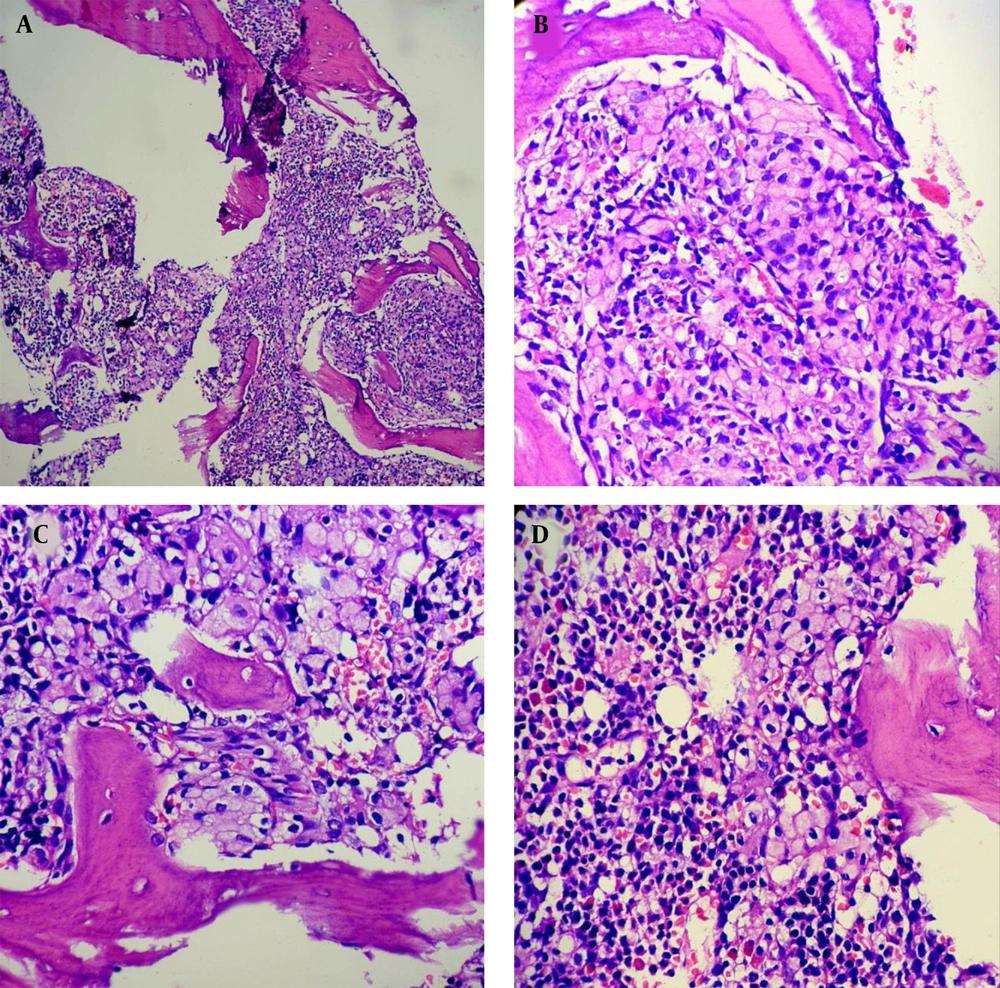
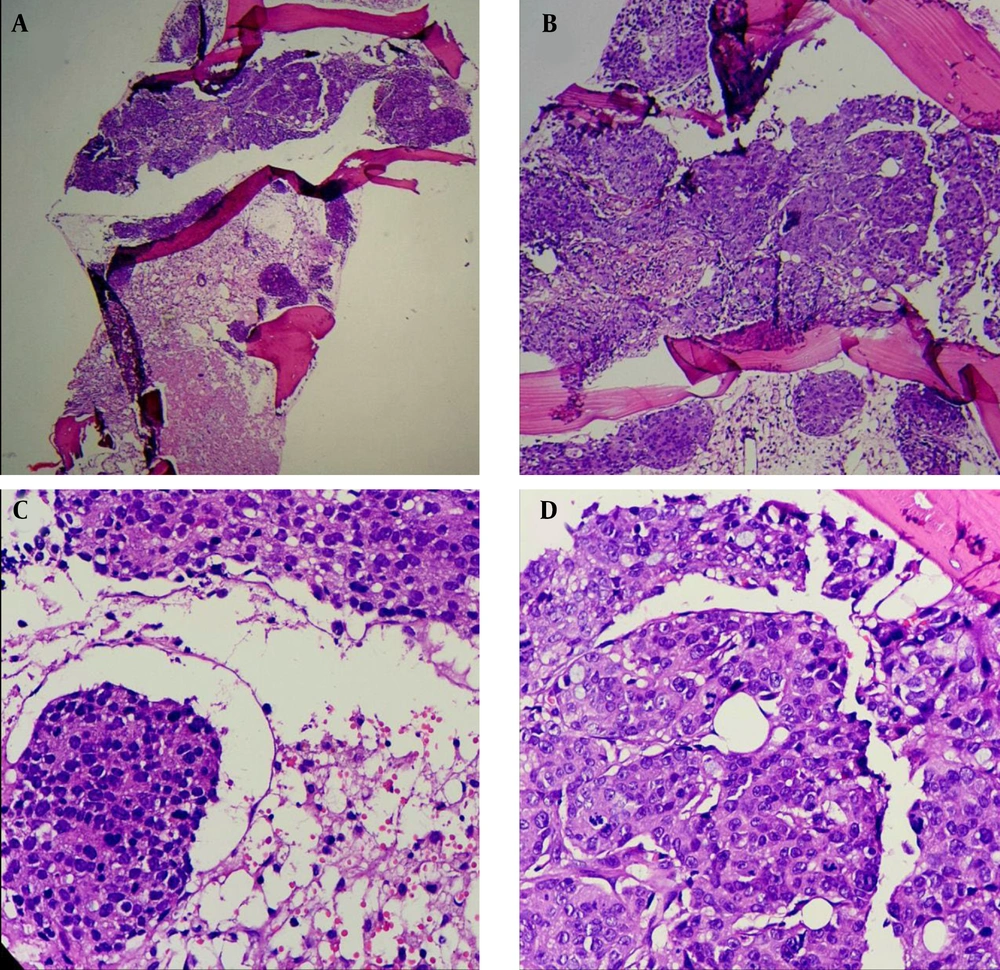
- Number 1: A 54-year-old man went to the emergency room due to progressive weakness and lethargy that started 10 days ago. He had a mild fever at the time of the visit. Vital signs were stable. The patient mentioned very severe weakness and headache, but medical history was nonsignificant. Abdominal, pelvic, and chest examinations were normal. Peripheral blood slide was evaluated. There were more than 5% schistocytes. The platelet count was around 10,000/mcL. Abnormal cells were not observed in the white blood cell category. nRBC was observed in the slide. A primary diagnosis of TTP was considered, and emergency plasmapheresis was prescribed. The administration continued on a daily basis, which led to the improvement of the patient's general condition, but the platelet count was still low and lactate was high. For this reason, bone marrow aspiration/biopsy was performed, and metastatic bone marrow involvement was observed. The result of the CT scan was the presence of multiple sclerotic and lytic lesions in the aorta along with para-aortic lymphadenopathy. Following the hematoma, endoscopy and colonoscopy were requested on the 9th day of hospitalization, and a polyp-shaped lesion with a clot was observed. As shown in Figure 1, signet ring pathology of the stomach was reported. Bone marrow immunohistochemistry also reported an involvement with the origin of the stomach (Figures 2 and 3). Chemotherapy regimen was prescribed with an interval of 2 weeks. In the last follow-up (October 2024), the patient was alive.
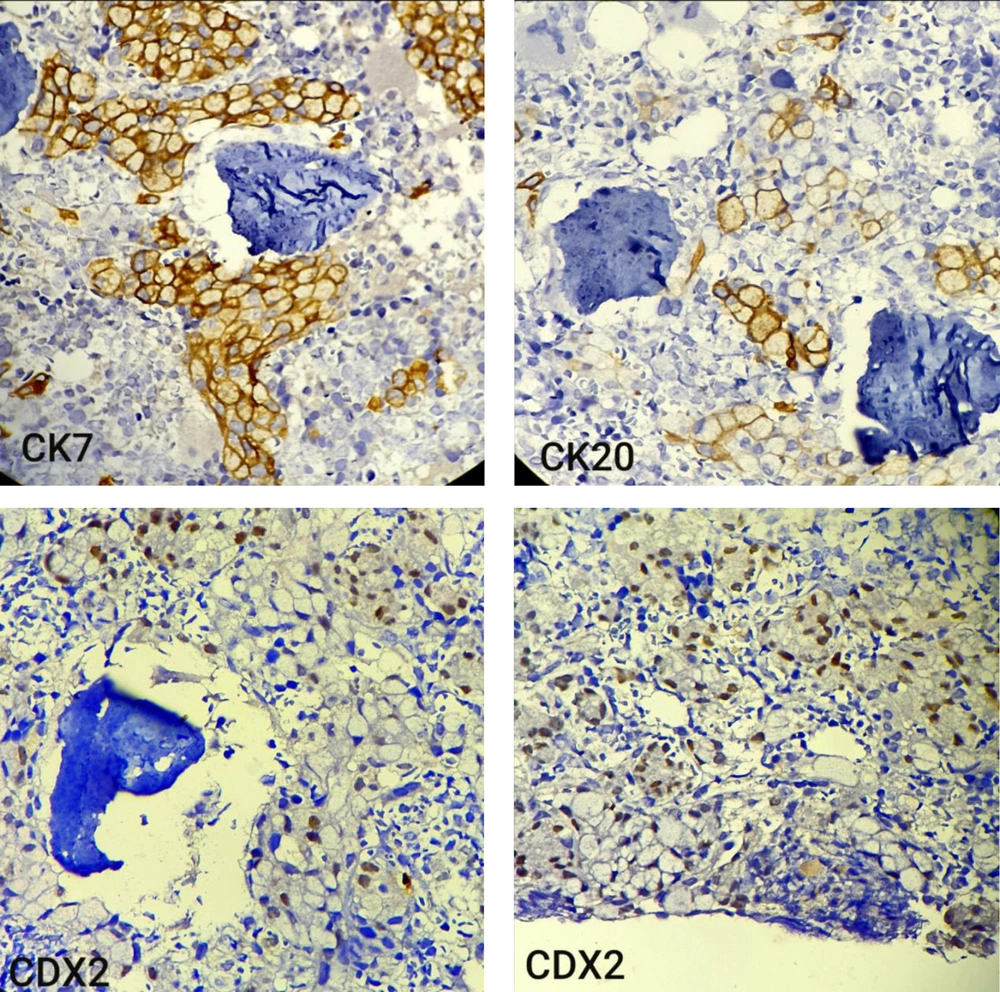
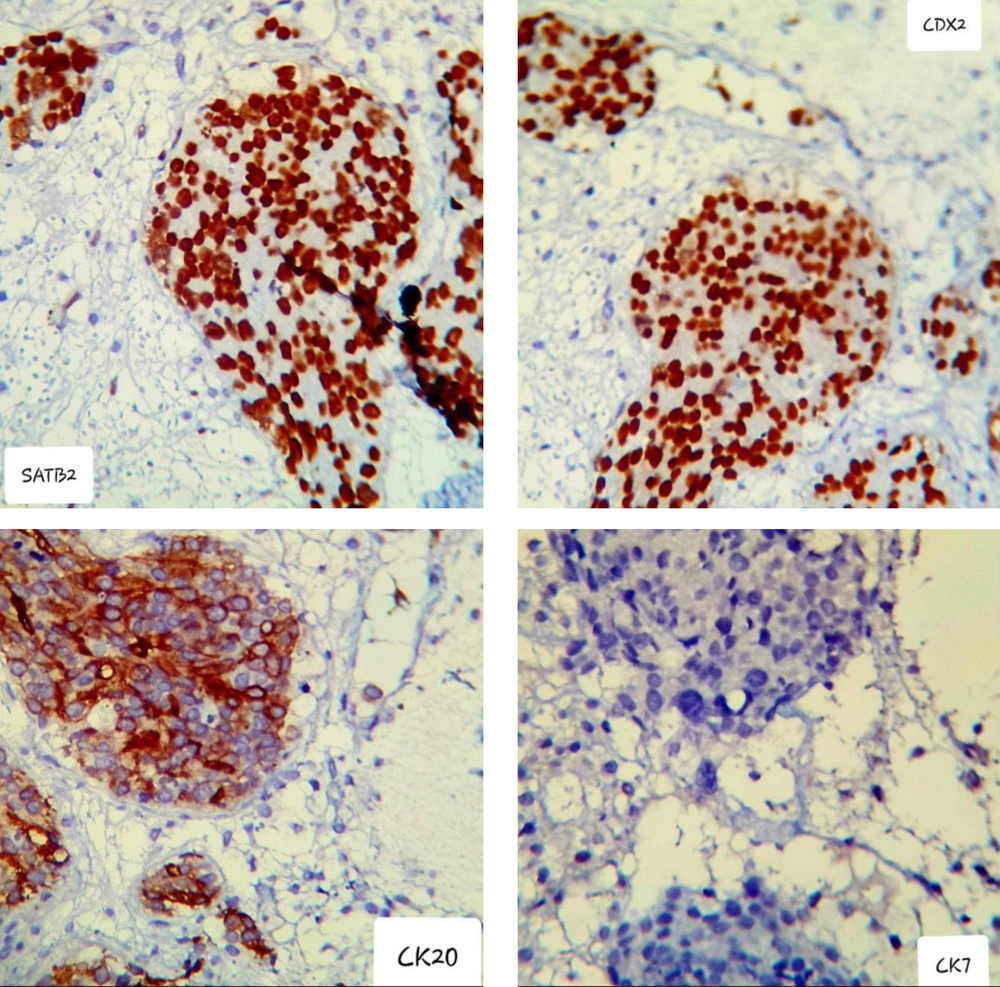
- Number 2: The next patient was a 38-year-old man who had visited the hospital for 3 months with symptoms of lethargy, fever, and chills. These symptoms had been managed with sedation and supportive therapy in previous visits. In the last visit, he mentioned headache, bone pain, and weakness. On examination, he had obvious petechiae on both legs. There were no GI symptoms or weight loss. The platelet count was around 20,000/mcL. On peripheral blood smear, no abnormal WBC lineage or schistocytes were seen. Upon bone marrow aspiration, multiple cluster cells and metastatic involvement were reported (as presented in Figures 4 and 5). CT scan findings included subdural hematoma, increased thickness of the sigmoid, multiple lymph nodes in the same area, and multiple involvement of vertebrae, clavicle, and sternum. The neurology consultation prescribed medication and transferred the patient to the intensive care unit. In the patient's sigmoidoscopy, a mass with a size of 4 cm was observed, and a biopsy revealed adenocarcinoma. The carcinoembryonic antigen (CEA) test was high (28 ng/mL, normal value: 0 to 5 ng/mL). The FOLFOX chemotherapy regimen was prescribed for the patient; unfortunately, he passed away 2 weeks after the first course.
IHC staining slides of BMB of the same case; upper insets show tumor cells are positive for SATB2 and CDX2 (as nuclear expression), indicating a lower GI tract origin. Lower right and left insets show tumor cells are negative for CK7 and positive for CK20, respectively, consistent with the lower GI tract origin of metastasis (IHC, 400X).
3. Discussion
Gastrointestinal cancers often present with a range of common complaints, including localized pain, loss of appetite, digestive issues, and more general symptoms like weight loss and fatigue. It is quite unusual to observe bicytopenia without any specific accompanying symptoms. The incidence of bone metastases, as documented in reports, typically falls within the range of 1% to 10% (10). In a study where a patient presents with a primary diagnosis of bone metastasis from GI tumors, different symptoms can be expected depending on the location and extent of involvement. Fever and pain (15), chronic low back pain (10, 16), back pain and reduced appetite (10), and even dysuria and fecaluria (17).
An interesting study examined the presence of bone micro metastases in patients with colorectal cancer who also had liver metastases with RT-PCR for CK20. Out of 44 patients, nine cases showed positive RT-PCR results, which was associated with worse outcomes (18). Assi et al. reported three patients with colorectal cancer and bone/bone marrow involvement at initial presentation. It is worth noting that two of these patients displayed GI symptoms, while the third did not (10). Bone metastasis in Turkish gastric cancer patients has been estimated at about 2%, which was associated with anemia and thrombocytopenia at presentation, with signet-ring cell type being the prominent pathology (19).
Kwon et al. identified 26 patients with gastric cancer who had confirmed bone marrow infiltration. The analysis of the observed indications for bone marrow biopsy revealed that thrombocytopenia (26.9%) was the most prevalent finding. Following this, bicytopenia was identified as the next most common condition, occurring in 19.2% of cases. In the supportive care group, the median overall survival was recorded at 11 days; in contrast, the palliative chemotherapy group demonstrated a better median overall survival of 121 days. While the overall survival outcomes are unfavorable, these patients still gain benefits from chemotherapy treatment (20).
Bicytopenia is an uncommon initial presentation of GI cancers. It is more frequently associated with hematologic disorders; however, GI malignancies can also present with this hematological abnormality, primarily through mechanisms like bone marrow infiltration, nutritional deficiencies (e.g., vitamin B12 or folate), or chronic disease anemia (21, 22). Early identification and management of GI malignancies presenting with bicytopenia are essential for improving patient prognosis and ensuring optimal therapeutic outcomes.