1. Background
As a fatal incident, myocardial infarction (MI) affects about 1% - 5% of the world population (1, 2). In Iran, 166 cases of MI lead to death on a daily basis (3), which mainly results in many physical and psychological consequences. Besides physical problems reported one year after the event in more than 40% of the patients (4), sudden and unexpected MI can lead to psychiatric disorders like depression (5).
As one of the most likely consequences of MI, depression is observed in 13% - 87% of the patients (6, 7). However, recent studies have shown depression is not just induced by acute heart events, but factors such as female gender, younger age, marital status, smoking, hospital stay, fat intake, functional limitation, social support, negative disease beliefs, history of anxiety and depression, and personality traits including type D and neuroticism are involved in it (8-10).
A wide range of studies have stated the role of personality factors in the incidence of cardiovascular diseases and MI (11-13), but few studies have compared the short and long forms of a personality model such as the five-factor model. The original questionnaire for measuring the five major personality factors has 240 items and its short form has 60 items (14, 15). Recently, a shorter form of this inventory has been standardized with 10 items for research purposes (16). Patients are often tired with long forms with many items and avoid answering accurately. Thus, it is often advisable to use shorter standard tools for evaluating the status of patients with acute diseases (17, 18).
2. Objectives
The present study was therefore conducted to compare 10-item and 60-item big five inventories in explaining the symptoms of depression in patients with MI.
3. Methods
3.1. Study Design and Participants
The study population in this cross-sectional study comprised all patients with MI admitted to Imam Ali (AS) Hospital in Kermanshah (Iran) during April-September 2018. The participants entered the study using consecutive sampling. During the mentioned time, 293 patients with MI were admitted to the hospital: 38 were excluded due to failure to meet the inclusion criteria and 4 due to their unwillingness to participate in the study. The inclusion criteria were a definitive diagnosis of MI by an experienced cardiologist, age range of 18 - 80 years, having at least elementary education, and willingness to participate in the study. The questionnaires with more than 20% missing answers were excluded. Finally, 250 questionnaires were analyzed. After the initial screening of the patients by the research team, the eligible patients were identified. After providing the necessary guarantees to patients for the confidentiality of their identity, their written consent was obtained. Then, the patients completed the questionnaires in the presence of the questioner.
3.2. Data Collection
The research team questioner went to the admissions ward of the hospital and identified the target population on a daily basis and gave them the questionnaires. A brief face-to-face interview was first performed with each patient to establish a therapeutic relationship and obtain the written consent from patients to participate in the study. Then, the questioner briefed the patients on how to respond to the questions. Demographic data and medical records of patients, such as age and gender, education, occupation, marital status, smoking, hypertension, hyperlipidemia, diabetes, history of MI, and family history of heart diseases reported by patients were recorded by the questioner in research forms. Then, this self-reported information was matched with the medical records of patients completed by the cardiologist and incorrect information was corrected. After questionnaires were completed by the subjects, they were collected individually and in the presence of the researcher. Finally, the data was recorded and analyzed in SPSS 20. In the initial interview with patients, the researchers explained the nature of the work to them and asked them to participate in the study to observe ethical considerations. They were then asked to sign a written consent, and complete the questionnaires. Moreover, the patients were assured that their information would remain confidential.
3.3. Tools
3.3.1. The 60-Item NEO-FFI
The original NEO form was developed to evaluate the main five personality factors by Costa and McCrae in 1989, and then repeatedly revised. The 60-item form of this scale was designed in 1992. The inventory is based on five major personality factors of neuroticism, extraversion, openness, conscientiousness, and agreeableness. Twelve items are designed for each of the 5 personality factors. The responses are graded as a 5-point Likert scale from totally disagree to totally agree. In the Iranian population, Cronbach’s alpha of this test for subscales is from 0.39 to 0.83, and its concurrent validity with Eysenck’s questionnaire is from 0.47 to 0.68 (19).
3.3.2. The 10-Item BFI-SV
This questionnaire evaluates the five big personality factors through ten items. The original designers of the questionnaire selected the questions with the help of consensus of experts and empirical analyses to reach the main traits (16). In the 10-item scale, each big factor is measured by two items. Scoring is based on a 5-point Likert scale from totally disagree = 1 to totally agree = 5. This tool has acceptable reliability, convergent validity and divergent validity (16). In Iran, Cronbach’s alpha has been reported as appropriate for all factors and the whole scale (0.60 - 0.69) (20).
3.3.3. Depression Anxiety Stress Scale (DASS)
This 21-item scale was developed by Lovibond and Lovibond in 1995 (21). The tool measures three subscales of depression, anxiety, and stress (7 items for each). The answers to these items are never, low, high, very high. Cronbach’s alpha was reported as acceptable for subscales of depression (0.81), anxiety (0.73), and stress (0.81). In Iran, Cronbach’s alpha was reported as acceptable for depression (0.70), anxiety (0.66), and stress (0.76). Moreover, the questionnaire was well correlated with Beck Anxiety and Depression Inventory (22). Only the depression subscale was used in the study.
3.4. Data Analysis
First, descriptive information related to demographic factors, disease risk factors, and personality traits and depression was reported. Then, non-violations of the assumptions of linear regression such as normality, non-collinearity in predictive variables, and the existence of a significant correlation between predictor variables were examined (23). After confirming the assumptions, to examine the effective personality variables in depression symptoms and determine the exact contribution of each of the variables, the data was analyzed using descriptive statistics (mean and standard deviation), Pearson correlation coefficient and multiple linear regression analysis (concurrent method) in SPSS 20. Two separate regression models were designed: In the first model, evaluated personality traits were entered into the model with a questionnaire of 10 items for predicting depression. In the second model, personality traits assessed with the 60-item questionnaire were inserted into the model. All of the predicting personality factors entered the model simultaneously. All tests were of two domains and were significant at 0.05 levels.
4. Results
The mean age of 250 patients with MI was 11.1 ± 62.1 years. Table 1 shows the status of demographic factors and risk factors for MI among women and men. As seen, there is a significant difference in terms of education (P < 0.001), occupation (P < 0.001), and marital status (P < 0.001), history of smoking (P < 0.001), hyperlipidemia (P = 0.039), and hypertension (P = 0.002) between men and women.
| Factor | Total (n = 250) | Female (n = 77) | Male (n = 173) | P Value | |
|---|---|---|---|---|---|
| Education | 22.702 | 0.001 | |||
| Under diploma | 164 (65.6) | 67 (87) | 97 (56.1) | ||
| Diploma | 46 (18.4) | 6 (7.8) | 40 (23.1) | ||
| Academic | 40 (16) | 4 (5.2) | 36 (20.8) | ||
| Job | 194.134 | 0.001 | |||
| Employee | 38 (15.2) | 4 (5.2) | 34 (19.7) | ||
| Self-employed | 113 (45.2) | 3 (3.9) | 110 (63.6) | ||
| Housekeeper | 68 (27.2) | 66 (85.7) | 2 (1.2) | ||
| Retired | 30 (12) | 4 (5.2) | 26 (15.6) | ||
| Marital status | 44.406 | 0.001 | |||
| Single | 12 (4.8) | 5 (6.5) | 7 (4) | ||
| Marriage | 213 (85.2) | 50 (64.9) | 163 (94.2) | ||
| Widow/separated | 25 (10) | 22 (28.6) | 3 (1.7) | ||
| Smoking | 113 (45.2) | 10 (13) | 103 (59.5) | 48.821 | 0.001 |
| MI history | 51 (20.4) | 11 (14.3) | 40 (23.1) | 2.562 | 0.109 |
| Family history | 101 (40.4) | 34 (44.2) | 67 (38.7) | 0.652 | 0.419 |
| HLP | 75 (30) | 30 (39) | 45 (26) | 4.255 | 0.039 |
| HTN | 116 (46.4) | 69 (61) | 47 (39.9) | 9.588 | 0.002 |
| DM | 39 (15.6) | 16 (20.8) | 23 (13.3) | 2.267 | 0.132 |
aValues are expressed as No. (%).
Table 2 shows the results of Pearson correlation coefficient between personality traits and depression. As seen, there is a significant inverse relationship between personality factors of extraversion (r = -0.235; P < 0.001), agreeableness (r = -0.202; P < 0.001), and conscientiousness (r = -0.209; P < 0.001) in 10-item questionnaire with depression. In 60-item form, there is a significant negative relationship between neuroticism (r = -0.154; P = 0.007) and agreeableness (r = -0.117; P = 0.032) with depression, but there is a significant direct relation between extraversion and depression (r = 0.141; P = 0.013).
| Personality Factors | Results | Depression | |
|---|---|---|---|
| r | P Value | ||
| Neuroticism-10 | 6.82 ± 1.48 | - 0.047 | 0.230 |
| Extraversion-10 | 8.60 ± 1.55 | - 0.235 | 0.001 |
| Openness-10 | 6.67 ± 2.00 | - 0.093 | 0.072 |
| Agreeableness-10 | 8.27 ± 1.42 | - 0.202 | 0.001 |
| Conscientiousness-10 | 8.69 ± 1.56 | - 0.209 | 0.001 |
| Neuroticism-60 | 27.32 ± 4.78 | - 0.154 | 0.007 |
| Extraversion-60 | 18.32 ± 4.81 | 0.141 | 0.013 |
| Openness-60 | 22.86 ± 3.59 | 0.024 | 0.355 |
| Agreeableness-60 | 23.85 ± 4.44 | - 0.117 | 0.032 |
| Conscientiousness-60 | 20.30 ± 2.14 | - 0.003 | 0.482 |
| Depression | 1.42 ± 2.14 | ||
aValues are expressed as mean ± SD.
Table 3 shows the results of multiple regression analysis for predicting depression using 10-item form of the questionnaire. As seen, none of the components alone can predict symptoms of depression (P > 0.05). However, all personality factors can significantly affect 6.7% of the variance of depression score (F = 3.519, P = 0.004).
| Personality Factors | B | β | t | P Value |
|---|---|---|---|---|
| Neuroticism-10 | 0.020 | 0.014 | 0.212 | 0.832 |
| Extraversion-10 | - 0.184 | - 0.134 | - 1.455 | 0.147 |
| Openness-10 | - 0.019 | - 0.018 | - 0.271 | 0.786 |
| Agreeableness-10 | - 0.152 | - 0.101 | - 1.379 | 0.169 |
| Conscientiousness-10 | - 0.096 | - 0.070 | - 0.799 | 0.425 |
aSummary of the model for depression; R = 0.259; R2 = 0.067; F = 3.519; P = 0.004.
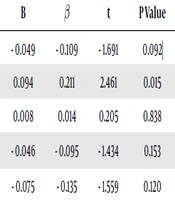
Table 4 shows the results of multiple regression analysis for predicting depression using the 60-item form. As seen, extraversion alone can significantly predict the symptoms of depression (P = 0.015). Overall, the total personality factors can significantly predict 5.8% of the variance of depression score (F = 3.026, P = 0.011).
| Personality Factors | B | β | t | P Value |
|---|---|---|---|---|
| Neuroticism-60 | - 0.049 | - 0.109 | - 1.691 | 0.092 |
| Extraversion-60 | 0.094 | 0.211 | 2.461 | 0.015 |
| Openness-60 | 0.008 | 0.014 | 0.205 | 0.838 |
| Agreeableness-60 | - 0.046 | - 0.095 | - 1.434 | 0.153 |
| Conscientiousness-60 | - 0.075 | - 0.135 | - 1.559 | 0.120 |
aSummary of the model for depression; R = 0.242; R2 = 0.058; F = 3.026; P = 0.011.
5. Discussion
The present study was conducted to compare 10-item and 60-item big five inventories in explaining the symptoms of depression in patients with acute MI. The results showed that the 10-item version explains 6.7% and the 60-item questionnaire explains 5.8% of the variance of the depression scores in patients with MI, and that the two tools are not different. If shorter standard tools are designed appropriately, they can be effective in evaluating patients over a shorter time and at a lower cost (24). Furthermore, longer tools do not necessarily cover all dimensions of a variable or factor (25).
Other results showed a significant inverse relationship between personality factors of extraversion, agreeableness, and conscientiousness in the 10-item form of the questionnaire with depression. Consistent with the results of the present study, the results of two studies showed the inverse relationship of extraversion and conscientiousness with depression (26, 27). Another study showed that depressed patients had lower levels of extraversion and conscientiousness compared to healthy controls (28). The study reported an inverse relationship between agreeableness and treatment-resistant depression (28). Probably, the patients with higher positive personality dimensions including extraversion, agreeableness, and conscientiousness create a more effective support system around them according to their characteristics. Moreover, they feel more conscientiousness for their physical and mental health. Thus, they are expected to experience less depression.
Other results showed a significant inverse relationship between neuroticism and conscientiousness in the 60-item form with depression but a significant direct relationship between extraversion and depression. A possible explanation for the relationship between agreeableness and depression was mentioned above. However, contrary to our results, previous studies showed a direct relationship between neuroticism and depression (26-28). However, the results of a study show that the relationship between these two variables is affected by the onset of depression. In other words, there is a negative relationship between depressions with late onset compared to early onset of depression with depression (26). The patients in our study are generally over 60 and are likely to experience late depression symptoms. Therefore, an inverse relationship between neuroticism and depression is expected.
Among the limitations of the study are that only patients with MI were included and other patients with coronary heart diseases, heart failure, heart valve diseases, and patients with invasive interventions including CABG were excluded. It is recommended that in future studies, all groups of patients with heart diseases be enrolled into the study. Non-randomized sampling was another limitation of the current study. The tool for measuring depression (one of the DASS subscales) in the present study may be more inefficient than structured interviews such as SCID-I. Using specific tools to measure depression symptoms should be considered in future studies. Moreover, the patients in our study were limited to a specialized cardiac hospital in western Iran. It appears that selecting the patients from different health centers from all over the country and increasing the sample size in future studies may help obtain more accurate results.
5.1. Conclusions
The 10-item version of NEO can probably explain the symptoms of depression in patients with MI as accurately as the 60-item version can. As using shorter tools and questionnaires in research activities is cost-effective and can increase the level of cooperation in patients with acute physical illnesses, the researchers in this field can use the 10-item version in future studies to assess personality traits of patients with MI.