1. Background
Tobacco-free restaurant in Malaysia was implemented after the Control of Tobacco Product Regulation amendment on 24 December 2018. The new amendment in this legislation is amended in regulation two by substituting the definition of “air-conditioned eating place” with a new definition. The new meaning for “eating place” means “any premises, whether inside or outside building, where food is prepared, served or sold and included any room or area on a ship or train, or any area on the vehicle, or any area within a radius of three meters from any table or chair which is placed on preparing, serving or selling food” (1). The other amendments of regulation 11 is substituting the paragraph (d) “in any eating place or the air-conditioned shop” (1). These regulations came into effect on 1 January 2019.
In Sarawak, the implementation of smoke-free restaurants started on 1 March 2019. The State Local Government and Housing Minister informed that the Sarawak Cabinet decided to enforce this regulation on Thursday, 24 January 2019, for the health of the public. The Minister reported that the State Cabinet also agreed that the first six months from 1 March would be an educational enforcement period. The federal government’s smoking ban at all restaurants and food outlets in Peninsular Malaysia came into effect on 1 January (2). Similar to the federal law, offenders found smoking at banned places in Sarawak can be fined up to RM10,000 or jailed for a maximum of two years. Eatery owners who fail to display “No smoking” signs can be fined up to RM3,000 or jailed up to 6 months (1). The amendment of the tobacco product regulation by the Ministry of Health is a vital step to be implemented to extend the protection from the exposure of SHS besides improving the air quality and enhancing the workers’ health (3, 4). It also gives awareness to smokers to quit smoking and prevent the young generation from smoking (5, 6).
Globally, the effect of direct tobacco users is more than 7 million deaths, while the non-smoker exposed to SHS is estimated at 1.2 million (7). The harmful effect of SHS exposure has resulted in the burden of disease in children and adult non-smokers (8). Restaurants and bars have the highest SHS concentration (9, 10). In Malaysia, the prevalence of exposure to SHS in an indoor workplace is approximately 39.8%. Moreover, about 84.9% were exposed to SHS in cafes or coffee shops and 71% in restaurants. This percentage can lead to a higher incidence of SHS-related illness (11). A study from GATS Malaysia in 2011 showed that restaurant employees are more vulnerable to being exposed to SHS-related diseases (12). Therefore, this indicates that implementing policies in eating places is a precise action by the government. Various parties need to collaborate with the Ministry of Health to increase public knowledge, attitude, and support towards the success of the smoke-free policy in the eating-places.
SHS-related illness is an increasing public health burden and has a negative impact on all ages, from the womb to the tomb (12). The effects of SHS exposure cause health, environmental, and economic problems to individuals, families, and communities. This includes direct or indirect medical costs. However, there is a remarkable gap between tobacco-free restaurants’ poor practices and the support towards the policy among the community. This could be explained in several ways with one of them is that the offenders thought that protecting people from harmful exposure to SHS was an issue that the government has to tackle, or they were unaware of the punishments for breaking the Tobacco Control Act laws. It is also likely that they did not give serious thought to the potential legal ramifications of violating the smoke-free rule until they showed some kind of support (13). Another explanation may be the owner or management are concerned about the potential decline in their businesses (14, 15). The significance of this study could identify the associated factors among the respondents to support and practice a smoke-free policy in all eating places or restaurants. This could help the government to focus on incrementing supportive awareness leading to increased compliance with a smoke-free policy. This study’s main aim is to determine the impact of perceived knowledge on tobacco control law, the health and environmental effect of SHS, and attitude to support and practice smoke-free eating-places.
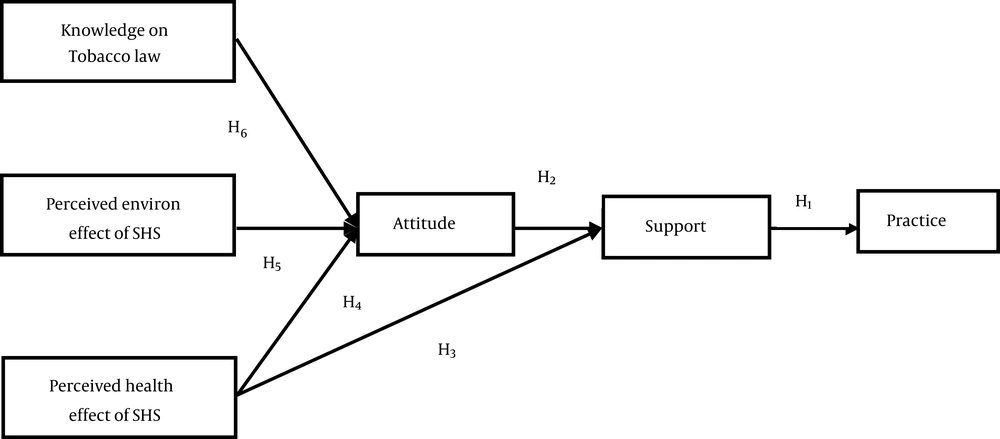
1.1. Conceptual Framework and Hypothesis
The practice of tobacco-free restaurants is influenced by various factors such as their knowledge of smoke-free legislation, knowledge of the dangers of exposure to passive cigarettes, smoking status, personal characteristics, attitudes, and support towards the policy (11, 13, 16). For this study, there are several selected variables, including knowledge on tobacco control law, perceived effects of SHS on health and environment, and attitude and support towards smoke-free eating-places. The level of practice of smoke-free legislation in restaurants is the dependent variable. The theory of planned behaviors (TPB) is a theory of individual health promotion. Theory of planned behaviors framework was used in this study to understand tobacco-free policy compliance behaviors. Behavioral intentions as variables, such as knowledge of the law, are perceived on the effect on the health and environment capable of influencing attitude. Attitude is the most typical characteristic that has always been discussed in research to determine behavior patterns. The conceptualisation of perceived behavioral control as a core component of the TPB model reflects the understanding of people’s ability to regulate their behavior (17).
For the tobacco-free restaurant practices after implementing the policy, we need to identify factors that can increase the level of compliance. In line with other tobacco-related TPBs, the findings suggest that TPB is a useful tool for understanding tobacco-free policy enforcement behaviors. TBP is always used in addiction problems such as quitting tobacco use. However, the compliance patterns, a feature of addiction, are increasingly affected by social beliefs, cultural norms, and behavioral regulation. Regarding compliance with smoke-free policies, the results clearly show that the authorities’ continuous and practical enforcement assessments, perceptions of social expectations, and willingness to comply are the critical factors in understanding tobacco-free policies (Figure 1) (18).
The potential hypothesis to be tested in this research is:
H1: Supporting tobacco-free eating places has a direct impact on the practice of tobacco-free eating places.
H2: Perceived attitude towards tobacco-free restaurants has a direct impact on supporting tobacco-free eating places.
H3 and H4: Perceived health effects of secondhand smoking directly and indirectly impacted supporting tobacco-free eating places.
H5: Perceived environmental effect of secondhand smoking has an indirect effect and mediating effect on supporting tobacco-free eating places.
H7: Knowledge of tobacco-free law has a mediating effect on practicing tobacco-free eating places.
2. Methods
2.1. The Setting, Population, and Sampling
This cross-sectional study was conducted in 5 out of 11 administrative divisions of Sarawak, in East Malaysia that is located in Borneo island. The population of Sarawak was estimated at 2.90 million in 2020, with a large ethnic diversity including Iban, Chinese, Malay, Bidayuh, Melanau, Kenyah, Kayan, Penan, and others. A multi-stage cluster sampling method was used to select the eating places. Firstly, we listed out the township areas in the district under the division. In each district, we randomly select 3 township areas. In the second stage, we listed the eating places in the selected township. In the third stage, we randomly selected 10% of the eating places. In the final stage, one respondent from each eating place was selected randomly. The inclusion criteria for the selection are a participant who worked in their respective eating place irrespective of gender and type of work. However, we did not select the customer of the same eating places. A total of 849 eating places were collected with 259 customers and 590 restaurant personnel.
2.2. Data Collection Instruments and Measurement Procedure
Data were collected by face-to-face interview using a validated structured questionnaire. The questionnaire was prepared in English followed by content analysis with support from an external expert. Then, a back-to-back translation was done using Bahasa Melayu, the local language. The questionnaire was administered in Bahasa Melayu. The instruments had several components with measurement of perceived knowledge on the tobacco-free eating place, tobacco-free policy, environmental and health effects of secondhand smoking, attitude and supporting tobacco-free eating place, and the current tobacco-free eating place.
The health effect of SHS was measured by asking agreement or disagreement with seven-point Likert scale questions. Eleven items of the five-point Likert scale questions were used to measure the perceived knowledge of tobacco-free policy or law supporting eating places. The answer options were ‘most unlikely’, ‘unlikely’, ‘neutral’, ‘likely’, and ‘most likely’. There were 8-item questions included in this domain, however, 9-item questions were used to assess the environmental effect of SHS. The answer options were ‘strongly disagree’, ‘somewhat disagree’, ‘slightly disagree’, ‘neither agree nor disagree’, ‘slightly agree’, ‘somewhat agree’, and ‘strongly agree’.
The attitude toward tobacco-free eating places was measured by asking the 15-item question with a 7-point Likert scale. The answer options were ‘strongly disagree’ to ‘strongly agree’. A higher score indicated a high attitude towards tobacco-free eating places.
The supporting tobacco-free eating place was measured by asking 6-point Likert’s scale questions in which the options are ‘completely not support’, ‘mostly not support’, ‘slightly not support’, ‘slightly support’, ‘mostly support’, and ‘completely support’. The higher score indicated more support for tobacco-free eating places.
The current practice of tobacco-free eating places was measured by asking two questions that are ‘Do you discourage anyone from smoking in the restaurant?’ and ‘Is smoking is allowed in this restaurant?’
2.3. Data Entry and Analysis
Data entry was done using Microsoft Excel with a validation check. All data were checked thoroughly and cleaned before analysis. Missing data were imputed using multiple imputations. The descriptive and exploratory data analysis was done using IBM SPSS version 27.0 (19). The descriptive analysis is presented in a table with frequencies, mean, standard deviation, minimum and maximum values.
We conducted a pilot study to determine the acceptability, feasibility, and comprehensibility of the instrument. All items of each domain remained during data collection. Cronbach alpha was assessed for the internal consistency of the items within each domain (20). However, before structural path analysis, we measured the measurement model in convergent and discriminant validity. Convergent validity is related to construct validity, which states that tests having the same or similar constructs should be highly correlated (21). For convergent validity, we examined the item loading of more than 0.5 (22), Cronbach alpha with an acceptable level of ≥ 0.60 (23), and composite reliability with an acceptable level of ≥ 0.60 (22). For discriminant validity, we examined three criteria that are viz. (1) Fornell-Larcker criterion, (2) Cross-loadings, and (3) heterotrait-monotrait (HTMT) ratio. The Fornell-Larcker criterion is the square root of the Average Variance Extracted (AVE). It should be higher than the correlation of the construct with all other constructs in the structural model (24). Table 1 shows that the diagonal values are the square root of the AVE. Off-diagonal elements are the correlations among the constructs. The diagonal elements should be larger than the off-diagonal elements. The cross-loading in each construct should be greater than the corresponding other items. The third criterion is the multitrait-multimethod matrix to assess discriminant validity in the form of heterotrait-monotrait (HTMT) ratio of correlations (25). A value that is greater than the HTMT0.85 of 0.85 (26) or HTMT0.90 of 0.90 (27) shows that the discriminant validity is not established.
| K_Law | Env_Res | H_SHS | Attitude | Support | Practice | |
|---|---|---|---|---|---|---|
| Fornell-Larcker Criterion | ||||||
| K_Law | 0.685 b | |||||
| Env_Res | 0.219 | 0.851 b | ||||
| H_SHS | 0.088 | 0.263 | 0.805 b | |||
| Attitude | 0.217 | 0.695 | 0.190 | 0.869 b | ||
| Support | 0.198 | 0.591 | 0.462 | 0.692 | 0.747 b | |
| practice | 0.134 | 0.153 | 0.222 | 0.177 | 0.315 | 0.861 b |
| Cross-loading | ||||||
| B2 | 0.649 b | 0.189 | 0.062 | 0.145 | 0.121 | 0.138 |
| B3 | 0.670 b | 0.098 | -0.021 | 0.152 | 0.073 | 0.060 |
| B4 | 0.756 b | 0.170 | 0.094 | 0.147 | 0.196 | 0.100 |
| B8 | 0.746 b | 0.114 | 0.055 | 0.122 | 0.113 | 0.091 |
| B9 | 0.592 b | 0.178 | 0.109 | 0.174 | 0.172 | 0.069 |
| C8 | 0.208 | 0.921 b | 0.218 | 0.632 | 0.542 | 0.167 |
| C9 | 0.222 | 0.885 b | 0.287 | 0.613 | 0.531 | 0.132 |
| C10 | 0.181 | 0.869 b | 0.258 | 0.534 | 0.491 | 0.094 |
| C11 | 0.211 | 0.915 b | 0.210 | 0.661 | 0.565 | 0.157 |
| C16 | 0.104 | 0.627 b | 0.135 | 0.490 | 0.364 | 0.096 |
| C1 | 0.052 | 0.207 | 0.842 b | 0.161 | 0.350 | 0.160 |
| C2 | 0.136 | 0.370 | 0.744 b | 0.361 | 0.451 | 0.174 |
| C3 | 0.105 | 0.155 | 0.834 b | 0.069 | 0.341 | 0.155 |
| C4 | 0.041 | 0.178 | 0.875 b | 0.094 | 0.356 | 0.241 |
| C5 | 0.085 | 0.153 | 0.661 b | 0.127 | 0.289 | 0.071 |
| C6 | 0.045 | 0.227 | 0.793 b | 0.170 | 0.417 | 0.217 |
| C7 | 0.028 | 0.184 | 0.864 b | 0.085 | 0.389 | 0.230 |
| D1 | 0.155 | 0.621 | 0.165 | 0.820 b | 0.517 | 0.096 |
| D4 | 0.199 | 0.650 | 0.089 | 0.921 b | 0.567 | 0.129 |
| D5 | 0.186 | 0.589 | 0.134 | 0.876 b | 0.609 | 0.172 |
| D6 | 0.178 | 0.585 | 0.177 | 0.856 b | 0.617 | 0.170 |
| D7 | 0.225 | 0.672 | 0.110 | 0.947 b | 0.602 | 0.152 |
| D8 | 0.180 | 0.663 | 0.132 | 0.940 b | 0.593 | 0.143 |
| D9 | 0.194 | 0.662 | 0.105 | 0.931 b | 0.601 | 0.125 |
| D10 | 0.195 | 0.590 | 0.124 | 0.905 b | 0.610 | 0.179 |
| D11 | 0.211 | 0.664 | 0.097 | 0.950 b | 0.620 | 0.151 |
| D12 | 0.193 | 0.533 | 0.275 | 0.754 b | 0.681 | 0.222 |
| D13 | 0.131 | 0.516 | 0.196 | 0.797 b | 0.575 | 0.102 |
| D14 | 0.165 | 0.544 | 0.202 | 0.837 b | 0.590 | 0.166 |
| D15 | 0.217 | 0.503 | 0.365 | 0.657 b | 0.607 | 0.194 |
| D16 | 0.198 | 0.623 | 0.133 | 0.925 b | 0.593 | 0.136 |
| E1 | 0.151 | 0.461 | 0.437 | 0.532 | 0.788 b | 0.327 |
| E2 | 0.186 | 0.683 | 0.224 | 0.869 | 0.758 b | 0.187 |
| E3 | 0.139 | 0.491 | 0.448 | 0.532 | 0.806 b | 0.210 |
| E4 | 0.121 | 0.613 | 0.254 | 0.740 | 0.797 b | 0.126 |
| E5 | 0.089 | 0.283 | 0.330 | 0.338 | 0.737 b | 0.281 |
| E6 | 0.124 | 0.253 | 0.331 | 0.268 | 0.672 b | 0.303 |
| E7 | 0.188 | 0.367 | 0.360 | 0.389 | 0.755 b | 0.193 |
| E8 | 0.181 | 0.373 | 0.367 | 0.455 | 0.647 b | 0.254 |
| F1_R | 0.062 | 0.020 | 0.186 | 0.057 | 0.225 | 0.861 b |
| F2_R | 0.169 | 0.244 | 0.198 | 0.247 | 0.319 | 0.861 b |
| Hetero-Trait and Mono-Trait Ratio | ||||||
| Knowledge | ||||||
| Env_effect | 0.274 | |||||
| Health_SHS | 0.146 | 0.291 | ||||
| Attitude | 0.260 | 0.742 | 0.206 | |||
| Support | 0.249 | 0.663 | 0.515 | 0.745 | ||
| Practice | 0.197 | 0.200 | 0.289 | 0.225 | 0.415 | |
a HTMT ratio (good if < 0.90, best if < 0.85).
b Diagonal values are the square root of the AVE.
Finally, a structural path analysis was done to examine the relationship between tobacco-free eating places and knowledge, attitude, and supporting tobacco-free eating places. The structural path analysis was performed using WarpPLS 7.0 stable version (28). However, the descriptive analysis was done by Statistical Package for the Social Sciences version 27 (19). A P-value of ≤ 0.05 is considered statistically significant.
2.4. Ethical Issues
The study was initiated after receiving ethics and administrative approval from the Faculty of Medicine and Health Sciences. Before the interview, informed consent was obtained from the participants. The participants were assured of anonymity and data confidentiality.
3. Results
3.1. Characteristics of the Respondents
The mean age of the respondents was 30.1 years with a standard deviation of 11.59 years. Two-fifths (58.1%) were female, and the rest were male. The highest percentage of the respondents were Malays (60.7%), followed by Iban (15.2%). More than half of the respondents had a secondary education (55.5%) followed by a diploma (17.2%). Two-fifths (38.6%) were married. The median family size was 5.0. At least one family member is a smoker. The median family income was MYR 1047.58, with a minimum of MYR 180 and a maximum of MYR 15000 (Table 2).
| Variables | No. (%) | Statistics | |||
|---|---|---|---|---|---|
| Mean ± SD | Median | Min | Max | ||
| Category | |||||
| Owner | 198 (23.3) | ||||
| Workers | 392 (46.2) | ||||
| Customers | 259 (30.5) | ||||
| Age (y) | 30.1 ± 11.59 | - | 12.0 | 79.0 | |
| < 20 | 113 (13.3) | ||||
| 20 - 29 | 399 (47.0) | ||||
| 30 - 39 | 161 (19.0) | ||||
| 40 - 49 | 101 (11.9) | ||||
| ≥ 50 | 75 (8.8) | ||||
| Gender | |||||
| Male | 356 (41.9) | ||||
| Female | 493 (58.1) | ||||
| Ethnicity | |||||
| Malay | 515 (60.7) | ||||
| Chinese | 117 (13.8) | ||||
| Iban | 129 (15.2) | ||||
| Others (Bidayuh, Indian etc) | 88 (10.4) | ||||
| Religion | |||||
| Islam | 545 (64.2) | ||||
| Christianity | 251 (29.6) | ||||
| Others (Hinduism, Buddhism etc.) | 53 (6.2) | ||||
| Level of education | |||||
| Primary and below | 113 (13.3) | ||||
| Secondary | 471 (55.5) | ||||
| University | 119 (14.0) | ||||
| Diploma | 146 (17.2) | ||||
| Marital status | |||||
| Married | 328 (38.6) | ||||
| Single | 521 (61.4) | ||||
| Family size | 5.72 ± 2.19 | 5.0 | 1 | 14 | |
| 1 - 2 | 35 (4.1) | ||||
| 3 - 4 | 249 (29.3) | ||||
| 5 - 6 | 314 (37.0) | ||||
| ≥ 7 | 251 (29.6) | ||||
| Number of smokers | 1.43 ± 1.41 | 1.0 | 0 | 8 | |
| 0 | 178 (21.0) | ||||
| 1 | 309 (36.4) | ||||
| 2 | 154 (18.1) | ||||
| ≥ 3 | 208 (24.5) | ||||
| Monthly income (MYR) | 1951.41 ± 1834.97 | 1047.58 | 180 | 15000 | |
| < 1000 | 189 (22.3) | ||||
| 1000 - 1999 | 230 (27.1) | ||||
| 2000 - 2999 | 153 (18.0) | ||||
| 3000 - 3999 | 115 (13.5) | ||||
| 4000 - 4999 | 162 (19.1) | ||||
| Food handling training | |||||
| Yes | 361 (61.2) | ||||
| No | 229 (38.8) | ||||
3.2. Convergent Validity and Discriminant Validity
Tables 1 and 3 illustrated the convergent and discriminant validity. Our analysis revealed that the loadings were all higher than 0.70, the composite reliabilities were higher than 0.70, and the AVE of the constructs was also higher than 0.50. Accordingly, the convergent validity of the constructs has been established (22, 29).
| Domains and Items | Loading | α | Dijkstra-R | CR | AVE | VIF |
|---|---|---|---|---|---|---|
| Knowledge of Tobacco-free eating place | 0.714 | 0.709 | 0.815 | 0.470 | 1.070 | |
| B2 | 0.649 | |||||
| B3 | 0.670 | |||||
| B4 | 0.756 | |||||
| B8 | 0.746 | |||||
| B9 | 0.592 | |||||
| Environmental effect of second-hand smoking | 0.899 | 0.914 | 0.928 | 0.724 | 2.061 | |
| C8 | 0.921 | |||||
| C9 | 0.885 | |||||
| C10 | 0.869 | |||||
| C11 | 0.915 | |||||
| C16 | 0.627 | |||||
| Health effect of secondhand smoking | 0.907 | 0.942 | 0.927 | 0.648 | 1.384 | |
| C1 | 0.842 | |||||
| C2 | 0.744 | |||||
| C3 | 0.834 | |||||
| C4 | 0.875 | |||||
| C5 | 0.661 | |||||
| C6 | 0.793 | |||||
| C7 | 0.864 | |||||
| Attitude toward the tobacco-free eating place | 0.974 | 0.975 | 0.977 | 0.756 | 2.266 | |
| D1 | 0.820 | |||||
| D4 | 0.921 | |||||
| D5 | 0.876 | |||||
| D6 | 0.856 | |||||
| D7 | 0.947 | |||||
| D8 | 0.940 | |||||
| D9 | 0.931 | |||||
| D10 | 0.905 | |||||
| D11 | 0.950 | |||||
| D12 | 0.754 | |||||
| D13 | 0.797 | |||||
| D14 | 0.837 | |||||
| D15 | 0.657 | |||||
| D16 | 0.925 | |||||
| Supporting tobacco-free eating place | 0.886 | 0.895 | 0.910 | 0.558 | 2.619 | |
| E1 | 0.788 | |||||
| E2 | 0.758 | |||||
| E3 | 0.806 | |||||
| E4 | 0.797 | |||||
| E5 | 0.737 | |||||
| E6 | 0.672 | |||||
| E7 | 0.755 | |||||
| E8 | 0.647 | |||||
| Practising tobacco-free eating place | 0.652 | 0.727 | 0.852 | 0.742 | 1.131 | |
| F1_R | 0.861 | |||||
| F2_R | 0.861 |
Abbreviations: α, Cronbach’s alpha; CR, composite reliability; AVE, Average Variance Extracted; VIF, variance inflation factor; Dijkstra’s reliability.
Regarding discriminant validity, the Fornell-Larcker criterion (24) suggests that the square root of AVE is higher than the correlation. Table 1 shows the diagonal values are the square root of the AVE. The off-diagonal values are the correlations among the constructs. According to the criterion, the diagonal values should be larger than the off-diagonal elements. The HTMT value is higher than HTMT0.85 of 0.85 (26) or HTMT0.90 value of 0.90 indicates that the discriminant validity is not established (27). Our results showed that the HTMT values are less than the cut of value. This indicated that the discriminant validity had been established. There is no multicollinearity problem among the domains. It has no overlapping items in each domain construct.
3.3. Model Fit and Quality Indices
Robust path analysis with a non-linear algorithm, which is bootstrapping resampling method was used for analysis (28). Model fitting and quality indices indicated that the average path coefficient was (APC) = 0.339, (P < 0.001), average R-squared (ARS) = .396, (P < 0.001), average adjusted R-squared (AARS) = 0.391, (P < 00.001), average block VIF (AVIF) = 1.065, and average full collinearity VIF (AFVIF) = 1.816. The standardized root mean squared residual (SRMR) was 0.098, and the standardized mean absolute residual (SMAR) was 0.075. All of the model fitting information indicated a well-fitted model.
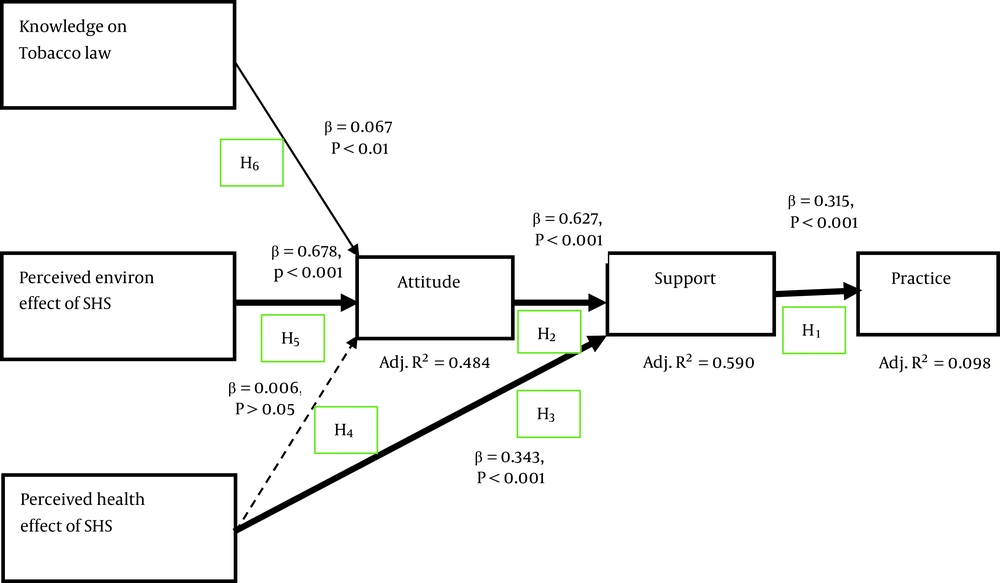
3.3.1. Practicing Tobacco-Free Eating Place
Figure 2 and Table 4 show the results for the structural equation modelling analysis. Consistent with the TPB, the supporting behavior is significantly associated with the practice of tobacco-free eating places (β = 0.315, P < 0.001) with a small effect size (ES = 0.100). This supports our H1.
| Hypothesis | Relationship | Std0. Beta | Std0. Error | ES | R2 Contribution | Q2 | Decision |
|---|---|---|---|---|---|---|---|
| H1 | Support → Practice | 0.315 a | 0.036 | 0.100 b | 0.100 | 0.099 | Supported |
| H2 | Attitude → Support | 0.627 a | 0.022 | 0.433 c | 0.433 | 0.591 | Supported |
| H3 | Health effect of SHS → Support | 0.343 a | 0.033 | 0.158 d | 0.158 | - | Supported |
| H4 | Health effect of SHS → Attitude | 0.006 | 0.029 | 0.001 | 0.001 | 0.487 | Not supported |
| H5 | Environmental effect of SHS → Attitude | 0.678 a | 0.026 | 0.471 c | 0.471 | Supported | |
| H6 | Tobacco control → Attitude | 0.067 e | 0.030 | 0.015 b | 0.015 | Supported |
Abbreviation: ES, Effect size.
a P < 0.001
b Small (0.02)
c Large (0.35)
d Medium (0.15)
e P < 0.01
3.3.2. Supporting Tobacco-Free Eating Place
The analysis on supporting tobacco-free eating places indicates that it directly correlated with the attitude towards tobacco-free eating places (β = 0.627, P <0.001) and also with the perceived health effect of secondhand smoking (β = 0.343, P < 0.001) with moderate effect size (ES = 0.158). However, there is a mediating effect of the perceived health effect of secondhand smoking (β = 0.006, P > 0.05) to supporting tobacco-free eating places through with attitude towards the tobacco-free eating place. This supports our H2 of the direct impact of attitude to supporting tobacco-free eating places and H3 of health effect smoking to support tobacco-free eating places.
3.3.3. Attitude Towards the Tobacco-Free Eating Place
In line with the TPB, three background variables were included in the structural model, viz. perceived health effect of secondhand smoking, perceived environmental effect of secondhand smoking, and perceived knowledge of tobacco-free law and policy to attitude towards tobacco-free eating places. The analysis revealed that the perceived health effect of secondhand smoking had no impact on attitude towards tobacco-free eating places (β = 0.006, P > 0.05) hence not supporting hypothesis 4. However, the perceived environmental effect of secondhand smoking had a strong impact (β = 0.678, P < 0.001) and a weak impact of knowledge on tobacco law or policy (β = 0.067, P < 0.01) on attitude towards tobacco-free eating places, which support our hypothesis 5 and 6.
3.4. The Indirect and Total Effect
Analysis of the indirect and total effect of different parameters on practising tobacco-free eating places is illustrated in Table 5. For a straightforward interpretation of the mediation effect, the variance accounted for (VAF) was calculated. Analysis indicated that supporting and attitude towards tobacco-free eating places had a significant impact on practising tobacco-free eating places with a total effect of 0.198 (P < 0.001). According to Hair et al. (22), there was no mediation effect (VAF = 0.0). On the contrary, the perceived health effect of secondhand smoking to practice tobacco-free eating places had a significant mediating effect with a VAF value of 0.9 indicating full mediation. However, there was very little or no impact of tobacco-free law or policy on practising tobacco-free eating places. The variance accounted for indicated that there was no mediating effect (VAF = 0.0%). The environmental effect of secondhand smoking had a total effect on practising tobacco-free eating places with an effect size of 0.021 indicating a small effect having no mediating effect (VAF = 0.0%). However, the total effect of supporting tobacco-free restaurants to practice was .315 (P < 0.001) and also attitude had an impact on supporting tobacco-free eating places (E.S. = 0.617, P < 0.001) with environmental effect of secondhand smoking is mediated through attitude to support tobacco-free eating place (E.S. = 0.425, P < 0.001) with no potential effect. Data analysis indicated that knowledge of the environmental effect of secondhand smoking had a potential impact on attitude toward tobacco-free places (E.S. = 0.678, P < 0.001). The knowledge of the health effect of secondhand smoking had no impact (P > 0.05).
| Parameters | Indirect | P-Value | ES | Total | P-Value | ES | VAF (%) |
|---|---|---|---|---|---|---|---|
| Attitude → Support → Practice | 0.198 | 0.001 | 0.020 | 0.198 | 0.001 | 0.035 | 0.0 |
| Health effect of SHS → Attitude →Support → Practice | 0.001 | 0.420 | 0.020 | 0.109 | 0.001 | 0.024 | 0.9 |
| Tobacco-free law → Attitude → Support → Practice | 0.013 | 0.020 | 0.002 | 0.013 | 0.020 | 0.002 | 0.0 |
| Environmental effect of SHS → Attitude → Support → Practice | 0.134 | 0.001 | 0.021 | 0.134 | 0.001 | 0.021 | 0.0 |
| Support → Practice | - | - | 0.315 | 0.001 | 0.100 | - | |
| Attitude →Support | - | - | 0.627 | 0.001 | 0.433 | - | |
| Tobacco-free law → Attitude → Support | 0.042 | 0.014 | 0.008 | 0.042 | 0.014 | 0.008 | 0.0 |
| Health effect of SHS → Attitude → Support | 0.004 | 0.418 | 0.018 | 0.346 | 0.001 | 0.160 | 1.17 |
| Environmental effect of SHS → Attitude → Support | 0.425 | 0.001 | 0.023 | 0.425 | 0.001 | 0.251 | 0.0 |
| Tobacco-free law → Attitude | - | - | 0.067 | 0.014 | 0.015 | - | |
| Environmental effect of SHS → Attitude | - | - | 0.678 | 0.001 | 0.471 | - | |
| Health effect of SHS → Attitude | - | - | 0.006 | 0.418 | 0.001 | - |
Abbreviations: ES, effect size (small (0.02), medium (0.15) and large (0.35)); VAF, variance accounted for (Indirect effect/total effect × 100)
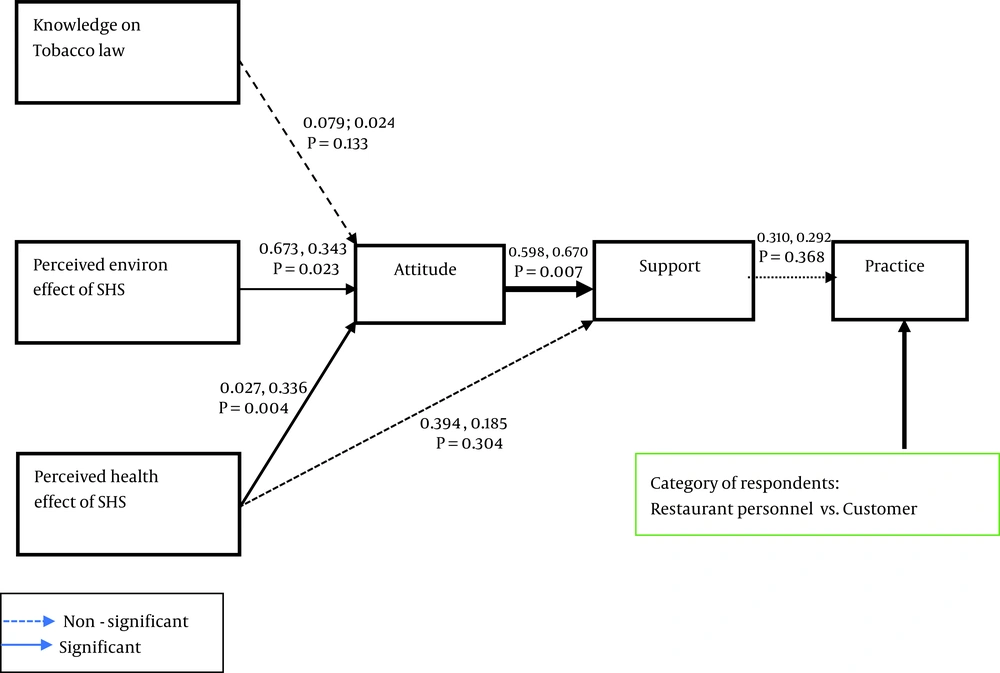
Multi-group analysis revealed no statistically significant difference was found between restaurant personnel and customers in terms of knowledge of tobacco law to attitude towards tobacco-free eating places (P > 0.05), perceived health effect of secondhand smoking to supporting tobacco-free eating places (P > 0.05), and supporting tobacco-free eating place to practicing tobacco-free eating places (P > 0.05). A statistically significant difference was found between restaurant personnel and customers perceived environmental effect of secondhand smoking and attitude towards tobacco-free eating places (P < 0.05), attitude and supporting tobacco-free eating places (P < 0.01), and perceived health effect of secondhand smoking to attitude (P < 0.01) (Figure 3).
4. Discussion
Undoubtedly, smoking-free laws are effective for public health (30, 31) and a cost-effective tobacco control strategy (32). A smoke-free law has eliminated secondhand smoking in public places, thus significantly improving air quality (33). In this study, we developed a structural equation modeling to determine the impact of knowledge, attitude, and supporting tobacco-free eating places to practice tobacco-free eating places using the TPB. The law helps smokers to reduce tobacco-related illnesses, deaths, and healthcare costs, thus preventing smokers from receiving unintentional healthcare services (34, 35) and increasing the government’s revenue capacity (30). The smoking-free law also encourages smokers to quit smoking and helps to reduce the prevalence of smoking (36). The law also could raise public awareness regarding the dangers of tobacco smoke and help individuals to quit smoking voluntarily (37). This law maintains smoke-free homes and cars. A few empirical studies with economic indicators have shown that smoking-free policies have no adverse economic impact on businesses. In particular, a smoking-free policy is associated with increased productivity of workers and a reduction in overhead costs (such as health insurance) (38). Studies also indicated that secondhand smoking indirectly increased air pollution in all public places, restaurants, bars, pubs, and nightclubs (39). Moreover, the hospitality workers absorb a considerable amount of tobacco smoke and experience symptoms of shortness of breath. The study showed a decline in respiratory symptoms among hospital workers after restricting smoking in restaurants and bars (40). In our study, supporting tobacco-free laws strongly encourage practising tobacco-free eating places (P < 0.001). This is consistent with a previous study (41).
Our analysis revealed that increased knowledge of tobacco control laws and perceived environmental effects of tobacco smoke directly impacted attitude towards smoke-free eating places but had no impact on the perceived health effect of secondhand smoking towards attitude. However, perceived health effects of secondhand smoking had a strong effect of supporting smoke-free eating places. It is a complex phenomenon in which public attitudes are essential to facilitate smoke-free legislation or regulations by local or national governments (11). Public attitudes are likely to be impacted by how well such laws are enforced. On the other side, attitudes around smoking might link complex ways with the satisfaction of particular experiences, especially in restaurants and bars. Smokers are already addicted to tobacco, perceived knowledge of tobacco control laws had no effect on practicing smoke-free eating-places though they had to support smoke-free eating places or restaurants, even though they had sufficient knowledge of health effects (42, 43). This might be the fact of complex attitude-to-behavior pathways (44).
There were several limitations in this study. Firstly, we did not examine all forms of tobacco control strategies. Different states might have different media campaigns, interventions, and modes of implementation on tobacco control. Secondly, our study also has the limitation of recall bias, especially regarding the health risk of exposure to SHS. Thirdly, we have tried to maintain the highest level of confidentiality and privacy. Still, there might be the possibility of underreporting because the information given by the workers in the owner’s presence may not be accurate. Finally, our findings may not be generalizable because the study was conducted in only one state in Malaysia.
4.1. Conclusions
In our analysis, we concluded that supporting tobacco-free eating places is significantly associated with the practice of tobacco-free eating places. Similarly, supporting tobacco-free eating places is directly correlated with the attitude towards tobacco-free eating places, perceived health effect of secondhand smoking, and mediating effect of the perceived health effect of secondhand smoking. We found that the perceived health effect of secondhand smoking had no impact on attitude towards tobacco-free eating places. However, the perceived environmental effect of secondhand smoking had a strong impact on tobacco law or policy, while there is a weak impact of knowledge on tobacco law or policy. We suggest that effective tobacco control in Malaysia will require the full implementation of comprehensive tobacco control laws and could be supported by penalties. We also suggest a combination of strong public health education programs involving different segments of the population with the incorporation of people’s current knowledge on tobacco control policy and its implementation.