1. Background
The quality of providing health services is an essential topic in health systems, and increasing knowledge and experience about it are necessary. Therefore, the standard method has been presented as several frameworks and methods, including clinical audit (CA) (1). The CA process was initially introduced in England and adopted by several countries as part of clinical governance to improve patient care and outcomes (2). An assessment of CA is used to determine whether a particular aspect of healthcare is reaching a recognized standard so that healthcare providers know where they can improve (3). The CA examines the health care system, compares it with the standards, and makes changes as necessary (2). Organizations can use CA as a quality improvement measure by showing where they have fallen short in providing quality care (4). The purpose of CA is to highlight the discrepancies between actual practice and the standard to identify the changes needed to improve service quality (5). Healthcare systems have been using CA for decades to ensure patients receive the most effective, up-to-date, and appropriate treatment (6). Further, CA is globally recognized as a method for evaluating the quality of health care, whose benefits include the ability to identify deficits and areas of excellence and develop appropriate recommendations for promoting changes (7). The aspects of clinical care are systematically evaluated in CA based on specific criteria to identify areas requiring improvement for guiding the training and research (6).
Sleep-disordered breathing is now a common disease with severe consequences, the most common type of which is obstructive sleep apnea (OSA) (8). Obstructive sleep apnea is a common health problem known as recurrent upper airway obstruction during sleep, recurrent hypoxia, and hypoxia, shortness of breath, airway obstruction, and waking up (9). The symptoms of OSA include snoring, daily drowsiness, and morning headaches (10). OSA is a clinical syndrome characterized by the recurrence of partial or complete obstruction of the airways during sleep, leading to a decrease in the normal oxygen saturation level of the blood and ending with a brief stimulation of sleep (11).
OSA is one of the most common clinical disorders in societies, which has been identified as one of the determinants of health due to its importance in the quality of life (12). In other words, OSA is a common and underdiagnosed medical condition characterized by recurrent sleep-dependent pauses and decreased airflow (13). Sleep quality is an essential clinical construct for health as one of the acute symptoms of many medical disorders (14).
2. Objectives
Based on the importance of the topic, this study was conducted to determine the CA status of OSA services at the sleep disorders research center of Kermanshah University of Medical Sciences (KUMS), Iran.
3. Methods
3.1. Study Design
A retrospective CA was performed on the records of patients with OSA in 2019 - 2020. The study protocol was approved by the KUMS Research Ethics Committee (IR.KUMS.REC.1400.555).
3.2. CA Procedures
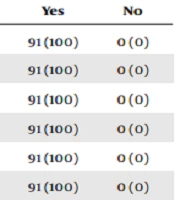
The five steps of CA included defining the standard, collecting the data, comparing current practice with the standard, and applying changes to improve service. The CA team had a sleep disorders specialist, psychiatrist, health promotion specialist, psychiatric nurse, general practitioner, and health policy expert. The international standards (15, 16) for providing clinical services to OSA patients were considered as service delivery standards. The data were collected using a checklist, including background information on patients and international standards for providing OSA clinical services from patients’ medical records. The list was filled out by two general practitioners. The information was collected in the checklist form of yes (the desired service has been performed for the patient) and no (the desired service has not been performed for the patient). At this step, the medical record of 91 patients was examined, and the treatments for OSA patients were compared with the standards. The results regarding the comparison with the standards of providing clinical services to OSA patients are presented in Table 1. As a result, KUMS's sleep research center for OSA patients was evaluated to determine which services did not meet standards. Then, the necessary changes to improve the services provided were determined. The information obtained from CA was provided to the sleep research center of KUMS to improve services. Finally, information and suggestions for matching the OSA service delivery indicators with international standards were given to the sleep research center of KUMS. CA should be re-evaluated one year after implementing the necessary changes to measure the status of providing services to OSA patients at KUMS.
| No | Investigated Indicators for OSA Patients | Yes | No |
|---|---|---|---|
| 1 | Providing training on weight control | 91 (100) | 0 (0) |
| 2 | Advice on not alcohol drinking | 91 (100) | 0 (0) |
| 3 | Providing training on how to sleep (sleeping on your side instead of your stomach or back) | 91 (100) | 0 (0) |
| 4 | Appropriate prescribing of medications | 91 (100) | 0 (0) |
| 5 | If necessary, prescribe CPAP | 91 (100) | 0 (0) |
| 6 | BiPAP administration, if necessary | 91 (100) | 0 (0) |
| 7 | If necessary, prescribe OA | 91 (100) | 0 (0) |
| 8 | Is OAs prescribed, if necessary, for those unwilling to undergo CAPA? | 0 (0) | 91 (100) |
| 9 | Have all interventions to improve tolerability of CPAP therapy been tried before deciding whether therapy has failed in a particular patient? | 0 (0) | 91 (100) |
| 10 | Are surgical options introduced to patients in whom noninvasive medical therapy (eg, CPAP, BiPAP, and OA) has failed? | 91 (100) | 0 (0) |
| 11 | Have patients been informed of the success rate of each surgical procedure? | 91 (100) | 0 (0) |
| 12 | Are patients informed that more than one surgery may be needed to improve OSA? | 91 (100) | 0 (0) |
| 13 | Are patients informed that some surgeries may be very extensive? | 91 (100) | 0 (0) |
| 14 | Are patients only referred to centers with experienced staff in sleep disorders surgery? | 91 (100) | 0 (0) |
| 15 | Has the treatment been followed up? | 0 (0) | 91 (100) |
| 16 | Has adherence medication (such as statins) been assessed? | 0 (0) | 91 (100) |
| 17 | Adherence to noninvasive medical therapy (eg, CPAP, BiAPA, and OA) is follow-up. | 0 (0) | 91 (100) |
| 18 | Are OA treatment adherence reports taken? | 0 (0) | 91 (100) |
a Values are expressed as No. (%).
3.3. Statistical Analysis
The data were described using SPSS software version 16. For this purpose, descriptive statistics, including mean, standard deviation (SD), frequency, and percentage, were used.
4. Results
The average age of the patients was 50.10 (SD = 13.16), ranging from 16 to 76 years. More details of the background variables of the OSA patients are shown in Table 2. The patients’ average body mass index (BMI) was 31.64 with an SD of 5.92 (BMI was 34.19 for women and 30.20 for men). The results showed that 58.2% of patients were in the obese category, 6.6% of patients had a history of opium use, and 28.6% of patients had a university education. Most patients were married (86.8%).
| Variables | No. (%) |
|---|---|
| Age group (y) | |
| Under 30 | 6 (6.6) |
| 30 - 39 | 13 (14.3) |
| 40 - 49 | 20 (22) |
| 50 - 59 | 30 (33) |
| 60 - 80 | 22 (24.2) |
| Gender | |
| Female | 33 (36.3) |
| Male | 58 (63.7) |
| Education level | |
| Illiterate | 9 (9.9) |
| Primary school | 38 (41.8) |
| High school | 18 (19.8) |
| Academic | 26 (28.6) |
| Marital status | |
| Single | 8 (8.8) |
| Married | 79 (86.8) |
| Widow or divorced | 1 (1.1) |
| Missing | 3 (3.3) |
| BMI status | |
| Underweight range | 1 (1.1) |
| Healthy weight range | 9 (9.9) |
| Overweight | 28 (30.8) |
| Obese | 53 (58.2) |
| Opium use | |
| No | 85 (93.4) |
| Yes | 6 (6.6) |
As shown in Table 1, the services were provided to all OSA patients based on indicators such as training in a healthy lifestyle related to OSA (weight control, no alcohol drinking, and sleep health behaviors), appropriate prescribing of medications and devices like continuous positive airway pressure (CPAP) and bilevel positive airway pressure (BiPAP). Indicators such as follow-up on prescribed CPAP and BiPAP devices, informing patients about the frequency of possible surgeries, and follow-up treatment was not performed for the patients.
5. Discussion
This study indicated the strengths and weaknesses in providing services to OSA patients in the sleep disorders research center of KUMS. Providing clinical services to OSA patients requires paying attention to the weak points. In general, the treatment follow-up for OSA patients in the western parts of Iran was poor, especially in using CPAP and BiPAP. Aloia et al. indicated that implementing eHealth interventions improved treatment adherence among OSA patients (17). Implementing educational interventions for the OSA treatment medical teams and follow-up programs for treating patients can lead to critical clinical achievements.
A total of 89% of the patients were obese or overweight based on BMI. In this regard, Erridge et al. stated numerous comorbidities in obese patients associated with an increased likelihood of OSA (18). On the other hand, the BMI of women was significantly higher than that of men. Some other studies have also reported that female patients have a higher BMI among patients with sleep disorders (19). Doctors can use the results to treat OSA patients. Paying particular attention to the weight control programs of patients can improve the clinical condition of OSA patients. Nutritional interventions are especially recommended for women with OSA.
The results also showed that 6.6% of the patients had a history of opium use. In this regard, Nerfeldt et al. reported that the prevalence of drug use among patients with obstructive sleep apnea syndrome (OSAS) was 3.2 % based on laboratory tests (20). Doctors can also consider this point in treating OSA patients.
5.1. Limitations
This study is the first CA in Iran to assess the status of services provided to OSA patients. A weak set of indicators was highlighted in this study regarding the provision of OSA services in the west of Iran. These data can be a basis for healthcare services providers to identify the indicators requiring modification. However, there were some limitations while conducting the research. First, CA evaluated the information from the patient’s medical records and failed to detect non-recorded actions. Hence, it is essential to emphasize recording all clinical procedures. This CA was a cross-sectional analysis without evaluation of long-term clinical data.
5.2. Conclusions
Based on the results, OSA patients' treatment follow-up indicators were not in compliance with the standards in western Iran, and this needs to be addressed in providing clinical services to OSA patients. Identifying weak points can help develop and implement targeted interventions for improving the situation of providing clinical services to OSA patients in Iran.