1. Introduction
Epiretinal membrane (ERM) is a prevalent retinal disease with cellular proliferation and metaplasia that cause pathological fibrocellular membrane that cause superjacent to the inner retinal surface (1). Between 7% and 11.8% of people have epiretinal membrane (ERM), with age as the major risk factor. While, the majority of ERM is idiopathic, usual secondary factors are uveitis, retinal tears, cataract surgery, and retinal vascular disease (2). Epiretinal membranes (ERMs) appears on the surface (i.e. the internal limiting membrane) of the retina, usually at the posterior pole and macular. Usually, ERM appears in individuals above 59 years old and affects both eyes in at most 13.5% of cases (3). The available intervention for ERM cases includes pars plana vitrectomy and peeling the membrane, which causes a significant improvement of the symptoms in most of the cases. There are also surgical risks of retinal detachment, retinal tears, and endophthalmitis (4). Young subjects, women, and myopes are the most common groups in which ERM spontaneously separate. It usually improves visual acuity and occurs in about 1 - 3% of cases overall (5-8). Contraction of Vitreous that causes the fundus condition and needs photocoagulation can change the vitreous or membrane and improve the peeling of the membranes (9). There are three ways that ERM can spontaneously separate: (1) detachment of the posterior vitreous that results in the pulling of the ERM by the vitreous (usually for adults); (2) with an increase in the contraction forces in immature ERM higher that the adhesive force with retinal causes a slow tangential traction of the edges of ERM and separation of the edges toward the center (remodeling common in youngsters); and (3) acute membrane retraction toward the epicenter and tearing of the ERM at the central point which is the weakest (10).
2. Case Presentation
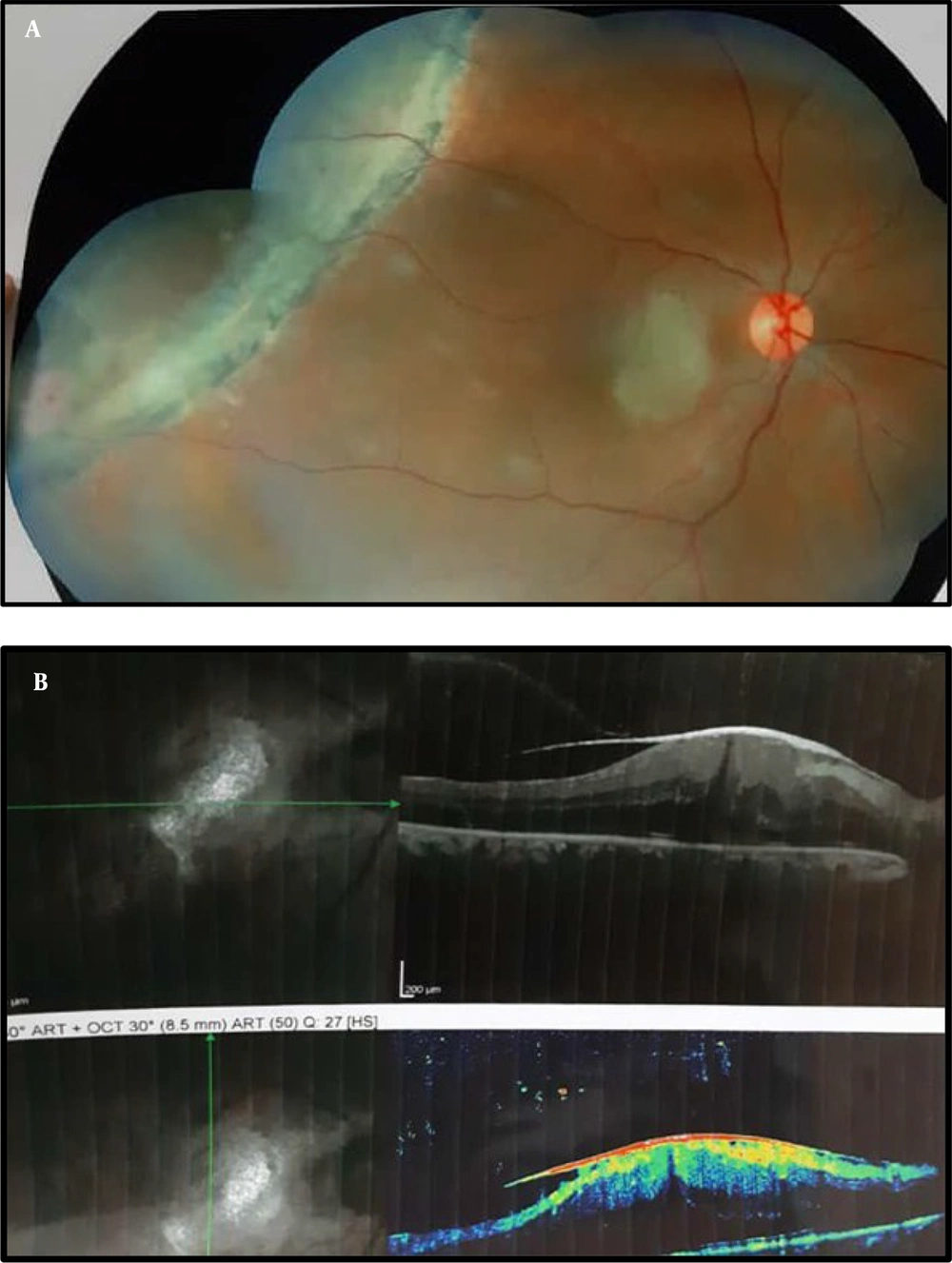
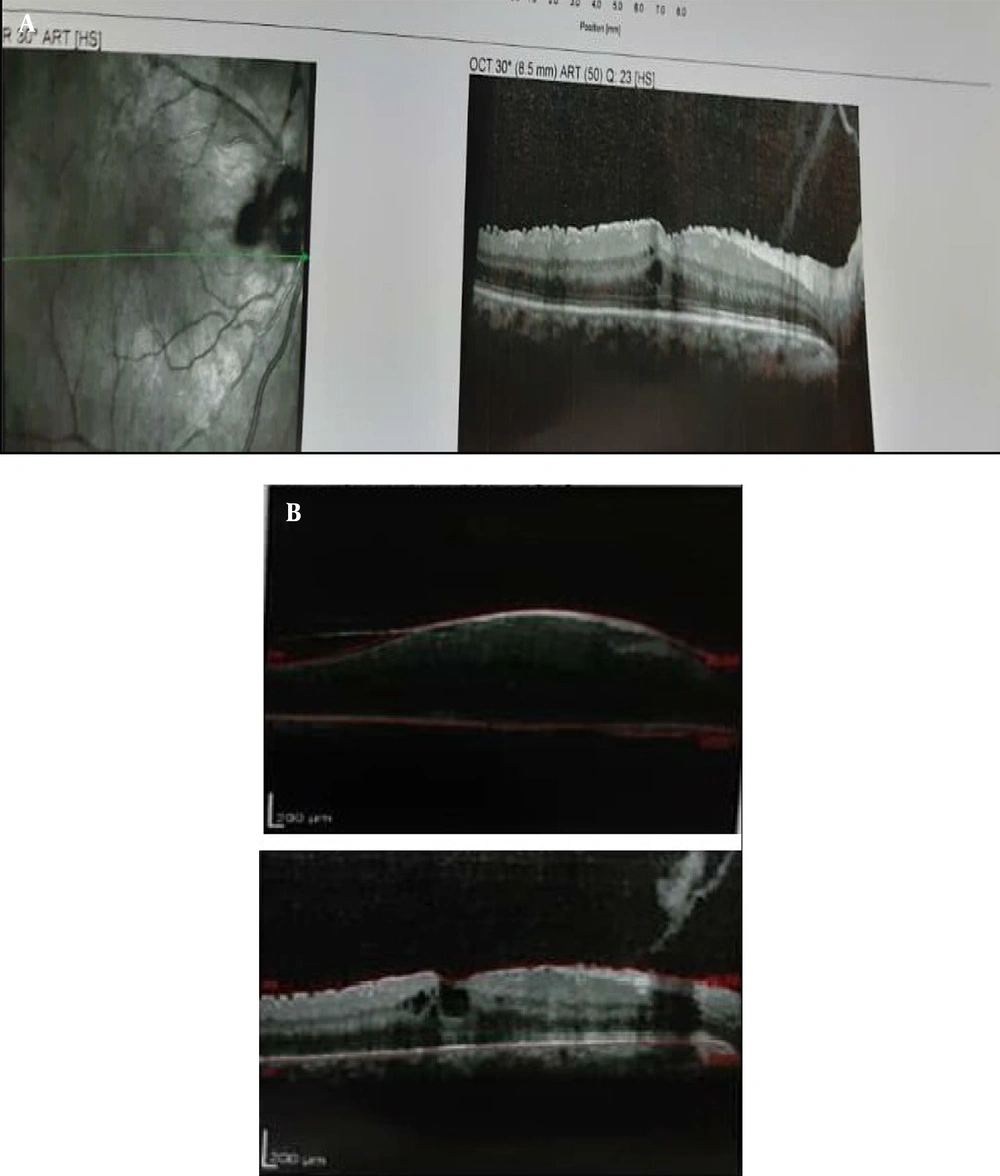
A female, 44-year-old, was presented to ophthalmology clinic due to a three-month-old complaint of blurred vision in the right eye. She did not have any eye surgery, infections, trauma, uveitis, or systemic diseases. In the right eye, the patient had a BCVA of 2/10, while in the left eye, it was 9/10. The anterior part of the eyes was examined normally, but the posterior segment revealed pigment atrophy, retinal wrinkling in the macular region, and a tear in the right eye's supratemporal region. (Figure 1A). The intraocular pressure was normal in both eyes. Optical coherence tomography (OCT) of the area affected had the ERM with a hyper-reflective layer and higher thickness of central foveal and intraretinal oedema (Figure 1B). With diagnosis of retinal break associated with secondary ERM in the patient's right eye, 1 session of retinal barrier laser photocoagulation in the supratemporal quadrants was performed. Watchful waiting strategy was chosen. at 2-month follow-up, VA improved to 4/10 in the right eye. OCT revealed that ERM was not attached to the surface of the macula by remaining parapapillary fixation (Figure 2A). SD-OCT showed a proceeded with partition of the ERM crossing the fovea and staying connected nasal to the fovea (Figure 2B).
(A) Fundus photograph pigment atrophy and retinal wrinkling in the macular area and a break was notice in the supratemporal area of the right eye; (B) Optical coherence tomography (OCT) of the affected area confirmed the ERM with a hyper-reflective layer with an increased central foveal thickness and intraretinal oedema.
3. Discussion
An avascular, fibrocellular membrane known as the ERM was found for the first time in 1865. When expanded to the inner surface of the retina, causing varying degrees of visual impairment. Macular ERMs, in contrast to peripheral ERMs, are more visually alarming. Macular ERMs affect two percent of people under the age of 60 and 12 percent of people over 70 (11). Epiretinal membrane can be secondary or idiopathic, affecting otherwise healthy eyes. In the latter, they are linked to retinal breaks, vascular retinopathy, posterior vitreous detachment (PVD), ocular inflammation, some congenital disorders, and intra-ocular surgery like repair after retinal detachment, retinal laser, cataract repair, and cryotherapy (3). There are three ways that ERM can spontaneously separate: (1) detachment of the posterior vitreous that results in the pulling of the ERM by the vitreous; (2) the contracting of the immature ERM grows stronger in comparison with its adhesions to the retina; which results in a gradual ERM edge tangential traction and center-ward separation from the edges (remodeling mostly used for younger cases); and (3) acute membrane retraction toward the epicenter and tearing of the ERM at the central point which is the weakest (10). Eye trauma, toxoplasma uveitis, and laser surgery (YAG-laser capsulotomy and pan-retinal photocoagulation) were all associated to spontaneous ERM release (12, 13).
In this patient, after the laser of retin break, spontaneous epithelial separation occurred. According to studies, one of the causes of spontaneous separation of the ERM is increased pressure on the membrane, the closure of retin break may lead to stretching on the retinal membrane and this factor has caused this happening.
Given the risk of spontaneous ERM separation and improvement in visual symptoms, patients without or mild symptoms can be monitored cautiously. Using standard structural examination and checking macular anatomy using OCT to find ERM is recommended to avoid or delay operations until a major decrease in vision or pertinent visual symptoms.