1. Background
A novel coronavirus was reported in Wuhan City, China on December 31, 2020, and the outbreak of the coronavirus disease (COVID-19) has become one of the biggest critical situations in the last five years worldwide (1). Although at the beginning of the outbreak of COVID-19, the mortality rate was approximately 1 - 5%, but due to the extraordinary spread of this virus and the rapid and unexpected spread of this disease in different communities, there are many concerns was created for the people (2). Due to the persistence of this virus in flat surfaces and the strength of its contagion among community members, especially in care and treatment environments, special measures were taken in hospitals to admit and care for patients with COVID-19. In addition, due to the new nature of this virus, at the beginning of the outbreak of COVID-19, people did not know how to protect themselves against it. Therefore, the rate of its transmission among people increased rapidly and eventually became a pandemic disease in the world (3, 4).
Symptoms of COVID-19 occur after an incubation period of approximately 5 - 6 days. Also, from the time of onset of symptoms to the time of death of patients, it varied from 6 to 41 days (with an average of 14 days) (5). This period depends on the age and the state of the patient's immune system, so that the rate of infection and death due to COVID-19 in people under 70 years old was lower than in patients over 70 years old (6). The most common symptoms of COVID-19 include fever, cough, muscle pain, and fatigue, and other symptoms include sputum production, headache, bleeding, diarrhea, indigestion, and lymphopenia (3, 5, 7, 8).
In most patients with COVID-19, the clinical features of this disease show themselves as pneumonia in the chest X-ray. Non-specific features such as acute respiratory distress syndrome, acute heart complications and occurrence of a white hazy area in the lung tissue (ground-glass opacity) which leads to death are also seen in some patients (9, 10). In some cases, ground-glass opacity is observed at the base of both lungs, which probably increases the resulting systemic and local immune response and ultimately leads to increased inflammation (11, 12).
The involvement of several organs, including the liver, digestive system, and kidney, has been reported in SARS in 2003 and recently in patients with COVID-19 (13, 14). Although the respiratory and immune systems are the main targets of COVID-19 disease, acute kidney injury (AKI) and urinary protein excretion have also been observed (15). For this reason, it is very important to take preventive measures against the occurrence and progression of acute kidney failure in patients with COVID-19 (16). The management of COVID-19 in patients with kidney disease is even more challenging, as the mortality rate from pneumonia in patients with chronic kidney disease (CKD) is 14 - 16 times higher than in the general population (17, 18). Based on the results of previous studies, the severity of complications is higher in patients with CKD who have immune system defects (19, 20).
2. Objectives
Although COVID-19 mainly targets the respiratory system, it may also damage other organs of the patient's body, such as the kidneys. Based on this, the main aim of the present study was to determine kidney function in patients with COVID-19 hospitalized in Imam Khomeini Hospital, Sari, Iran.
3. Methods
3.1. Study Design and Implementation
This study was cross-sectional, which was selected by the census method of all available samples. The statistical population of this research included patients admitted to Imam Khomeini Hospital, Sari, Iran with a definite diagnosis of COVID-19 based on the findings of radiology, CT scan or molecular test. Sampling during this study was non-random and all patients who met the inclusion and exclusion criteria of this study were examined. Definite infection with COVID-19 and the completeness of patient file information were considered as inclusion criteria, while lack of access to patient information and also death before obtaining checklist information were considered as exclusion criteria. The sample size of this study was 498 hospitalized patients with COVID-19, after selecting the patients and obtaining consent to participate in the study, the information required for the study including demographic information (including age, gender, marital status and employment status), clinical information (including disease symptoms, comorbidities and complications) and laboratory information of patients were received, then entered into the researcher's checklist. Patients were evaluated in three stages (first, third and sixth days after the start of the study) and their results were recorded. Finally, the data obtained by SPSS software version 19 was analyzed using two independent samples t-tests and chi-square at the significance level (α = 0.05).
3.2. Definition of Terms Related to Kidney Diseases and Their Treatment
Kidney disease or renal disease or nephropathy actually means damage or various diseases related to kidneys. Nephritis is an inflammatory disease of the kidney and it has different types based on the location of the inflammation. Kidney disease often causes some degree of loss of kidney function and may lead to kidney failure, complete loss of kidney function. Renal failure is often referred to as end-stage renal disease, the stage for which the only remaining treatments are dialysis or kidney transplant. Kidney failure is divided into two categories, acute and chronic. Acute kidney disease is now called AKI, which is characterized by a sudden decrease in kidney function for more than seven days. Chronic kidney disease is a type of kidney disease with gradual loss of kidney function over a period of several months to several years. Kidney disease: Improving global outcomes (KDIGO) is the global nonprofit organization developing and implementing evidence-based clinical practice guidelines in kidney disease. A kidney transplant is the transfer of a healthy kidney from one person into the body of a person who has little or no kidney function. The kidney purifies the blood by removing waste materials and excess fluids from the body. These waste materials are sent to the bladder and removed from the body with urine. If the kidneys fail, dialysis does the work of the kidneys (21).
4. Results
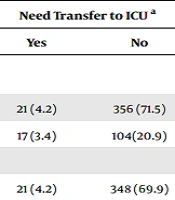
The results of the present study showed that 49.6% (247 people) of the evaluated patients were women and 50.4% (251 people) were men. Based on the results, the minimum and maximum ages of hospitalized patients were 16 and 93 years, respectively, with an average of 55.2 ± 16.4 years. The death rate among hospitalized patients was equal to 60 people (12%). Among hospitalized patients, the most common diseases recorded in addition to COVID-19 included blood pressure (33.3%), diabetes (28.5%) and cardiovascular diseases (13.3%), respectively. and other underlying diseases were ranked next (Table 1). Among kidney disorders, CKD had the highest frequency (25.9%). According to KDIGO criteria, 12.9% of patients with AKI were (Table 2). The presence of kidney disease and the development of AKI showed a significant relationship with the need for intensive care unit (ICU) (P < 0.05) (Table 3). The results showed that although initially there was significant relationship between kidney disease and transfer to ICU (P < 0.05), but after removing the effect of age and gender variables, this relationship was not significant (P > 0.05) (Table 4). Based on the results, it was found that the abnormal compounds of urea and creatinine, among large number of patients with COVID-19 have died (Table 5).
| Type of Underlying Disease | Values |
|---|---|
| Diabetes | |
| Yes | 142 (28.5) |
| No | 356 (71.5) |
| Hypertension | |
| Yes | 166 (33.3) |
| No | 332 (66.7) |
| Cardiovascular | |
| Yes | 66 (13.2) |
| No | 432 (86.8) |
| Lung failure | |
| Yes | 16 (3.2) |
| No | 482 (96.8) |
| Cancer | |
| Yes | 21 (4.2) |
| No | 477 (95.8) |
| Rheumatism | |
| Yes | 14 (2.8) |
| No | 484 (97.2) |
| Various kidney diseases | |
| Yes | 212 (42.6) |
| No | 286 (57.4) |
| Total | 498 (100) |
Frequency of Patients with COVID-19 in Terms of Underlying Diseases a
| Variables | Values |
|---|---|
| CKD | |
| Yes | 129 (25.9) |
| No | 369 (74.1) |
| Kidney dialysis | |
| Yes | 17 (3.4) |
| No | 481 (96.6) |
| Kidney transplant | |
| Yes | 2 (0.4) |
| No | 496 (99.6) |
| KDIGO | |
| Yes | 64 (12.9) |
| No | 434 (87.1) |
| Total | |
| Yes | 212 (42.6) |
| No | 286 (57.4) |
Frequency of Patients with COVID-19 Who Had Different Kidney Diseases a
| Variables | Need Transfer to ICU | P-Value | |
|---|---|---|---|
| Yes | No | ||
| The presence of kidney disease | 0.005 | ||
| Yes | 21 (4.2) | 356 (71.5) | |
| No | 17 (3.4) | 104(20.9) | |
| CKD | 0.011 | ||
| Yes | 21 (4.2) | 348 (69.9) | |
| No | 17 (3.4) | 112 (22.5) | |
| Kidney dialysis | > 0.99 | ||
| Yes | 37 (7.4) | 444 (89.2) | |
| No | 1 (0.2) | 16 (3.2) | |
| Kidney transplant | > 0.99 | ||
| Yes | 38 (7.6) | 458 (92) | |
| No | 0 (0) | 2 (0.4) | |
| KDIGO | < 0.001 | ||
| Yes | 21 (4.2) | 413 (83.0) | |
| No | 17 (3.4) | 47 (9.4) | |
| Total | 498 (100) | 498 (100) | - |
The Frequency of Patients with COVID-19 and Various Kidney Diseases Who Needed to Be Transferred to the Intensive Care Unit a
| Variables and Outcome | Year | Values | P-Value |
|---|---|---|---|
| Age | < 0.001 | ||
| Died | 53.5 ± 15.8 | 438 (87.9) | |
| Survived | 67.7 ± 14.5 | 60 (12.1) | |
| Sex | 0.096 | ||
| Woman | |||
| Died | - | 27 (5.4) | |
| Survived | - | 247 (49.6) | |
| Man | |||
| Died | - | 33 (6.6) | |
| Survived | - | 191 (38.4) |
The Effect of Sex and Age Variables on Outcome of the Disease in Patient with COVID-19 a
| Compound and Measurement Turn | Status | Frequency a | P-Value | |
|---|---|---|---|---|
| Died | Survived | |||
| Urea | ||||
| First time | Normal | 0 (0) | 48 (9.6) | 0.007 |
| Increased | 60 (12) | 390 (78.4) | ||
| Second time | Normal | 0 (0) | 38 (7.6) | 0.018 |
| Increased | 60 (12) | 400 (80.4) | ||
| Third time | Normal | 0 (0) | 426 (85.6) | 0.194 |
| Increased | 60 (12) | 12 (2.4) | ||
| Albumin | ||||
| First time | Normal | 0 (0) | 426 (85.6) | 0.194 |
| Increased | 60 (12) | 12 (2.4) | ||
| Second time | Normal | 0 (0) | 426 (85.6) | 0.194 |
| Increased | 60 (12) | 12 (2.4) | ||
| Third time | Normal | 0 (0) | 426 (85.6) | 0.362 |
| Increased | 60 (12) | 12 (2.4) | ||
| Creatine | ||||
| First time | Normal | 30 (6) | 360 (72.3) | < 0.001 |
| Increased | 30 (6) | 78 (15.7) | ||
| Second time | Normal | 30 (6) | 380 (76.3) | < 0.001 |
| Increased | 30 (6) | 58 (11.7) | ||
| Third time | Normal | 38 (7.6) | 400 (80.4) | < 0.001 |
| Increased | 22 (4.4) | 38 (7.6) | ||
Changes of Urea, Albumin and Creatinine in Three Times of Measurement in Patient With COVID-19
5. Discussion
Although COVID-19 mainly targets the respiratory system, it may also damage other organs of the patient's body, such as the kidneys. Based on this, the main aim of the present study was to determine kidney function in patients with COVID-19 hospitalized in Imam Khomeini Hospital, Sari, Iran.
According to the results of the present study, among the hospitalized patients, the most common diseases recorded in addition to COVID-19 include blood pressure (33.3%), diabetes (28.5%) and cardiovascular diseases (13.3 %) and other underlying diseases ranked next. Among kidney disorders, the most types of kidney disorders among hospitalized patients were related to CKD (25.9%) and KDIGO (12.9%), respectively. The presence of kidney disease and the development of AKI showed significant relationship with the need for ICU. The results showed that although initially there was significant relationship between kidney disease and ICU transfer (P < 0.05), but after removing the effect of age and gender variables, this relationship was not significant. Based on the results, it was found that the abnormal compounds of urea and creatinine, among large number of patients with COVID-19 have died.
The findings of various previous studies showed that the prevalence of AKI in COVID-19 patients was different. In the studies of Aggarwal et al. (22), Cheng et al. (23), Pei et al. (24), Diao et al. (25), Li et al. (26), Yang et al. (27), Zhou et al. (28) and Chen et al. (29) reported that the prevalence of AKI was 69.0%, 5.1%, 6.60%, 27%, 70.7%, 29%, 14.7% and 11.0% respectively. The results of the study by Zhu et al. with a sample size equal to 3062 COVID-19 patients, showed that the incidence of abnormal renal function is equal to 25.5% (30).
The results of Passoni et al. showed that the incidence of AKI in general and in ICU was 9.2% (4.6 - 13.9) and 32.6% (8.5 - 56.6), respectively. According to the results of the mentioned study, the incidence of AKI in elderly patients and those with acute respiratory syndrome was 22.9% (4.0 - 49.7) and 4.3% (1.8 - 6.8), respectively. The incidence of AKI in patients with secondary infection was estimated to be 31.6% (12.3 - 51.0). In addition, the results of the mentioned study showed that the estimated incidence for patients who needed renal replacement therapy (RRT) was 3.2% (1.1 - 5.4) and the estimated AKI mortality was 50.4% (17.0 - 83.9) reported (31).
Based on the results of Yang et al. study, it showed that 29% of 52 critically ill Chinese patients were diagnosed with AKI (27). In the study of Huang et al., 23% of patients admitted to the ICU developed AKI, while none in non-ICU care had such conditions (32). Goldfarb et al. reported that out of 105 patients with COVID-19 in the ICU, 44 patients had AKI and 40 of whom required kidney replacement therapy (KRT) (33).
The results of Li et al. (34), Cheng et al. (23) and Pei et al. (24) showed that significantly, high percentage of patients had symptoms of renal dysfunction during hospitalization. According to the results of these studies, 44 to 65% of patients with proteinuria, 27 to 44% with hematuria, 10 to 14% with increased serum creatinine showed symptoms of kidney dysfunction (23, 24, 34).
The presence of underlying diseases, including hypertension, cardiovascular diseases, cancer, obesity, and type 2 diabetes, are likely to cause COVID-19 and cause a severe disease (22). In the present study, there was a comparison between two groups of people with kidney failure, high blood pressure and cardiovascular disease as the most important underlying disease. Patients with COVID-19 usually die from various causes such as multi-organ failure, shock, respiratory failure, heart failure, arrhythmias, and renal failure (22). Previously, it has been shown in various studies that older age and suffering from several diseases at the same time can cause defects in the response of the body's immune system to pathogens, dysfunction of body organs, acceleration of inflammation and finally lead to death in ICU (35-40). In addition, it has been shown in previous studies that the simultaneous occurrence of other diseases may cause weakness in the immune system and dysfunction of the body. This issue is more effective in elderly patients than in young patients with COVID-19 (35, 36, 41, 42). Previous studies reported cardiovascular disease, pulmonary obstruction, blood pressure, diabetes, and kidney failure as the most important risk factors for disease severity and death due to COVID-19 (43).
Renal dysfunction evident with proteinuria and hematuria without meeting AKI criteria may also predict outcomes. The study by Pei et al. showed that the incidence of proteinuria and hematuria was almost twice as high in critically ill patients as in patients with moderate disease (81% vs. 44% for proteinuria, 69% vs. 33% for hematuria). Also, based on the mentioned results, among 333 COVID-19 patients, the mortality rate in patients with kidney involvement, including hematuria, proteinuria, and AKI, was more than 9 times higher than in patients without kidney involvement (11.2 vs. 1.2%) (24). Different observations in the results of this study with other similar studies can be caused by racial differences, severity of the disease, measurement times, laboratory methods, as well as different definitions of CKD.
5.1. Limitations
The most important limitations of this study included the incompleteness of some patients' files in terms of demographic and clinical information and the limited period of time to observe the condition of hospitalized patients.
5.2. Conlusions
Based on the results of the present study, it can be concluded that underlying diseases such as kidney failure can be very effective in contracting COVID-19 as well as increasing its severity. In addition, the risk of mortality is higher in kidney patients with COVID-19 compared to the general population. Therefore, it seems more necessary to take preventive measures and take care of these patients.