1. Background
Smoking is a significant behavioral risk factor with an attributable health burden worldwide (1). Cigarette smoking is a significant threat to public health as the world’s largest preventable cause of death, with approximately eight million premature deaths annually (2). Smoking continues to have a high prevalence worldwide, despite the evidence that it harms people’s health and those around them (36.7% prevalence in men and 7.8% in women) (3). Almost 1.3 billion people aged 15 and older smoke worldwide, 80% living in low- and middle-income countries (LMICs). It is estimated that the number of smokers will increase in developing countries. For example, the findings of a study indicated that smoking among adolescents in LMICs is more than four times the rate in the UK (4). Smoking usually begins during adolescents and has become more common among young people in recent years (5).
According to the STEP survey 2015 among Iraqi adults aged (18+ years), the prevalence of present smokers was 20.7%, and the amount of smoking among males was 20 times higher than among females (38% vs. 1.9%) (6). In the Kurdistan region, the smoking rate among college students was 12.3%, and the prevalence of smoking among male students was higher than among female students (23.9% and 1.9 %) (7).
The evidence shows that using theory facilitates the most efficient and effective health behavior intervention measures, and applying theory has a prominent role in education and health promotion interventions (8). The theory is the essential criterion for evidence-based health promotion because of facilitating the understanding of health-related behaviors and providing goals and strategies for interventionists (9). The integrative model of factors influencing smoking behavior (IMFISB) is specifically used to identify the determinants of smoking behavior during adolescence and illustrate the progressing stages in which smoking behavior happens. The integrative model of factors impacting smoking behaviors shows four stages in which smoking behavior in adolescents grows and outlines the critical psychological, environmental, and social factors at the different stages of smoking behavior (10).
Furthermore, using mobile technologies and devices to maintain health and well-being is a promising opportunity for health policymakers and relevant stakeholders (11, 12). In addition, by 2019, more than seven billion people (95% of the world’s population) live in an area covered by a mobile phone network. Therefore, most places have the infrastructure for implementing mhealth interventions (13).
2. Objectives
The current study aimed to evaluate the mhealth program to promote smoking prevention behaviors among university students in northern Iraq. IMFISB was used as a theoretical framework.
3. Methods
3.1. Participants
The quasi-experimental research study was conducted from March to June 2023 among 150 Kurdish students of Raparin University in northern Iraq. Students were selected and randomly divided into two intervention groups (75 people) and control (75 people). The inclusion criteria were being a Kurdish student of Raparin University in northern Iraq, having a smartphone, and wanting to participate in the research. Non-participation in training sessions and incomplete answers to questionnaire items were the exclusion criteria.
3.2. Measures
Google Forms were used to collect data, and an invitation link containing a survey questionnaire was mailed to the students by the university teachers. Students were asked to fill out the questionnaire once to avert response duplications. Students were informed regarding the confidentiality of their responses, and the participation was voluntary. The questionnaire was designed based on standard questionnaires (14-16) in two sections. The first section included 15 questions that determined the socio-demographic data such as (gender, age, academic year, marital status), educational level of their parents, economic status of the family, the student staying place, and the student’s smoking status. The second part of the questionnaire included 33 questions, in which the items assessed the IMFISB determinants. Specifically, six items were used to measure the knowledge of the health effects of smoking (e.g., do you know that smoking cause lung cancer). Seven items measure the attitude (e.g., I support restaurant smoking bans). Three items measured the belief (e.g., I believe I will get cancer if I smoke). The value was measured by three items (e.g., smoking causes harm to my body). Two items measured the intention (e.g., I might start smoking in the next two months). Two measured the family influence (e.g., if one of your family members offers you a cigarette, will you smoke it?). The peer influence was measured using two items (e.g., if one of your closest friends gives you a cigarette, will you smoke it?). In addition, four items measured the self-image of smoking (e.g., I think I have low self-esteem if I smoke). The smoking preventive behaviors were measured by four items (e.g., if someone smokes next to me, I leave the place). A research team analyzed the questionnaire to ensure the content’s readability and accuracy. A pilot test was performed to evaluate the reliability and validity of the questionnaire. Then, a certified English teacher translated the final questionnaire into Kurdish. Estimated reliability using alpha Cronbach coefficient for each construct’s questionnaire were as follows: Knowledge (α = 0.73), attitude (α = 0.80), value (α = 0.61), belief (α = 0.79), intention (α = 0.89), family influence (α = 0.63), peer influence (α = 0.86), self-image (α = 0.74), and smoking preventive behaviors (α = 0.70).
3.3. Procedure
The authors developed an organized and innovative educational application program under the name of (Avoid Smoking) to improve the most determinants related to smoking prevention among college students of Raparin University. The results of the cross-sectional study were analyzed to design the contents of the educational application intervention. The educational priorities for each variable were determined, and the educational application program contents were aligned with these priorities and the idea of experts. The decision for the number of intervention lessons was based on the authors’ experiences.
The present study considered IMFISB as a theoretical framework for explaining behavior change. IMFISB does not have a protocol for program development. Thus, the intervention mapping (IM) approach was considered a guiding framework for the development and implementation strategies for program adoption, implementation, and maintenance because of the comprehensiveness of the programs developed based on IM (17).
The goals of each training session were determined based on the needs assessment conducted in the formative evaluation study and IMFISB determinants. Training sessions using the mobile application (Avoid Smoking) were conducted based on the mhealth strategy (18) because of college students’ capabilities, smartphone access, and the benefits of this delivery method.
The application consisted of eight educational lessons. The first lesson included information to improve the knowledge of students about smoking. The second to fourth lessons were related to subjective norms and included increasing and understanding many pressures people face when offering a cigarette and providing information to recognize between positive and negative peer pressure. The fifth and sixth sessions provide information regarding the addictiveness of smoking and enhance the attitude of students about the effects of starting smoking at a young age. The seventh and eighth lessons improve students' self-image towards smoking behavior and increase participants' self-image to deal with smoking cravings. A set of theoretical behavior change methods based on the Kok et al. (19, 20) classification was used for each determinant.
The application provided interactive methods, including short videos, written content, and images, to make educational lessons more engaging (Table 1).
| Determinants | Lessons | Practical Application, Strategy, | Parameter Use | Change Objectives |
|---|---|---|---|---|
| Knowledge | Lesson one | Providing written material, images | Should be relevant, plain and vary in format and media; learning moments should be short; adding helpful information | Enhance the knowledge and understanding towards effects of smoking on smokers’ lungs; increase the knowledge via images regarding effects of smoking on the body |
| Attitude + belief + value | Lesson five and six | Providing written material, images | Should be relevant, comprehensible, and interesting to follow; reinforcement of the model | Increasing awareness regarding smoking as an addictive material; increasing the attitude of students regarding effects of starting smoking in a young age |
| Family + peer pressure | Lesson two, three and four | Providing written material, images, short videos | Requires building of refusal skills | Enhancing parental support to their teenagers about smoking use; have the ability to say no to smoking in many ways; increasing and understanding many pressures that people face related to offering a cigarette; providing information to recognize between positive and negative peer pressure |
| Self-image | Lesson seven and eight | Providing written material, images, and short videos | Go to places without smoking, or with people that do not smoke. | Increase, self-image towards smoking behavior; increasing self-image of participants via images to deal with smoking cravings; changing idea of participants regarding second hand smoke effects; how to build positive self-image towards bad behavior (smoking) |
3.4. Statistical Analysis
Analyses were conducted by SPSS software 16. A cross-tabulation test and independent t-test were used to assess the status of these variables before and after the program was implemented. Independent t-tests and paired sample t-tests were employed to determine the comparability of the intervention in comparison with the control group. In addition, the effect size (Cohen’s d) for IMFISB constructs was estimated as the mean score of the intervention group minus the mean score of the control group divided by the standard deviation. Cohen provided a method to interpret effect size. Values smaller than 0.2, 0.2 to 0.499, 0.5 to 0.8, and more than 0.8 are interpreted as small, medium, large, and very large, respectively (21). Levene’s test was utilized to measure the equality of IMFISB constructs variances. Cronbach’s coefficient alpha was used to estimate the internal consistency of the various measures.
4. Results
The mean age of respondents was 21.29 years (95% CI: 21.05, 21.53). Table 2 indicates no significant difference between the intervention and control groups in socio-demographic variables before the intervention program.
| Variables | Intervention | Control | P-Value |
|---|---|---|---|
| Age | 21.51 ± 1.42 | 21.07 ± 1.51 | 0.069 |
| Gender | 0.247 | ||
| Female | 46 (47.4) | 51 (52.6) | |
| Male | 29 (54.7) | 24 (45.3) | |
| Academic level | 0.306 | ||
| First and second year | 45 (47.9) | 49 (52.1) | |
| Third and fourth year | 30 (53.6) | 26 (46.4) | |
| Working beside study | 0.101 | ||
| Yes | 10 (37) | 17 (63) | |
| No | 65 (52.8) | 58 (47.2) | |
| Family income | 0.236 | ||
| Bad | 10 (71.4) | 4 (28.6) | |
| Good | 54 (47.4) | 60 (52.6) | |
| Very good | 11 (50) | 11 (50) | |
| Father educational level | 0.577 | ||
| Illiterate | 26 (42.6) | 35 (57.4) | |
| Primary school | 24 (54.5) | 20 (45.5) | |
| Secondary school | 11 (50) | 11 (50) | |
| High school | 10 (58.8) | 7 (41.2) | |
| University degree | 4 (66.7) | 2 (33.3) | |
| Mother educational level | 0.407 | ||
| Illiterate | 46 (47.4) | 51 (52.6) | |
| Primary and secondary school | 25 (58.1) | 18 (41.9) | |
| High school | 4 (40) | 6 (60) | |
| Marital status | 0.214 | ||
| Married | 10 (62.5) | 6 (37.5) | |
| Single | 65 (48.5) | 69 (51.5) | |
| living in dormitory | 0.205 | ||
| Yes | 46 (53.5) | 40 (46.5) | |
| No | 29 (45.3) | 35 (54.7) | |
| Smoking status | 0.500 | ||
| Yes | 6 (46.2) | 7 (53.8) | |
| No | 69 (50.4) | 68 (49.6) | |
| Father smoker | 0.279 | ||
| Yes | 19 (55.9) | 15 (44.1) | |
| No | 56 (48.3) | 60 (51.7) | |
| Brother smoker | 0.220 | ||
| Yes | 20 (51.1) | 15 (42.9) | |
| No | 55 (47.8) | 60 (52.2) | |
| Friends smoker | 0.145 | ||
| Yes | 27 (57.4) | 20 (42.6) | |
| No | 48 (46.6) | 55 (53.4) |
a Values are presented as mean ± SD or No. (%).
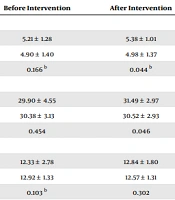
Table 3 compares IMFISB constructs scores before and after the program implementation in the intervention and control groups. The results indicated that the effect size was estimated as "small" for belief, value, and family pressure. The effect size was estimated as “medium" for knowledge, attitude, peer pressure, self-image, and intention. As well as, Table 3 indicates average response for smoking prevention behaviors was 15.17, which significantly increased to 16.88 after program implementation among the intervention group. The effect size for smoking prevention behaviors was estimated to be "medium." As shown in Table 3, the program performance significantly increases the score of attitude, value, family pressure, peer pressure, intention, and smoking preventive behaviors among intervention group students without significantly improving the knowledge and belief scores.
| Constructs | Before Intervention | After Intervention | Paired Sample t-Test | Effect Size |
|---|---|---|---|---|
| Knowledge | ||||
| Intervention group | 5.21 ± 1.28 | 5.38 ± 1.01 | 0.329 | 0.33 |
| Control group | 4.90 ± 1.40 | 4.98 ± 1.37 | 0.742 | Medium |
| Independent t-test | 0.166 b | 0.044 b | - | |
| Attitude | ||||
| Intervention group | 29.90 ± 4.55 | 31.49 ± 2.97 | 0.007 | 0.32 |
| Control group | 30.38 ± 3.13 | 30.52 ± 2.93 | 0.795 | Medium |
| Independent t-test | 0.454 | 0.046 | - | |
| Belief | ||||
| Intervention group | 12.33 ± 2.78 | 12.84 ± 1.80 | 0.184 | 0.17 |
| Control group | 12.92 ± 1.33 | 12.57 ± 1.31 | 0.084 | Small |
| Independent t-test | 0.103 b | 0.302 | - | |
| Value | ||||
| Intervention group | 12.41 ± 2.83 | 13.20 ± 1.93 | 0.043 | 0.08 |
| Control group | 12.92 ± 1.34 | 13.06 ± 1.33 | 0.541 | Small |
| Independent t-test | 0.165 b | 0.624 | - | |
| Family pressure | ||||
| Intervention group | 9.28 ± 1.38 | 9.69 ± 0.65 | 0.022 | 0.04 |
| Control group | 9.56 ± 1.05 | 9.66 ± 0.64 | 0.432 | Small |
| Independent t-test | 0.165 b | 0.802 | - | |
| Peer pressure | ||||
| Intervention group | 8.22 ± 1.89 | 8.85 ± 1.14 | 0.022 | 0.34 |
| Control group | 8.10 ± 2.07 | 8.33 ± 1.92 | 0.447 | Medium |
| Independent t-test | 0.712 | 0.047 b | - | |
| Self-image | ||||
| Intervention group | 15.60 ± 3.22 | 17.33 ± 2.39 | < 0.001 | 0.32 |
| Control group | 16.56 ± 3.32 | 16.45 ± 2.98 | 0.822 | Medium |
| Independent t-test | 0.075 | 0.048 | - | |
| Intention | ||||
| Intervention group | 8.57 ± 1.77 | 9.36 ± 1.33 | 0.002 | 0.34 |
| Control group | 8.82 ± 1.51 | 8.89 ± 1.49 | 0.765 | Medium |
| Independent t-test | 0.348 | 0.045 | - | |
| Smoking preventive behaviors | ||||
| Intervention group | 15.17 ± 3.35 | 16.88 ± 2.23 | < 0.001 | 0.37 |
| Control group | 15.65 ± 3.46 | 15.92 ± 2.87 | 0.585 | Medium |
| Independent t-test | 0.390 | 0.024 b | - |
a Values are presented as mean ± SD unless otherwise indicated.
b Levene’s test showed inequality of variances and a significant report was made.
5. Discussion
The current study aimed to determine the effects of an application smartphone program on smoking prevention among college students. Results revealed that program intervention participation increased determinants of IMFISB after implantation among the intervention group. This result highlighted the success of theory-based mhealth programs regarding smoking prevention of individuals in short-term interventions.
A significant change was observed in the intervention group’s mean score of attitude and value. In line with the present results, Mirzaei Alavijeh et al., in their research among Iranian medical college students, indicated the intervention programs’ usefulness in reducing attitudes toward drug use (15). Furthermore, Jalilian et al. performed a web-based education intervention and reported that the e-intervention had a practical approach to addressing the attitude toward alcohol drinking in university students (16). Doumas et al. (22) also confirmed the usefulness of web-based interventions regarding reducing positive attitudes toward alcohol consumption. On the other hand, the evidence indicates that increasing the negative attitude towards substance abuse can be an effective strategy in preventing and reducing substance abuse (23, 24). Positive and negative beliefs about smoking can be promoted in programs to reduce smoking. This study and other studies confirmed the usefulness of mhealth programs in increasing negative beliefs about smoking. Implementing programs to promote negative thoughts about smoking is suggested to health policymakers in universities, especially for students upon entering the university.
Another result of this study was the efficacy of the implemented program in promoting family and pressure about smoking prevention behaviors among students. Several studies have found the effectiveness of interventions toward smoking prevention by targeting peers (25-27). Family and peer pressure are strong predictors of smoking (28, 29). The educational interventions addressing peer and family pressure were much more important to include in educational interventions because friend pressure could be a significant motivator for starting tobacco use.
Regarding self-image, this intervention increased the self-image score of the intervention compared with the control group. The results supported Junnual et al. in Thailand (30). The effectiveness of educational interventions on self-image might vary, counting on individuals’ characteristics and educational interventions’ nature. Thus, interventions should be tailored to the individual’s needs, and ongoing support should be provided to maintain good changes in self-image in the future.
In addition, the results indicated the significant effect of the implemented educational intervention on promoting the intention of smoking prevention behaviors among students. These results are consistent with other studies (15, 31). Ajzen believes behavioral intention is the main predictor of behavior (32). Considering the usefulness of educational interventions on behavioral intention, providing these interventions can lead to valuable findings in preventing smoking.
Finally, smoking prevention behaviors significantly improved among students in the intervention group. Evidence-based mhealth interventions can confirm the efficacy of health promotion programs. Several studies have shown the usefulness of mhealth interventions in preventing high-risk behaviors such as smoking, substance abuse, and alcohol consumption (33-36). Moreover, Moore et al. reported that the smoking abstinence rate in these interventions was generally 1.5 times higher than the control group (37). These studies have revealed that mhealth educational programs can enhance the mean scores of smoking preventive behavior. Therefore, smoking preventive behavior can be changed and strengthened through educational intervention programs. A course should be implemented in the curriculum of Iraqi Kurdistan universities on the control of tobacco use and the impact of prevention and smoking cessation on well-being, especially in the first year of entering the university for students.
5.1. Limitations
This study had some limitations, including the self-report data collection, which could be accompanied by social desirability or recall biases, and the data collection was only among students in Raparin University, which cannot be generalized to other universities in the Kurdistan region of Iraq. Despite these limitations, the current study illustrates magnificent information because, to the best of our knowledge, this study was the first study in the Kurdistan of Iraq using a smartphone application based on IMFISB to prevent smoking among college students.
5.2. Conclusions
Smartphone application intervention regarding smoking prevention was feasible and enhanced students’ constructs of IMFISB. Thus, implementing prevention programs in a larger population could be significant to protect, strengthen, and prevent the prevalence of tobacco use among university students.