1. Background
Type 1 and type 2 are the two primary forms of diabetes, and Type 1 diabetes is a complicated chronic condition that causes severe physical, psychological, and clinical complications for patients (1). In addition, Type 1 diabetes is a metabolic disorder characterized mainly by the body’s inability to produce and secrete insulin. This condition is caused by an autoimmune disorder in the β-cells of islets of Langerhans in the pancreas. The most common age of onset for type 1 diabetes is adolescence (2, 3). The failure of the pancreas to produce sufficient insulin or the body’s cells and lack of response effectively to the secreted insulin in type 2 diabetes is primarily observed in adults over 30 (4). Diabetes prevention and care programs have been practiced in many industrial countries for years (5). Given the upward trend in the prevalence of this disease in developing countries, some of these countries have recently taken specific measures to control diabetes (6). There are more than 5.3 million patients with diabetes in Iran, where studies indicate that one in five adults (over 30 years old) is at risk of developing diabetes (7).
Diabetes impacts all aspects of a patient’s life, so it can undoubtedly disrupt their quality of life (QoL) and does not have the same impact on patients worldwide (1). According to studies, the direct costs of diabetes treatments account for nearly 14% of the total healthcare costs. This study aimed to improve health and QoL among patients with diabetes to reduce the social and personal costs of diabetes care (8). Generally, people with a particular disease experience lower QoL than healthy individuals. Improving a patient’s physical health without considering their QoL is difficult, especially in non-communicable chronic conditions (9). Diabetes is a non-communicable chronic disease worldwide and a significant cause of low QoL (10, 11). Health-related quality of life (HRQoL) is an individual’s perception of how a disease, disability, or disorder affects them physically, psychologically, and socially. The ultimate goal of diabetes treatment is to enhance QoL even if clinical indices depict a good estimation of the disease control (12).
Interoceptive awareness is an influential factor in the QoL of patients with diabetes, which refers to the ongoing perception and awareness of sensations within the body. Interoceptive awareness is a process whereby the brain senses and integrates the signals from the internal organs for the real-time mapping of intrinsic operations (13, 14). The human body responds to different stimuli inside and outside the environment at any specific point of the day. The human body has eight sensory systems: Visual, auditory, tactile, gustatory, olfactory, vestibular, proprioception, and interoception. The sensory inputs of these systems are essential to developing the human body as they form the brain structure, affect brain functions, and create adaptive responses (15). Interoceptive awareness for moderating avoidance behaviors and approaches can help us maintain and regain hemostasis, i.e., adjusting the internal state of our bodies (16). The experienced senses within the body give individuals some indices to interpret feelings. Sensations from inside the body can help encrypt feelings. The inaccurate interpretation of body sensations leads to the misinterpretation of emotional states and maladaptive environmental responses (17). Interoceptive awareness is considered a significant mechanism of mindfulness interventions, and studies have shown that chronic pains can reduce the levels of interoceptive awareness (18).
Lack of treatment adherence is one of the significant challenges in managing diabetes and controlling the QoL among patients. Patients’ self-care behaviors, diabetes management, lifestyle, and therapeutic adaptability are influenced by the physical, psychological, and social burdens of diabetes, which ultimately affect the QoL in the affected population (19). However, patients with diabetes fail to adhere to therapeutic instructions 23 - 93% of the time, resulting in twice as many fatalities as those who follow treatment (20). Generally, the inability to perform physical tasks due to complications or feelings of anxiety or depression caused by high glycemia can reduce HRQoL in patients with diabetes. Hence, it is essential to perceive the effects of diabetic complications on HRQoL to develop more efficient treatment plans for patients with diabetes since higher QoL can mitigate the risk of diabetes.
2. Objectives
Based on the abovementioned issues, the present study aimed to investigate the mediating role of adherence to treatment in the relationship between interoceptive awareness and QoL in patients with diabetes.
3. Methods
This descriptive-correlational study used the structural equation modeling (SEM) technique to analyze the relationships of variables. The statistical population included all patients with diabetes visiting health centers of Ahvaz, Khuzestan Province (Iran) in 2022, who were selected by the convenience sampling method. According to Loehlin and Beaujean (21), an SEM sample should include 220 participants, but 250 participants were selected due to the risk of attrition. Finally, a total of 232 participants were included after removing defective forms. The inclusion criteria were a history of a definite diagnosis of diabetes for at least two years, having a middle school education to understand the items of research questionnaires, the absence of acute or chronic mental disorders, and the absence of psychiatric medication. The exclusion criteria included unwillingness to continue the study and failure to complete all questionnaire items. This study was approved by the university’s ethics committee with code IR.IAU.AHVAZ.REC.1401.008. Patients with diabetes were assured that their data would remain confidential. Written informed consent was also obtained from participants.
3.1. Measures
Diabetes Quality of Life–Brief Clinical Inventory: This 15-item questionnaire for patients with type 1 and 2 diabetes was designed by Burroughs et al. (22). The items of this questionnaire are divided into two dimensions: Caring behaviors of patients and satisfaction with disease control. This 15-item questionnaire is scored on a five-point Likert scale ranging from 1 for “very satisfied” to 5 for “very unsatisfied,” and the total score varies between 15 and 75. Higher scores indicate patient dissatisfaction with QoL. The reliability of the Persian version of Diabetes Quality of Life–Brief Clinical Inventory was reported as 0.75 using Cronbach’s alpha (23).
Multidimensional Interoceptive Awareness Scale: This multidimensional 32-item scale includes eight subscales: (1) Noticing: Awareness of pleasant, unpleasant, and neutral body sensations; (2) not-distracting: Emotional reaction and attentional response to body sensations like pain or illness; (3) not-worrying: Not worrying or experiencing emotional distress in response to body pains or ill health; (4) attention regulation: The ability to control and maintain attention to body sensations; (5) emotional awareness: Awareness of mind-body integration; (6) self-regulation: Ability to regulate distress concerning body sensations; (7) body listening: Attention to and listening actively to the body to gain insight; (8) trusting: Trusting experience of body sensations. This 32-item scale is scored on a six-point Likert scale ranging from 0 for “never” to 5 for “always,” and the total score varies between 0 and 160 (24). The reliability of the Persian version of the Multidimensional Interoceptive Awareness Scale was reported (0.83) using Cronbach’s alpha (25).
Morisky Medication Adherence Scale (MMAS-8): This questionnaire was designed by Morisky et al. (26). The scale items are easy for participants to understand. This scale is often administered to populations with low levels of literacy. The MMAS-8 consists of seven two-choice yes/no questions and a single Likert scale question. The total score of this scale ranges from 0 to 8, and lower scores indicate higher levels of medication adherence. The reliability of the Persian version of MMAS-8 was reported as much as 0.70 using Cronbach’s alpha (27).
3.2. Statistical Analyses
The Pearson product-moment correlation coefficient and the SEM technique were employed to analyze the relationships of variables and evaluate the proposed model, respectively, in SPSS 27 and AMOS 25 software. Moreover, the indices, including normalized chi-square (χ2/df), normalized fit index (NFI), comparative fit index (CFI), incremental fit index (IFI), Tucker–Lewis’s index (TLI), and root mean square error of approximation (RMSEA) were used to evaluate the fitness of the model.
4. Results
The demographic findings revealed that the mean age of patients was 38.15 (± 4.60) years old, and the mean duration of the disease in the participants was 7.64 (± 1.37) years. There were 105 (45.26%) female and 127 (54.74%) male patients, of whom 113 (48.71%) individuals were single, whereas the other 119 (51.29%) were married. Table 1 reports the means, standard deviations, and Pearson’s correlation coefficients of the research variables.
| Variables | Mean ± SD | 1 | 2 | 3 |
|---|---|---|---|---|
| 1- Quality of life | 44.26 ± 16.00 | 1 | ||
| 2- Interoceptive awareness | 79.54 ± 9.41 | 0.16* | 1 | |
| 3- Adherence to treatment | 3.81 ± 2.52 | 0.48** | 0.28** | 1 |
Means, Standard Deviations, and Pearson’s Correlation Coefficient of the Research Variables a
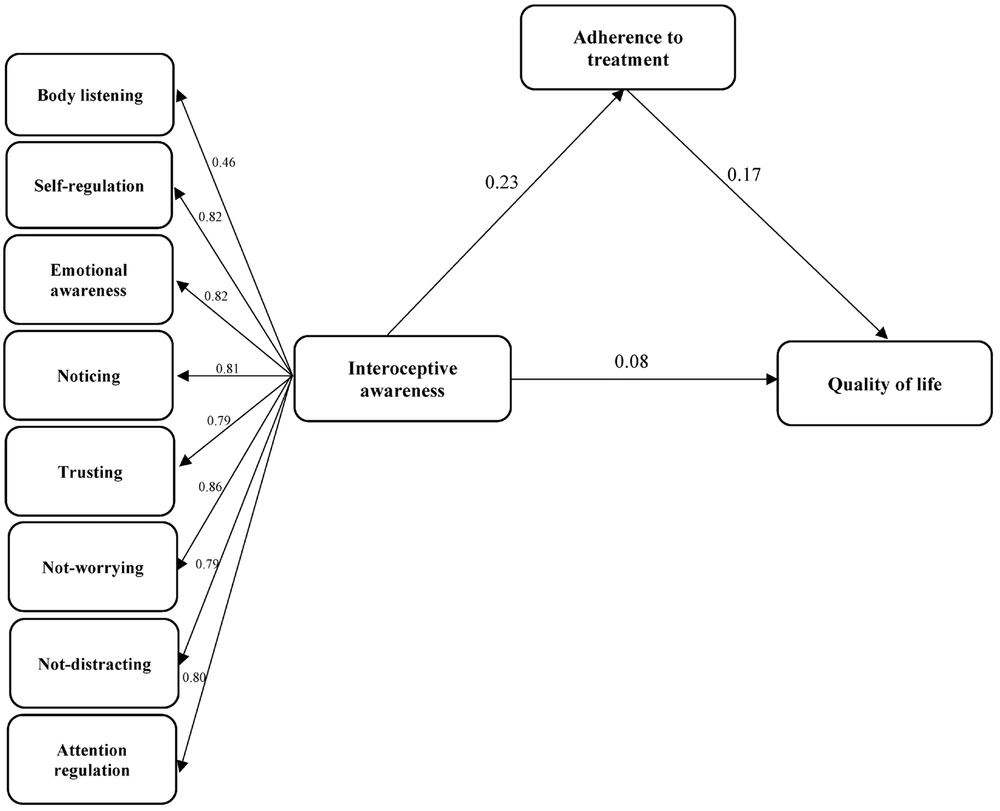
As shown in Table 1, Pearson’s correlation coefficients indicate significant relationships between all research variables. Figure 1 depicts an initial model proposed to explain the QoL based on interoceptive awareness and adherence to treatment.
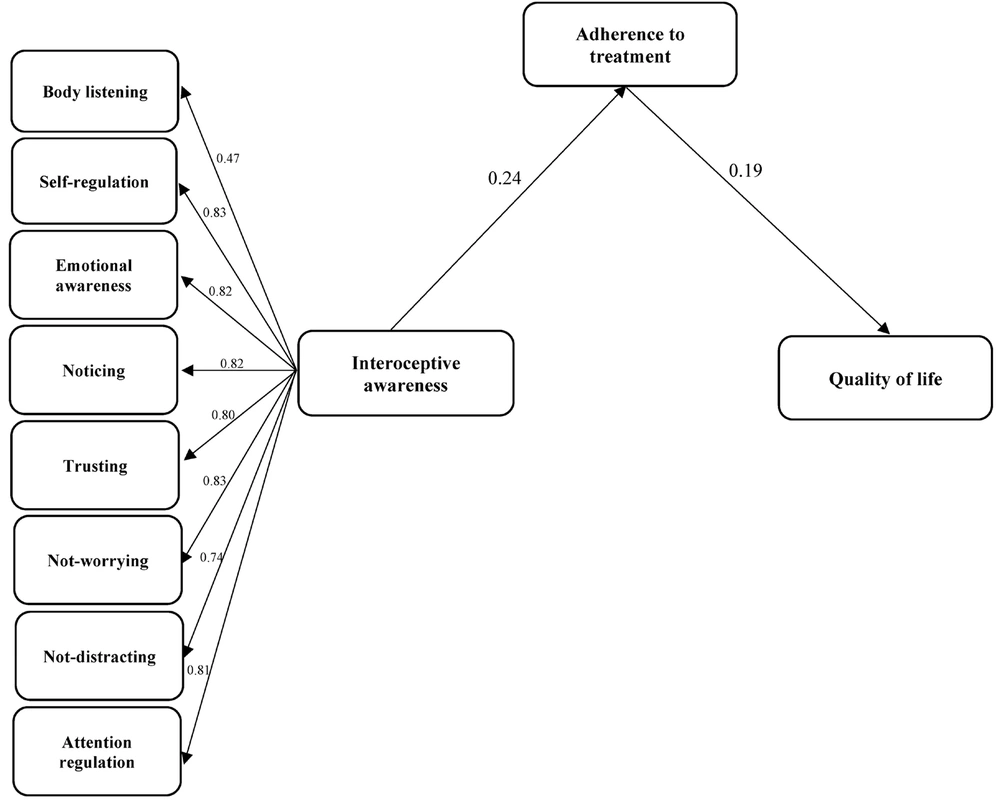
According to Table 2, the root mean square error of approximation (RMSEA = 0.107) indicates that the proposed model did not fit the data well and needed revision. In addition, all fit indices, such as the χ2/df, NFI, CFI, IFI, TLI, and RMSEA, indicated the acceptable fit of the final model to the data. RMSEA in the modified final model was 0.076. Figure 2 demonstrates the revised model.
| Variables | χ2 | df | (χ2/df) | TLI | CFI | IFI | NFI | RMSEA |
|---|---|---|---|---|---|---|---|---|
| Fit indicators | ||||||||
| Initial model | 123.11 | 34 | 3.62 | 0.90 | 0.93 | 0.87 | 0.90 | 0.107 |
| Final model | 79.29 | 34 | 2.33 | 0.95 | 0.96 | 0.92 | 0.94 | 0.076 |
The Fit Indices of the Initial and Final Models
Table 3 represents the estimation of path coefficients for the analysis of direct and indirect relationships. For this purpose, the interoceptive awareness-QoL relationship was excluded. There was a direct and significant relationship between interoceptive awareness and adherence to treatment (β = 0.24, P = 0.001) and between adherence to treatment and QoL (β = 0.19, P = 0.003) in patients with diabetes.
The bootstrap method was employed to determine the significance of moderating relationships. Table 3 indicates the significance of an indirect path from interoceptive awareness to QoL mediated by adherence to treatment in patients with diabetes (β = 0.27, P = 0.024).
| Path | Initial Model | Final Model | ||
|---|---|---|---|---|
| β | P | β | P | |
| Interoceptive awareness → Quality of life | 0.08 | 0.246 | - | - |
| Interoceptive awareness → Adherence to treatment | 0.23 | 0.001 | 0.24 | 0.001 |
| Adherence to treatment → Quality of life | 0.17 | 0.010 | 0.19 | 0.003 |
| Interoceptive awareness → Quality of life through the mediating role of adherence to treatment | 0.24 | 0.043 | 0.27 | 0.024 |
Path Coefficients of Direct and Indirect Relationship Between Research Variables
5. Discussion
The present study aimed to evaluate the mediating role of adherence to treatment in the relationship between interoceptive awareness and QoL in patients with diabetes. The results indicated no significant relationships between interoceptive awareness and QoL in patients with diabetes. This result is inconsistent with Yagci et al. (28), who found a relationship between interoceptive awareness and QoL in patients with spinal deviation. This study analyzed the relationship between interoceptive awareness and QoL through the correlation coefficient test and was significant. However, the research hypotheses were tested through path analysis in this study, where a significant relationship was found between interoceptive awareness and QoL in the Pearson test. The contribution and effect of adherence to treatment on QoL were explained through the mediating variable or the indirect relationship in patients with diabetes. In other words, interoceptive awareness indirectly affected QoL in this model.
Generally, interoceptive awareness refers to awareness and attentional response to the body’s internal state. This awareness includes paying attention to physical signals, feelings, strengths and weaknesses, and functions of different body systems, such as glycemia. According to previous studies, interoceptive awareness improves symptoms in the human digestive system, fatigue, anxiety, depression, and stress (13). Studies have also emphasized how this relationship improves QoL in patients with diabetes (28). Different exercises such as mindfulness, meditation, and yoga can help boost interoceptive awareness, which can also help reduce stress and anxiety, improve sleep and concentration, and enhance awareness of body needs. Therefore, interoceptive awareness can help patients with diabetes significantly improve QoL. Patients can identify their health problems and make the right decisions to manage diabetes by increasing their awareness of body signals.
The results indicated a significant relationship between adherence to treatment and QoL, consistent with the results of Majeed et al. (29). Majeed et al. (29) reported that good QoL in patients with diabetes was significantly associated with treatment adherence. In other words, treatment adherence had a positive significant relationship with QoL, which can be explained by the notion that adherence to treatment in patients with diabetes can have considerable effects on disease progression and QoL. Treatment adherence refers to compliance with the instructions provided by doctors and nurses about disease management, which includes the regular use of medications, a good diet, regular physical activity, and medical tests and consultations (30). Since diabetes affects a patient’s daily routine, the detrimental outcomes of inaccurate treatment designs can lead to severe risks. In addition, noncompliance with treatment results in new complications such as lethargy, muscular weakness, heart failure, and other conditions, increasing treatment costs and hospitalization rates (30). Therefore, compliance with treatment can significantly affect QoL, and failure to properly control blood sugar levels and diabetic complications (e.g., sexual impotence, psychological disorders, and decline in the ability to do daily activities) may reduce QoL.
This study showed a significant relationship between interoceptive awareness and QoL mediated by adherence to treatment. The researcher found no similar studies on this finding. The first hypothesis revealed that interoceptive awareness had no significant relationship with QoL. However, interoceptive awareness improved the QoL in patients with diabetes indirectly as adherence to treatment increased. Generally, QoL has an axial role in the lives of patients with chronic conditions, especially those with diabetes. Some experts have regarded improving the patient’s QoL as the treatment goal (12). Quality of life is a multidimensional construct concerning physical, cognitive, social, emotional, psychological, and spiritual aspects of a person’s life. Nonetheless, the QoL in patients with diabetes is considered an acceptable self-care outcome compared with the general population (19).
5.1. Limitations
Since the statistical population of this study included only patients with diabetes from Ahvaz, Iran, the results should be generalized to other patients with chronic conditions in other cities with caution. Another research limitation was using a self-report tool, which might have led to biased social utility in participants and affected their reports. Hence, future studies are recommended to control other influential variables such as gender, age, and duration of diabetes. The results can then be compared with the findings of this study.
5.2. Conclusions
Based on the results, there was a relationship between adherence to treatment and QoL in patients with diabetes. Moreover, the indirect path between these variables was significant through treatment adherence. The final revised model also had a good fit and can be considered a step forward in improving QoL in patients with diabetes. Given the research results, specific training can be provided for patients with diabetes to improve their QoL, enhance treatment adherence, and boost their interoceptive awareness. Medical planners and advisors should pay more attention to adherence to treatment and interoceptive awareness since both are acquired skills, and they can use mass media to teach such skills to patients with diabetes and other chronic conditions.