1. Background
Physical and psychological problems are among the effects of war for people who were directly present in the war. Physical problems usually lead to disability, but psychological injuries remain with the victims for a long time, even after the war. The injured person is psychologically disturbed, and their family is also at risk as the outcome (1, 2).
War is one of the influencing factors on the amount of prevalence, the time of onset, and the process of creating mental disorders. Due to the tensions caused by the war and its destructive effects on the soul and psyche of the person returning from the war, the adverse effect of the war on the family, especially the wife, continues for a long time after the war. According to the reports of the World Health Organization, 65% of patients with mental disorders live with their families (3, 4).
Post-traumatic stress disorder (PTSD) is one of the psychological consequences for people exposed to war. The lifetime prevalence of PTSD is about 8% (10 - 12% in women and 5 - 6% in men). In addition, the majority of diseases associated with PTSD are high, and about two-thirds of patients have at least two other disorders (5). In research based on the records and diagnoses included in the records of the veterans, more than 80% of them had PTS, and the severity of the symptoms that appeared in them ranged from "weak" to "very severe" (6, 7).
As one of the complications of war, PTSD has adverse effects on the families and spouses of war victims. Spouses of veterans with PTSD are considered indirect victims of war (1) because they experience high psychological stress. Some studies have indicated that most spouses of veterans suffer from PTSD symptoms because he/she is the only family member who suffers from many emotional and nervous problems due to frequent contact with the affected person throughout his/her life. In addition, in the long term, family functioning is disrupted and causes common problems such as shame, guilt, and mistrust, as well as negative effects on interpersonal relationships and decreased intimacy in the family (8).
Self-efficacy means a special ability to take care of oneself, which increases health and adaptability to life pressures (9). Self-efficacy plays an important role in stress reduction of spouses of veterans with PTSD (10).
Numerous research studies have shown that the most effective educational programs are those based on theory-based approaches rooted in behavior change patterns (11, 12). The use of models and theories of behavior change increases the possibility of increasing the effectiveness of health education programs and helps to identify individual and environmental characteristics. In addition, it is essential to use theories and patterns of behavior change to promote health (12-15).
2. Objectives
The main aim of the present study was to evaluate the effect of the extended parallel process model (EPPM) on the self-efficacy of spouses of veterans with PTSD.
3. Methods
3.1. Sampling
This study is semi-experimental, with two control and intervention groups with a pre-test and post-test design. The type of intervention, the training, and the method of implementation of the intervention were held in six sessions; the training was based on the Extended Parallel Process Model, and each session was 30 to 40 minutes. Exclusion criteria included addiction or unwillingness to participate in the present study. For this research, G*Power statistical software (16) with an effect size of 0.95, test power equal to 80%, and significance level = 0.05, the sample size was estimated to be 30 people, which were selected randomly and divided into two groups (15 persons for each group).
3.2. Data Collection Tools
The demographic questionnaire and parenting self-agency measure (PSAM) questionnaire were used in this research collection of information. A demographic questionnaire was used to assess the respondents' age, duration of marriage, number of children, spouse's military service percentage, education level, and employment status. The PSAM questionnaire consists of 10 questions; each question's answers are graded on a Likert scale from 1 (completely disagree) to 7 (completely agree). In the case of adding up the scores, if the total score is equal to 10 to 20, 20 to 40, and above 40, it is considered as "low," "medium," and "high" self-efficacy, respectively. The validity and reliability of this questionnaire have already been confirmed by Motahari and Hojjati , and Cronbach's alpha for the reliability of this questionnaire was reported as 0.82 (17).
3.3. Implementation of the Study
At first, the research objectives and steps were explained to all the study participants, and then they were assured the confidentiality of the research results. All the participants were informed that if they did not want to continue, they could withdraw from this research even during the implementation of the study. The participants were divided into control and intervention groups using random allocation (15 people in each group). Six training sessions of 30 to 40 minutes for the intervention group were conducted based on the EPPM method (18). No intervention was performed for the control group.
3.4. Statistical Analysis
Shapiro-Wilk Test evaluated the normality of the primary results of this research. Then, the raw results obtained by SPSS-ver. 21 statistical software using descriptive statistics (including cross table, mean, and standard deviation) and inferential statistics (including paired-samples t-test, independent samples t-test, ANOVA, ANCOVA) were analyzed at a significance level of 0.05.
4. Results
The results showed that the average age of the study groups, including the control group and the group trained with EEPM, was 48.1 ± 4.1 and 52.1 ± 5.4 years, respectively. The frequency of participants in the study related to the control group regarding education level, including secondary education, diploma, and university education, was equal to 5 (33.3%), 5 (33.3%), and 7 (46.7%), respectively. These values for the group trained with EPPM were equal to 7 (46.7%), 5 (33.3%), and 3 (20%), respectively (Table 1). Other characteristics of the study participants in terms of other demographic parameters, including job type, number of children, percentage of husband's veterans, hospitalization history of husband, and underlying disease, are shown in Table 1.
| Variables | Study ‘Groups | |
|---|---|---|
| CG | EPPG | |
| Age (y) | 48.1 ± 4.1 | 52.1 ± 5.4 |
| Level of education | ||
| Secondary education | 3 (20) | 7 (46.7) |
| Diploma | 5 (33.3) | 5 (33.3) |
| University education | 7 (46.7) | 3 (20) |
| Job type | ||
| Housewife | 3 (20) | 9 (60) |
| Employee | 8 (53.3) | 4 (26.7) |
| Freelance job | 4 (26.7) | 2 (13.3) |
| Number of children | 1.6 ± 0.5 | 1.86 ± 0.51 |
| Percentage of husband’s veterans | 29.7 ± 8.9 | 33.0 ± 8.9 |
| Underlying disease? | ||
| Yes | 9 (60) | 9 (60) |
| No | 6 (40) | 6 (40) |
| Hospitalization history of husband | ||
| Yes | 3 (20) | 5 (33.3) |
| No | 12 (80) | 10 (66.7) |
The Demographic Characteristics of Study Participants a
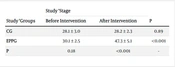
The study results showed that the self-efficacy of the intervention among the two study groups was not significantly different from each other. At the same time, this difference was significant after the intervention (Table 2). Based on the findings of the present study, it was found that the intervention by EPPM had a significant effect on the self-efficacy of spouses of veterans with PTSD (Table 2).
| Study ‘Groups | Study ‘Stage | P | |
|---|---|---|---|
| Before Intervention | After Intervention | ||
| CG | 28.1 ± 3.0 | 28.2 ± 2.3 | 0.89 |
| EPPG | 30.1 ± 2.5 | 47.3 ± 5.1 | <0.001 |
| P | 0.18 | <0.001 | - |
The Effect of EPPM on Self-efficacy of Spouses of Veterans with PTSD
The covariance test showed a significant difference by removing the effect of the pre-test (P<0.01 and Eta=0.81) so that 81% of the post-test changes can be related to the intervention (Table 3).
| Factors | Sum of Squares | Degrees of Freedom (DF) | Mean of Squares | F Value | P Value | Eta |
|---|---|---|---|---|---|---|
| Modified model | 3553.57 | 2 | 1184.24 | 79.1 | < 0.01 | 0.85 |
| Post-test separator | 228.32 | 1 | 328.7 | 22.73 | < 0.01 | 0.35 |
| Group | 2615.1 | 1 | 1307.58 | 87.35 | < 0.01 | 0.81 |
| Error | 613.7 | 31 | 16.89 | - | - | - |
| Sum | 77049 | 30 | - | - | - | - |
| Total | 4166.4 | 29 | - | - | - | - |
The Results of the ANCOVA Test to Evaluate the Effect of EPPM on the Self-efficacy of the Spouses of Veterans with PTSD
5. Discussion
The findings showed that the effect of EPPM on the self-efficacy of spouses of veterans with PTSD was significant, so the level of self-efficacy in the group under EPPM, more than in the control group, increased significantly after the intervention. The results of most similar studies in the past were consistent with the present study. Zamani et al. showed that EPPM increased the self-efficacy of diabetic adolescents (18). Sarbanan et al. reported that increasing self-efficacy reduces stress and increases adaptation in spouses of veterans with PTSD (19). The findings of the study of Parsaee et al. revealed that using educational models and theories, especially EPPM, as a low-cost but effective educational method plays an important role in increasing compliance with the drug treatment of diabetic patients (20).
The burden of care can affect the quality of care and cause the severity of the disease in the patients themselves. Therefore, it is suggested that medical professionals use suitable educational models to reduce the burden of care and increase self-efficacy in the families of veterans with PTSD. The results of some similar studies align with the present study's findings. Dalir et al. examined the effect of spiritual self-care training on the care burden of mothers with children hospitalized in intensive care units for open heart surgery (21). The amount of care burden on caregivers was high. After training in spiritual self-care, the care burden of caregivers decreased to a moderate level (21). Bamari et al. evaluated caregivers' burden of patients with type 2 diabetes referred to a diabetes clinic in Zabol, Iran. The research results showed that the care burden score of companions was reported at a moderate level (22), while the care burden in the present study was declared at a high level.
Caregivers of different patients may be exposed to various mental and psychological injuries due to the pressure and stress caused by caregiving. Differences in the results of various studies can be due to differences in culture, race, geographical location, and differences in the target group (23). Sanaei and Nasiri found that spiritual and religious content create a positive attitude towards oneself, the environment, and the future due to their many positive consequences. Therefore, people do not consider themselves vulnerable and feel relaxed in the environment (24). In addition, spirituality helps him evaluate negative events in better ways and have a stronger sense of control over existing conditions by targeting a person's beliefs. However, the feeling of control makes people extremely powerful in coping with life conditions, improving their mental health, and reducing stress (25). Falah et al. expressed the effect of spiritual intervention on reducing the tension and anxiety of these people and increasing their general health overall (26). Reyhani et al. exhibited that distress tolerance increased significantly after training spiritual self-care mothers compared to before the intervention (25). Spiritual self-care is considered the most essential form of self-care and includes all physical, mental, and emotional dimensions (27). Rashidzadeh et al. indicated that spirituality and religious beliefs can improve the well-being and psychological well-being of mothers with autistic children and increase their resilience (28). In addition, the findings of some previous studies have shown that religious coping has a direct relationship with resilience (29, 30). In explaining the results of the present study, one of the ways that spirituality can increase effectiveness is that spirituality improves the ability to analyze and solve problems better by increasing positive characteristics such as promoting patience and tolerance in the face of issues and difficulties at work. People with spirituality can find suitable solutions to problems and issues in life and show more resilience (31) because spirituality is one of the main axes of knowing God correctly and having a purpose and meaning in life, which is a prelude to resilience and adaptability to problems.
5.1. Limitations
Due to the difficulty of accessing the spouses of veterans, a small sample size was selected, which was one of the main limitations of the present study. The difficult access to the spouses of veterans and their complex participation in the implementation of the study were other limitations of the present study.
5.2. Conclusions
Based on the results, the Extended Parallel Process Model (EPPM) had a significant and positive effect on the self-efficacy of spouses of veterans with post-traumatic stress disorder (PTSD). Based on the findings, the use of the models mentioned above improves the care management of veterans with PTSD by their spouses. Therefore, it is suggested that the models above be continuously implemented and planned for veterans' spouses.