1. Background
Post-traumatic stress disorder (PTSD) is the last group of anxiety disorders. In this disorder, the person suffers from mental problems caused by a bitter and severe incident. Post-traumatic stress disorder includes the set of reactions that humans show when faced with stress beyond their tolerance level, such as war, aggression, accidents, and natural disasters (1). The events that cause this disorder are so debilitating that a person with this disorder can face many psychological problems (2). Post-traumatic stress disorder is one of the chronic diseases that manifests in the form of increased arousal, avoidance, and experience of traumatic events (3). This disorder has a significant impact on a person's life, as it disrupts a person's mental life and social performance and also causes a decrease in the level of psychological health of a person (4). People who suffer from this disorder have characteristics such as low self-confidence, high violence, low correlation with family members and society, and high levels of conflict (5).
According to the research, those who have faced a severe event, such as war, have problems in their executive functions. Functional impairments are common among these patients, as they cannot work independently, care for themselves, and maintain social relationships (6). People with PTSD ignore their bodies, and things like health, treatment, and self-care become worthless to them. Therefore, these kinds of problems cause people with PTSD to be exposed to various risks and injuries. In addition, the lack of self-care in these patients causes problems for people's health and decreases their quality of life (7, 8).
Webber et al. defined self-care as follows, citing the World Health Organization: Self-care is the ability of individuals, families, and communities to promote health and cope with illness and disability (with or without the support of a health care provider). According to the view of Webber et al., the most critical achievement of self-care includes making the right decisions by people about the correct use of healthcare and self-care behaviors (9).
Many reasons make it necessary to use spiritual self-care patterns (SSCP) for patients with PTSD, including war in different countries of the world, the prevalence of PTSD, self-care disorders in these patients, the inability of more than two-thirds of these patients to manage their lives, the loss of jobs of these patients, and the increase in financial burden due to frequent hospitalizations (6-8, 10). The reasons above make paying attention to PTSD of particular importance, and so one can try to improve self-efficacy, resilience, and quality of life for spouses of veterans with PTSD using models and theories of behavior change such as SSCP.
2. Objectives
Considering the importance of SSCP in the stress management of various diseases, the primary purpose of this study was to evaluate the effect of spiritual self-care patterns (SSCP) on the resilience of spouses of veterans with post-traumatic stress disorder (PTSD).
3. Methods
This semi-experimental study was conducted on 30 spouses of veterans with PTSD, who were randomly selected. The statistical population of this study included all spouses of veterans with PTSD in Gorgan, Iran. The total sample size was estimated to be 30 people using the statistical software (G*Power), the effect size = 0.95, the test power = 0.80, and the significance level = 0.05. The selected people were divided into two control groups (15 people) and an experimental group (15 people). The exclusion criteria included addiction or unwillingness to participate in the study. In this study, the experimental group was trained by spiritual self-care pattern (SSCP), which was implemented based on the model of Mary L. White (six training sessions) (11). The discussion method was implemented in each training session for 30 to 40 minutes.
Two questionnaires were used to collect information in this study: The demographic questionnaire and the Conner-Davidson Resilience Scale (CD-RIS) questionnaire. Information related to the demographic variables of the participants in the study, including age, duration of marriage, number of children, spouse's percentage of military service, level of education, and occupation, was collected by a researcher-made demographic questionnaire. The CD-RIS questionnaire had 25 questions and a range of answers with a Likert scale (0 to 4 points). The options for answering the questions included "completely false," "somewhat false," "no idea," "somewhat true," and "completely true." The overall scoring of this questionnaire is from zero to 100 (with an average of 50) (12), and a higher score means higher resilience of the individual (13, 14). The validity and reliability (Cronbach's alpha = 0.82) of the Persian version of this questionnaire, which was previously studied by Ghasemi et al., were confirmed (15).
The raw results were recorded in the SPSS After collecting the data. Relevant statistical tests statistically analyzed 21 statistical software, then the findings at a significance level of α = 0.05.
4. Results
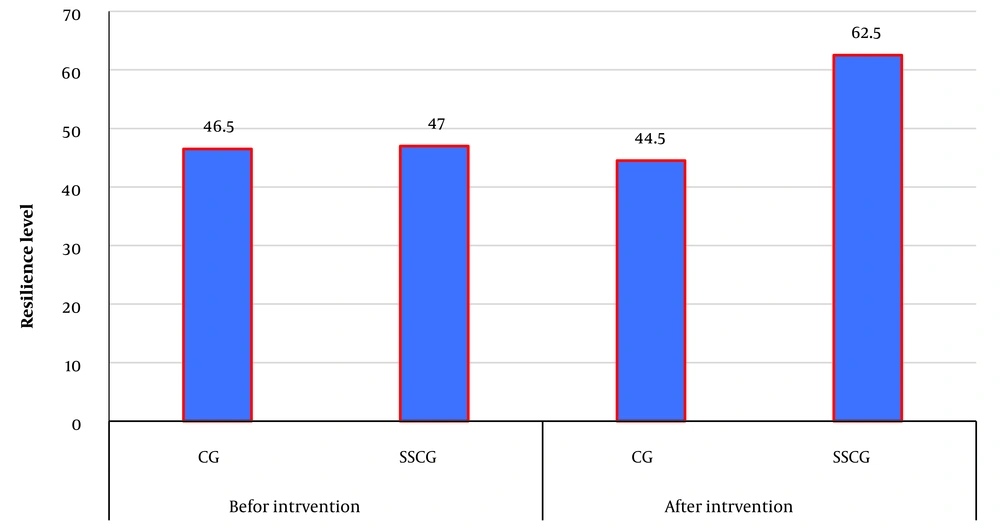
The results related to demographic variables are presented in Table 1. The statistical analysis results for comparing the two groups showed that the resilience level before the intervention between the control and SSCP-trained group was insignificant. In contrast, this difference was significant after the intervention (Table 2). In addition, the findings showed that after the educational intervention with SSCP, the level of resilience of the spouses of veterans with PTSD increased significantly (Table 2 and Figure 1).
| Variables | Groups | |
|---|---|---|
| CG | SSCG | |
| Age (y) | 48.1 ± 4.1 | 50.9 ± 5.7 |
| Level of education | ||
| Secondary education | 3 (20) | 7 (46.7) |
| Diploma | 5 (33.3) | 5 (33.3) |
| University education | 7 (46.7) | 3 (20) |
| Job type | ||
| Housewife | 3 (20) | 8 (53.3) |
| Employee | 8 (53.3) | 6 (40) |
| Freelance job | 4(26.7) | 1(6.7) |
| Number of children | 1.6 ± 0.5 | 1.8 ± 0.77 |
| Percentage of husband’s veterans | 29.7 ± 8.9 | 32.3 ± 7.9 |
| Underlying disease? | ||
| Yes | 9 (60) | 9 (66.7) |
| No | 6 (40) | 5 (33.3) |
| Hospitalization history of husband | ||
| Yes | 3 (20) | 3 (20) |
| No | 12 (80) | 12 (80) |
Abbreviations: CG, control group; SSCG, spiritual self-care group.
Values are presented as No. (%) or mean ± SD.
| Groups | Stages | P-Value | |
|---|---|---|---|
| Before Intervention | After Intervention | ||
| CG | 46.5 ± 5.7 | 47.0 ± 6.2 | 0.70 |
| SSCG | 44.5 ± 3.8 | 62.5 ± 8.8 | < 0.001 |
| P-Value | 0.46 | < 0.001 | - |
Abbreviations: CG, control group; SSCG, spiritual self-care group.
a Values are presented as mean ± SD.
5. Discussion
The mental health of society is dependent on the health of the families. Among these, women have a vital and undeniable role as helpers in family management, emotional support, and psychological security (16). Therefore, a special look at the mental health of women is necessary to help the mental health of the whole society. This research has sought to provide effective solutions for the psychological empowerment of the spouses of veterans according to the valuable teachings of Islam.
The overall results of this study showed that spiritual self-care patterns (SSCP) can increase the level of resilience of spouses of veterans with PTSD, suggesting that SSCP increases the level of resilience in individuals with PTSD by increasing life expectancy and reducing stress. The results of some previous similar studies also showed that the use of SSCP reduces stress and increases the level of general health in patients or their caregivers. Reyhani et al. evaluated the effect of SSCP on the feeling of relaxation of mothers with premature babies hospitalized in the intensive care unit. Spiritual self-care patterns reduces stress and increases distress tolerance in mothers (17). In addition, Bolahri et al. indicated that spiritual intervention reduced the stress, tension, and depression of patients (18), which may be due to the effect of spiritual care on improving conditions and increasing tolerance of these people in stressful times. In this regard, Sanaei and Nasiri believe that spiritual and religious content creates a positive attitude toward oneself, the environment, and the future due to their many positive consequences. Therefore, people do not consider themselves vulnerable and feel relaxed in the environment (19). In addition, spirituality helps him to evaluate negative events better and have a stronger sense of control over the existing situation by targeting a person's beliefs. In addition, a sense of control makes people highly appreciative of coping with life conditions, subsequently improving their mental health and reducing stress (17). The findings of Fallah et al. expressed the effect of spiritual intervention on reducing the tension and anxiety of these people and generally increased their general health (20). Kia et al. reported that the resilience score increased after spiritual therapy, indicating the positive effect of spiritual therapy training in hemodialysis patients (21). In addition, Ebrahimi et al. found a significant and high correlation between spiritual health and resilience in hemodialysis patients (22). Rashidzadeh et al. showed that spirituality and religious beliefs can improve the well-being and psychological well-being of mothers with autistic children and increase their resilience (23). In addition, the findings of some other previous studies showed that religious coping has a direct relationship with resilience (24-26). In explaining the results of the present study, one of the ways that spirituality can increase the effectiveness in patients' quality of life is to increase the positive characteristics in life. These features include the improvement of patience and tolerance against the problems and difficulties of work and the ability to analyze and solve problems better. Spiritual people can find a suitable solution to life's problems and show more resilience (27) because spirituality is a process, one of the main axes of which is knowing God correctly and having a purpose and meaning in life, a prelude to resilience and adaptability to problems.
5.2. Limitations
The difficulty of accessing the families of veterans, the various obstacles in the selection of samples, and the low willingness of the families to participate in the study were the most critical limitations of the present study.
5.2. Conclusions
Based on the results, the training intervention by spiritual self-care pattern (SSCP) could reduce stress and increase the resilience of spouses of veterans with PTSD. Therefore, using SSCP together with other methods can significantly reduce the negative consequences related to the care of veterans with PTSD.