1. Introduction
Autosomal dominant tubulointerstitial kidney disease (ADTKD) is an inherited renal disorder characterized by progressive renal insufficiency, tubulointerstitial nephropathy, and normal urinary sediment (1). Various gene mutations associated have been identified with ADTKD, including uromodulin, renin, mucin-1 (MUC-1), hepatocyte nuclear factor 1β, and SEC61A1 mutations (1-3), which affect the coding of proteins crucial for normal renal function. The clinical presentation of ADTKD is nonspecific and depends on the specific gene mutation (4). Patients with MUC-1 mutations universally progress to chronic kidney disease (CKD) stage (1). The MUC-1 gene is situated on chromosome 1q21, and mutations result from cytosine duplication, leading to a frameshift mutation. The accumulation of abnormal proteins in renal tubular cells is a critical pathogenic factor (1).
Diagnostic criteria for ADTKD include hereditary CKD with an autosomal dominant pattern, affecting clinical and histological features in at least one relative. A definitive diagnosis may not be solely established through kidney biopsy. Alternatively, confirmation of one of the four mutations in the patient or at least one family member is indicative of ADTKD (5).
2. Case Presentation
A 42-year-old police officer participated in swimming competitions for the first time two years ago. Two days after the event, he experienced muscle pain and noticed red urine, and his serum creatinine level was elevated at 3 mg/dL. Then, he was treated with hydration and conservative management, decreasing serum creatinine to 0.8 mg/dL.
Six months later, he engaged in a high-stakes situation involving criminals and traveled a long distance. The following day, he felt unwell and sought intravenous fluid treatment. Several months after this incident, he was admitted to the hospital for a similar incident, and his symptoms included red urine, muscle pain, and decreased urine volume.
The serum creatinine level was 10 mg/dL, while creatine phosphokinase (CPK) and serum electrolytes were within normal ranges. The patient had no history of alcohol intake, tobacco consumption, or drug abuse. Similar symptoms were reported by his 40-year-old brother, a police officer, who experienced red urine and muscle weakness related to work activities. However, his brother's maximum creatinine rise was only 3mg/dL, and his physical examination was unremarkable.
On the first day, blood test results were as follows: Hemoglobin 16.7 g/dL; blood urea 72 mg/dL, serum creatinine 10 mg/dL, serum uric acid 1.8 mg/dL, serum sodium 138 meq/L, serum potassium 4.9 meq/L, serum phosphate 5.5 meq/L, serum calcium 10.5 meq/L, and serum CPK 94 mg/dL. Urinary sediment revealed 3 - 4 RBCs in a high-power field without proteinuria. HIV, HCV, and HBV tests were negative, and hemolytic and rheumatologic assessments were within normal limits. Renal sonogram results were normal, and a biopsy was not performed based on the patient's preference.
Four sessions of hemodialysis were conducted based on his uremic symptoms. When discharging, his blood test results were as follows: Hemoglobin 13.2 g/dL, blood urea 34 mg/dL, serum creatinine 1.2 mg/dL, and electrolyte levels were within the normal range.
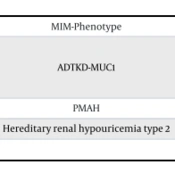
In the genetic analysis, no findings indicated myopathy in either nuclear or mitochondrial forms. The patient DNA sample revealed a homozygous mutation (158340) in the MUC-1 gene on chromosome 1q22 (Table 1).
| Gene | A.A. Change, HGVS | MIM-Phenotype |
|---|---|---|
| MUC-1 | NM-001371720 | ADTKD-MUC1 |
| c.1630A>G | ||
| p. Thr544A1a | ||
| ARMC5 | NM-001105247 | PMAH |
| SLC2A9 | NM-001001290 | Hereditary renal hypouricemia type 2 |
Abbreviations: MUC-1, mucin-1; PMAH, primary macronodular adrenal hyperplasia; ADTKD, autosomal dominant tubulointerstitial kidney disease.
In the follow-up six months later, he reported being in good overall condition with no symptoms during a phone call, even though he had changed his position within the police office.
3. Discussion
A middle-aged man was presented with acute kidney injury (AKI), diagnosed with ADTKD related to MUC-1, exhibiting a positive response to fluid therapy and temporary hemodialysis. The characteristic symptoms of ADTKD related to MUC-1 included an absence of proteinuria or hematuria. The elevation in serum creatinine typically began in middle age and gradually progressed (4, 6). The glomerular filtration rate (GFR) decreases by 10 mL/min per year, leading to the development of CKD in the fifth decade (4, 6-8). In this case, the patient experienced AKI episodes and hematuria, which are not typical symptoms of MUC-1 (9, 10). Mucin-1 patients usually do not present with gout, anemia, or other extra-renal symptoms, confirmed as a pattern in the studies' patients.
Autosomal dominant tubulointerstitial kidney disease is an autosomal dominant inherited disorder, carrying a 50% chance of transmission to the next generation from each affected parent (2). Unfortunately, information on the kidney status of both parents is unavailable due to their demise in previous years. The recommended treatment for ADTKD related to MUC-1 involves a lifestyle modification program, including routine daily mild exercise, avoidance of obesity and smoking, and optimal control of hypertension, dyslipidemia, and hyperglycemia. A kidney transplant is a therapeutic option (5).
In conclusion, ADTKD is a rare disorder with limited information available. Any patient with an unexplained increase in creatinine, whether acute or chronic, should be considered for this test.