Dear Editor,
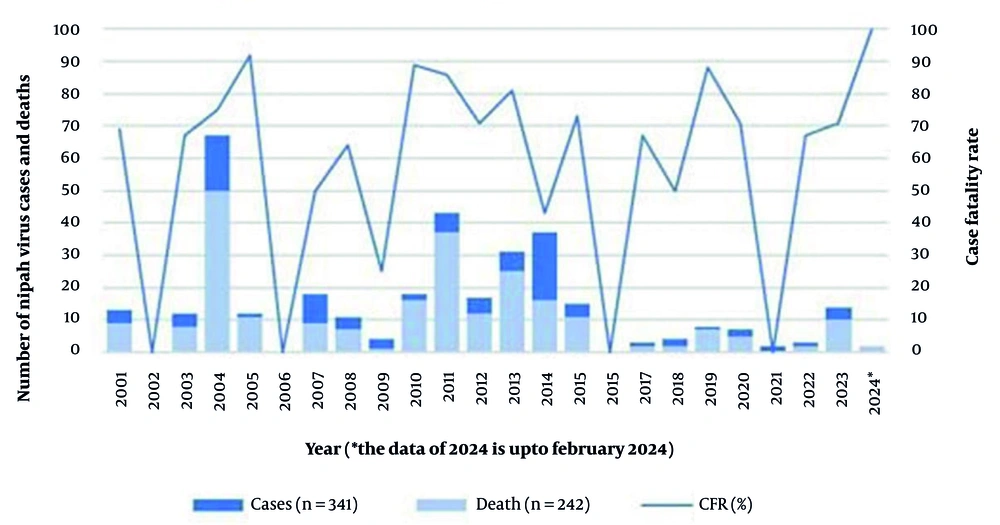
Nipah virus, also known as NiV, is a virus transmitted by fruit bats or flying foxes of the Pteropus genus and belongs to the Henipavirus genus. It was first identified in Malaysia 20 years ago (1). In Bangladesh, seasonal outbreaks of this zoonotic RNA virus have been occurring between December and May since 2001, with a death rate of over 70% (2). In 2023, 14 cases of Nipah virus have already been reported, with 10 fatalities, marking the highest death toll in the past seven years (3). Raw date palm sap contaminated with bat saliva, urine, and excreta is believed to be the primary carrier of NiVs that infect humans. Nipah virus infection causes acute respiratory illness, nausea, fever, headache, sore throat, cough, myalgia, and fainting, as well as fatal encephalitis, which is lethal inflammation of the brain (4). Depending on the strain (5) and local capabilities for early detection and clinical management, the virus has a death rate of between 40% and 100% (Figure 1) (6). It has been detected in 32 of the country's 64 districts and has previously caused outbreaks in India, the Philippines, and Singapore (4). Evidence of the virus has also been found in Cambodia, Ghana, Indonesia, Madagascar, and Thailand (7). As of 2023, there have been a total of 721 confirmed cases of NiV worldwide, resulting in 419 deaths (8). Laboratory diagnosis of NiV infection requires a combination of tests that include RT-PCR from bodily fluids and ELISA for antibody detection.
The Nipah virus strains found in Bangladesh and Malaysia are constantly changing and evolving (9). Due to its quick transmissibility and high mortality rate, this virus could cause a global public health disaster (10). The Nipah virus strain prevalent in Bangladesh is highly pathogenic (11) and poses a real concern about the virus spreading across borders. It has already been detected in Kerala, India, where it caused two deaths among six laboratory-confirmed cases of infection (12). Person-to-person transmission of the Nipah virus is common in both Bangladesh (13) and India (14). Furthermore, it has been confirmed for the first time in Bangladesh that the virus (NiV-specific antibodies) can be transferred through the placenta from the mother to a newborn (15). Currently, there are no licensed treatments for the Nipah virus, but a live attenuated vector of recombinant vesicular stomatitis virus (rVSV) is being developed for the invention of the Nipah virus vaccine (16). Zoonotic viruses such as Ebola, HIV, MERS, Monkeypox, SARS-CoV-2, and Zika have become increasingly common in recent years. These RNA viruses mutate quickly, much like SARS-CoV-2, which has already caused the deaths of almost 5 million people, making them a significant threat to global health. Additionally, the Nipah virus can attach to the ephrin B-2 and B-3 receptors of epithelial cells. These receptors act as gateways to invade the tissues of the host, vital for transmission and infection; thus, zoonotic NiV has the potential to infect a broad range of mammals as ephrin B-2 and B-3 receptors are found in many mammals (17). Therapeutic development for the Nipah virus in low-income countries like Bangladesh is unattractive to businesses, and designing clinical trials poses challenges (18). Therefore, to prevent future zoonotic RNA virus outbreaks, it is essential to raise public awareness, exercise health vigilance, and implement control measures to reduce the impact of the emerging Nipah virus.