1. Background
Women's health practices during pregnancy refer to those activities and habits of pregnant women which impact their health (1). These practices include having a healthy diet, controlling maternal weight gain, adequate rest and sleep, regular exercise, regular prenatal care, oral hygiene and avoiding alcohol, tobacco and other illicit substances (2). The malaria and HIV prevention, foetal measurements including the use of ultrasound, nutritive and balanced diet, recreation, physical exercise, rest and sleep, dress and dwellings and body cleanliness, precautionary measures and home sanitation are other positive health practices in pregnancy (3). These practices are aimed at maintaining maternal and foetal health.
In a Nigeria Demographic and Health Survey 2018 only 58% of the pregnant women slept under an insecticide-treated net (ITN) the night before the survey. Also, 31% of women with a child born in the last 5 years did not take any iron tablets during their most recent pregnancy; the same percent took iron tablets for 90 days or more during their most recent pregnancy; and only 17% of women took deworming medication (4). There are reports in northern Nigeria of pregnant women patronising over the counter drugs for treating minor discomforts of pregnancy (5). In a study conducted in Katsina, Yobe and Zamfara States, only 27% of women with a live birth in the previous five years had attended at least one antenatal consultation. Thirty percent sought advice from friends, family or traditional birth attendants, and the rest did not seek or receive any pregnancy-related advice (4).
Patel et al. (6) asserted that adverse pregnancy outcomes (APOs) are said to occur when any of the following events exist: Losing a baby during early pregnancy (miscarriage or spontaneous abortion), losing a baby in late pregnancy (stillbirths), and delivery of a baby earlier than normal time (preterm birth) or having a baby with low birth weight. However, Yeshialem et al. (7) point out that APOs vary from pregnancy to pregnancy and it includes intrauterine foetal death, early neonatal death and late neonatal death. Several risk factors for APOs have been identified including maternal tobacco consumption (8), and exposure to unsafe water, poor sanitation, and poor waste management (9).
Globally about 3 million third trimester stillbirths are occurring annually with the same number of occurrences of infant death within 28 days of life (10). Around 14% of all births in sub-Saharan Africa result in stillbirths (11) and more than 60% of global preterm births occur in Asia and sub-Saharan Africa (12). In Nigeria, of the children with known birth weights, 7% weighed less than 2.5 kg at birth. But according to mothers’ reports, 3% of births were very small, 11% were smaller than average, and 85% were average or larger. Also, the country’s infant mortality rate was 67 deaths per 1,000 live births and the neonatal mortality rate was 39 deaths per 1,000 live births in 2018 (13).
In the recent years, association between the maternal life style and pregnancy outcomes has been given attention. But related studies are limited in sub-Saharan Africa (14). Most of the studies did not give emphasis on maternal characteristics that could affect the health practices in pregnancy. This could be useful in identifying the risk factors of APOs especially in countries like Nigeria where the APOs are not uncommon. The low health practices among pregnant women and the common occurrence of APOs in developing countries like Nigeria as well as inadequacy of studies that completely addressed the issue make the investigation of pregnant women’s health practices and self-reported APOs pertinent.
2. Objectives
The study was aimed at investigating pregnant women’s health practices and self-reported APOs.
3. Methods
3.1. Study Design and Population
The study was a retrospective cross-sectional analytic study that investigated pregnant women’s health practices and self-reported APOs in Ante-Natal Clinic (ANC) unit of Ahmad Sani Yariman Bakura Specialist Hospital, Gusau, Zamfara State, Nigeria. Only multigravida and grand-multigravida women were included. Pregnant women with a known chronic disease or condition predisposing woman to APOs were excluded from the study. The calculated sample size was 190 and systematic sampling was used in selecting the study sample. However, 175 questionnaires were retrieved.
3.2. Instrument for Data Collection
The “Health Practices Questionnaire-II” (HPQ-II) adapted from Lindgren (15) was used in data collection. It was a Likert scale measured as 1 = Never, 2 = Almost never, 3 = Sometimes, 4 = Almost always, and 5 = Always. The measuring scaled used was a mean score of ≤ 3.00 is low health practices; a mean score of 3.01 - 4.00 is moderate health practice; and a mean score of 4.01 - 5.00 is high health practices. Adverse pregnancy outcomes was assessed using a researcher constructed questionnaire. It was measured as ≤ 10 very low, 11 - 20 low, 21 - 30 moderate, 30 - 40 high, and 41 - 50 very high. The reliability of the adapted HPQ-II was 0.782 using Cronbach’s alpha.
3.3. Data Analysis
Data were analysed using Statistical Package for Social Science (SPSS) version 26. Frequencies and percentages were used to present the respondents’ socio-demographic variables and health practices. Spearman rank order correlation was used to examine the correlation between respondents' health practices and their self-reported APOs. Chi-square was used to assess the association between respondents’ demographic variables and pregnant women's health practices and APOs respectively at 0.05 level of significance.
4. Results
Table 1 indicates that the respondents within the age bracket 15 - 24 years were having the highest percentage (41.1%). The majority (57.7%) of the respondents had 1 - 3 deliveries. Also, the majority (62.3%) of the respondents were having 2 - 4 pregnancies. The respondents with tertiary education had the highest percentage (37.1%).
| Variables | No. (%) |
|---|---|
| Age bracket | |
| 15 - 24 | 72 (41.1) |
| 25 - 34 | 48 (27.4) |
| 35 - 44 | 31 (17.7) |
| ≥ 45 | 24 (13.7) |
| Number of deliveries | |
| 1 - 3 | 101 (57.7) |
| 4 - 6 | 37 (21.1) |
| 7 - 9 | 21 (12.0) |
| ≥ 10 | 16 (9.1) |
| Number of pregnancies | |
| 2 - 4 | 109 (62.3) |
| 5 - 7 | 26 (14.9) |
| 8 - 10 | 26 (14.9) |
| ≥ 11 | 14 (8.0) |
| Level of education | |
| Primary | 19 (10.9) |
| Secondary | 61 (34.9) |
| Tertiary | 65 (37.1) |
| Non-formal | 30 (17.1) |
| Socio-economic status | |
| Upper - upper | 27 (15.4) |
| Upper | 21 (12.0) |
| Middle | 99 (56.6) |
| Lower | 11 (6.3) |
| Lower - lower | 17 ( 9.7) |
Table 2 revealed that there were significant weak negative correlations between the health practices and all the APOs (P < 0.01) except in neonatal death.
| APOs | Correlation | P-Value |
|---|---|---|
| Hypertension in pregnancy | -0.387 | < 0.001 |
| Prenatal bleeding | -0.340 | < 0.001 |
| Intrauterine death | -0.236 | 0.002 |
| Still birth | -0.295 | < 0.001 |
| Preterm baby | -0.291 | < 0.001 |
| Caesarean section | -0.302 | < 0.001 |
| Low birth weight baby | -0.316 | < 0.001 |
| Malformed baby | -0.337 | < 0.001 |
| Neonatal death | -0.143 | 0.058 |
| Postpartum hemorrhage | -0.261 | < 0.001 |
Abbreviation: APOs, adverse pregnancy outcomes.
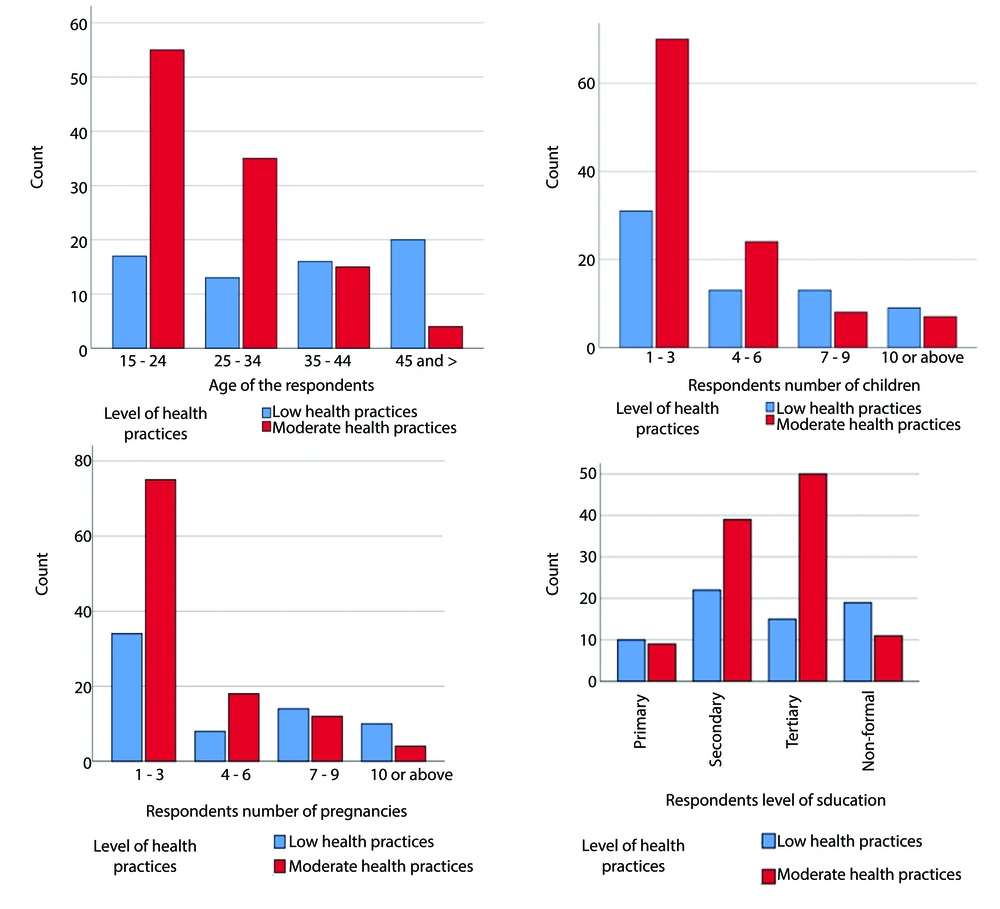
In Table 3 it is shown that there was a significant relationship between all the socio-demographic variables and respondents' health practices, P < 0.01 except for the number of deliveries, P < 0.05.
| Variables | Low Health Practices | Moderate Health Practices | Total | χ2 | P-Value | Cramer’s V |
|---|---|---|---|---|---|---|
| Age bracket | 32.217 | 0.00 | 0.43 | |||
| 15 - 24 | 17 (23.6) | 55 (76.4) | 72 (41.1) | |||
| 25 - 34 | 13 (27.1) | 35 (72.9) | 48 (27.4) | |||
| 35 - 44 | 16 (51.6) | 15 (48.4) | 31 (17.7) | |||
| ≥ 45 | 20 (83.3) | 4 (16.7) | 24 (13.7) | |||
| Number of deliveries | 9.796 | 0.02 | 0.24 | |||
| 1 - 3 | 31 (30.7) | 70 (69.3) | 101 (57.7) | |||
| 4 - 6 | 13 (35.1) | 24 (64.9) | 37 (21.1) | |||
| 7 - 9 | 13 (61.9) | 8 (38.1) | 21 (12.0) | |||
| ≥ 10 | 9 (56.3) | 7 (43.8) | 16 (9.1) | |||
| Number of pregnancies | 12.162 | 0.00 | 0.26 | |||
| 1 - 3 | 34 (31.2) | 75 (68.8) | 109 (62.3) | |||
| 4 - 6 | 8 (30.8) | 18 (69.2) | 26 (14.9) | |||
| 7 - 9 | 14 (53.8) | 12 (46.2) | 26 (14.9) | |||
| ≥ 10 | 10 (71.4) | 4 (28.6) | 14 (8.0) | |||
| Level of education | 16.181 | 0.00 | 0.30 | |||
| Primary | 10 (52.6) | 9 (47.4) | 19 (10.9) | |||
| Secondary | 22 (36.1) | 39 (63.9) | 61 (34.9) | |||
| Tertiary | 15 (23.1) | 50 (76.9) | 65 (37.1) | |||
| Non-formal | 19 (63.3) | 11 (36.7) | 30 (17.1) | |||
| Socio-economic status | 38.266 | 0.00 | 0.47 | |||
| Upper-upper | 9 (33.3) | 18 (66.7) | 27 (15.4) | |||
| Upper | 5 (23.8) | 16 (76.2) | 21 (12.0) | |||
| Middle | 27 (27.3) | 72 (72.7) | 99 (56.6) | |||
| Lower | 10 (90.9) | 1 (9.1) | 11 (6.3) | |||
| Lower-lower | 15 (88.2) | 2 (11.8) | 17 (9.7) |
a Values are expressed as No. (%).
The multiple bar charts depicts the relationship between demographic variable and levels of health practices of the respondents (Figure 1).
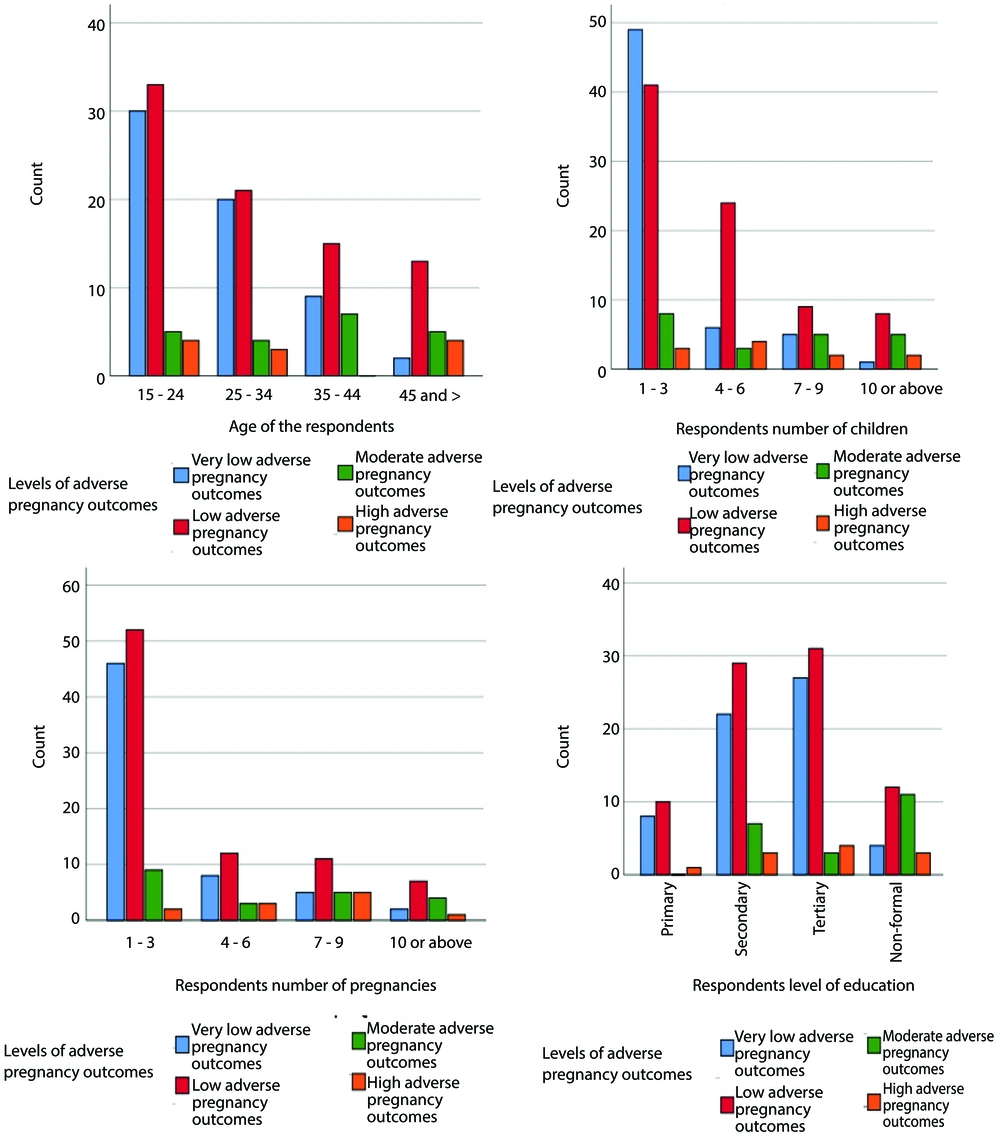
Table 4 revealed that there was no respondent with a very high APOs. There were strong significant relationships between socio-demographic variables and APOs, P < 0.01 across all the variables except in age variable in which P < 0.05.
| Variables | 1 | 2 | 3 | 4 | Total | χ2 | P-Value | Cramer’s V |
|---|---|---|---|---|---|---|---|---|
| Age range | 19.8 | 0.01 | 0.19 | |||||
| 15 - 24 | 30 (41.7) | 33 (45.8) | 5 (6.9) | 4 (5.6) | 72 (41.1) | |||
| 25 - 34 | 20 (41.7) | 21 (43.8) | 4 (8.3) | 3 (6.3) | 48 (27.4) | |||
| 35 - 44 | 9 (29.0) | 15 (48.4) | 7 (22.6) | 0 (0.0) | 31 (17.7) | |||
| ≥ 45 | 2 (8.3) | 13 (54.2) | 5 (20.8) | 4 (16.7) | 24 (13.7) | |||
| Number of deliveries | 30.9 | < 0.001 | 0.24 | |||||
| 1 - 3 | 49 (48.5) | 41 (40.6) | 8 (7.9) | 3 (3.0) | 101 (57.7) | |||
| 4 - 6 | 6 (16.2) | 24 (64.9) | 3 (8.1) | 4 (10.8) | 37 (21.1) | |||
| 7 - 9 | 5 (23.8) | 9 (42.9) | 5 (23.8) | 2 (9.5) | 21 (12.0) | |||
| ≥ 10 | 1 (6.3) | 8 (50) | 5 (31.3) | 2 (12.5) | 16 (9.1) | |||
| Number of pregnancies | 21.8 | < 0.001 | 0.20 | |||||
| 1 - 3 | 46 (42.2) | 52 ( (47.7) | 9 (8.3) | 2 (1.8) | 109 (62.3) | |||
| 4 - 6 | 8 (30.8) | 12 (46.2) | 3 (11.5) | 3 (11.5) | 26 (14.9) | |||
| 7 - 9 | 5 (19.2) | 11 (42.3) | 5 (19.2) | 5 (19.2) | 26 (14.9) | |||
| ≥ 10 | 2 (14.3) | 7 (50) | 4 (28.6) | 1 (7.1) | 14 (8) | |||
| Level of education | 23.2 | < 0.001 | 0.22 | |||||
| Primary | 8 (42.1) | 10 (52.6) | 0 (0.0) | 1 (5.3) | 19 (10.9) | |||
| Secondary | 22 (36.1) | 29 (47.5) | 7 (11.5) | 3 (4.9) | 61 (34.9) | |||
| Tertiary | 27 (41.5) | 31 (47.7) | 3 (4.6) | 4 (6.2) | 65 (37.1) | |||
| Non-formal | 4 (13.3) | 12 (40) | 11 (36.7) | 3 (10) | 30 (17.1) | |||
| Socio-economic status | 25.4 | < 0.001 | 0.24 | |||||
| Upper-upper | 12 (44.4) | 14 (51.9) | 1 (3.7) | 0 (0.0) | 27 (15.4) | |||
| Upper | 8 (38.1) | 10 (47.6) | 3 (14.3) | 0 (0.0) | 21 (12) | |||
| Middle | 38 (38.4) | 47 (47.5) | 9 (9.1) | 5 (5.1) | 99 (56.7) | |||
| Lower | 1 (9.1) | 4 (36.4) | 4 (36.4) | 2 (18.2) | 11 (6.3) | |||
| Lower-lower | 2 (11.8) | 7 (41.2) | 4 (23.5) | 4 (23.5) | 17 (9.1) |
Abbreviation: APOs, adverse pregnancy outcomes.
a Values are expressed as No. (%).
b 1, very low APOs; 2, low APOs; 3, moderate APOs; 4, high APOs.
The multiple bar charts depicts the relationship between demographic variable and levels of APOs of the respondents (Figure 2).
5. Discussion
Usually pregnancy inspires women to develop a healthier practices even before becoming pregnant. This makes practicing healthy behaviour more successful during pregnancy, and positively influences the infant’s life (16). Despite this and the importance of healthy practices in the health of an individual, and most importantly in the health of pregnant women, developing foetus and infant; it was found that no respondents had a high level of health practices. This situation is capable of causing negative pregnancy outcomes, since one of the major attribute of a successful pregnancy is healthy prenatal behaviors (17).
However, about two-thirds of the respondents were having moderate health practices. Contrary to this study, a cross-sectional study on predictors of health practices among a group of Iranian adolescent pregnant women found that the mean score of health practice was very good (18). Their study was only on adolescent pregnant women. This, and differences in the study areas might be the reasons for the differences. Another found that pregnant women had high levels of healthy behaviours including healthy practices (19). The authors used different instruments with this study and there are differences in culture and traditions between the two areas of the studies.
By implication, the women’s insight should be developed toward understanding that the pre-pregnancy negative behaviour can have devastating effect on both the mother, foetus and infant. Many maternal risk factors develop either prior to pregnancy or between pregnancies (20). Addressing these risk factors serves as a pathway for ensuring safer motherhood (21). This study’s results revealed the higher the APOs the lower the health practices. This finding is in consonance with the assertion that health practices of women during pregnancy can affect maternal and foetal health, and influence pregnancy outcomes (2). A chance of having healthy children improves with healthy behaviours (22). Lower health practices among pregnant women are therefore risk factors that can be manipulated through appropriate intervention (23).
The percentage of low health practices increased with an increase in age. The percentage of moderate health practices decreased with an increase in age. The younger women had more healthy practices than the older women with a significant association. In disagreement with this study, Boguszewski et al. (19) found no correlation between age and levels of healthy behaviour amongst pregnant women. However, in consonance to this study, the authors found that women under 30 years old manifested substantially higher levels of healthy behaviour. The two studies have differences in the respondent’s’ age grouping.
The percentage of low health practices roughly increased with an increase in number of deliveries. Also, the percentage of moderate health practices roughly decreased with an increase in number of deliveries. This finding tally with the finding of a study at Abou-Tig district Assiut in where it was found that there is a significant relationship between the number of births and Health-promoting lifestyle behaviours (P < 0.05) (24). The percentage of low health practices roughly increased with an increase in number of pregnancies. Likewise, the percentage of moderate health practices roughly decreased with an increase in number of pregnancies. This is in accordance with the association between the number of deliveries and health practices.
The results of this study indicate that the higher the level of education the higher the health practices. This finding is in agreement with the findings of a study conducted in the Netherlands, where it was found that lower educated women were more likely to have low health control beliefs (25). In line with these findings, educated women are more likely to understand the public health message (26). It was also found in this study that the higher the socio-economic status the higher the health practices. In agreement with this finding other studies have also shown a relationship between socio-economic status and rates of smoking, alcohol use, and dietary behavior (27). However, the strength of the relationship in this study was moderate.
In this study, the higher the age brackets, the higher the APOs. This is in accordance with the findings of this study in which the lower age brackets had higher health practices. Also, finding of a study by Boguszewski et al. (19) revealed that women under 30 years old manifested substantially higher levels of healthy behaviour. In accordance with a study in Kenya (28), respondents at the upper extreme parity were having the highest percent in high APOs. The authors found that parity is associated with APOs. High parity is associated with adverse outcomes. In another dimension, the lower the number of pregnancies the lower the APOs.
In this study APOs were found to be higher among those with non-formal education. The educated women are more likely to understand health messages (26); and therefore more likely to adhere to the messages, and in turn impact their health positively. It is shown that the higher the socio-economic status, the lower the APOs. Also, the lower the socio-economic status, the higher the APOs. This finding corresponds with the finding of this study that respondents with lower socioeconomic status had a higher percent of low health practices, and the respondents with upper socio-economic status had a higher percent of moderate health practices.
5.1. Limitations
The limitations of this study include the use of retrospective information from the respondents, which could be associated with recall bias. The use of one center for the study is associated with limited sample size. Moreover, other factors such as maternal stress, emotional support, cultural beliefs, and social support were not considered in this study.
5.2. Conclusions
The health practices of the pregnant women were mostly moderate. There were weak negative significant correlations between pregnant women's health practices and APOs. Also, very few respondents had a high-level APOs. Further studies can focus on the mediators of maternal health practices and APOs. The maternal stress, emotional support, cultural beliefs, and social support can be considered as possible mediators. Based on the findings of the study, the following recommendations are made: (1) Healthcare professionals should give high emphasis on older women and grand multiparous when educating mothers about health practices for healthy pregnancy and birth. (2) Healthcare professionals should provide an economical strategy for ensuring health practices to mothers from a low socio-economic background.