1. Background
Infertility is a personal and social problem that can expose affected individuals to various psychological pressures (1). Infertility is a process that affects the physical, occupational, personality, and mental state, and has adverse effects on the individual's emotions, including self-esteem (2). Researchers have reported the occurrence of impulsive behaviors and diffuse pressures, depression, feelings of helplessness and worthlessness, anxiety, and restlessness in infertile individuals (3).
In order to reduce the psychological consequences of infertility, health counselors and psychologists should understand the factors affecting infertility and the depression caused by it so that they can help these people in psychological crises (4). Finding predisposing factors for depression in infertile people and screening those at risk and supporting and protecting them from this can be very valuable in improving the outcome of infertility treatment (5).
Since infertility is a multifactorial problem, understanding these factors requires extensive studies (6). One of the important factors of infertility that has received less attention is lifestyle, which is the normal and routine daily activities that people accept as acceptable in their lives (7). By choosing a specific lifestyle, an individual takes measures and activities to maintain and improve their health and prevent diseases, including following a proper diet, sleeping, resting, exercising, controlling body weight, not smoking and drinking alcohol, and immunizing against diseases (8). Lifestyle has a decisive effect on the aforementioned factors, and every person can enjoy physical and mental well-being by having a desirable daily life pattern (9). Following a health-oriented lifestyle can easily prevent this problem among couples, away from the exorbitant costs of infertility treatments (10).
Another factor related to mental health is social health, which includes the levels of social skills, social functioning, and the ability of each person to recognize themselves as a member of society. In measuring social health, attention is paid to the way a person communicates in the network of social relationships (11). Since life and social health are interconnected and cannot be considered separately from each other, it is important to pay attention to social health as one of the important dimensions of health (1). Considering the above points, on the one hand, several factors such as lifestyle, social health, and marital satisfaction have a significant impact on the physical and mental health of individuals (12); on the other hand, infertile women are exposed to more severe physical, psychological, and social harms and are mainly affected by these factors (4-6, 11). Therefore, it seems necessary to investigate and determine the role of mental health and lifestyle in the occurrence of depression in infertile women (2, 11).
2. Objectives
The main aim of the present study was to determine a predictive model of depression in infertile women based on lifestyle and social health components mediated by marital satisfaction.
3. Methods
3.1. Sampling
The statistical population was all infertile women with depression who referred to infertility centers in Kermanshah in 2021. The sampling of this study was conducted using census method, in which 360 infertile women were selected based on the depression score obtained from the Beck Questionnaire (score 8 and above).
3.2. Inclusion and Exclusion Criteria
Incomplete responses to any of the questionnaires were considered exclusion criteria, while inclusion criteria included the following items:
- Consent to participate in the present study.
- Infertility (at least six months have passed since the diagnosis of infertility).
- A score of at least eight on the Beck Depression Inventory (Beck's score indicated moderate depression).
- No history of depression according to the client's report.
- No use of medications related to the treatment of depression according to the client's report.
- No underlying diseases according to the client's file (underlying and chronic diseases can cause depression, while in this study the aim was to find samples whose depression is due to infertility).
- No use of tobacco and narcotics according to the client's file.
- Having a mobile phone and familiarity with how it works (in order to complete online questionnaires).
- Being literate.
3.3. Data Collection Tools
3.3.1. Beck Depression Inventory-Short Form
The Beck depression inventory-short form (BDI-SF) has 13 questions that assess both the presence and severity of depressive symptoms, and the questions are scored on a Four-Point Likert Scale from “0” to “3”. The interpretation of the BDI-SF is that to obtain the overall score, the total score of all questions is added together, and the minimum and maximum total scores fluctuate from zero to 39. The results of the study by Stefan-Dabson et al. showed that the findings of factor analysis and validity testing indicate its suitability for evaluating the results of any type of clinical trial. In addition, the findings of the aforementioned study showed that the BDI-SF has adequate reliability for diagnosing and measuring the severity of depression (13).
3.3.2. Health-Promoting Lifestyle Profile
The health-promoting lifestyle profile II (HPLP-II) is a modified version of the HPLP developed by Walker et al. and measures health-promoting lifestyles by focusing on individual initiative and self-perception (14). The questionnaire consists of 52 questions and six subscales, including nutrition, physical activity, health responsibility, stress management, interpersonal relationships, and spiritual growth. The HPLP-II asks respondents to indicate, using a Four-Point Likert-Type Response Scale (including “never,” “sometimes,” “often,” and “usually”), how often they engage in specific health-promoting behaviors. Overall, the health-promoting lifestyle score and behavioral dimension score are calculated using the average of responses for all 52 questions and for each subscale (8 to 9 items). Walker and Hill-Polerecky reported a Cronbach's alpha of 0.94 for the HPLP-II, with a range of 0.79 to 0.94 for its six subscales (15). In addition, Mohammadi Zeidi et al. evaluated the reliability of the Persian version of the HPLP-II, which had an overall Cronbach's alpha of 0.82, while this coefficient varied between 0.64 and 0.91 for the subscales. Also, its content validity was assessed and confirmed through exploratory factor analysis (16).
3.3.3. Keyes's Social Well-Being Questionnaire
Keyes's Social Well-Being Questionnaire (KSWBQ) has five components including social flourishing, social solidarity, social cohesion, social acceptance and social participation. This questionnaire has 20 questions and the answer to each question is in the form of a Five-Point Likert Scale from “strongly agree” to “strongly disagree”. Higher scores will indicate higher social health and vice versa. The validity and reliability of KSWBQ have been confirmed in various studies conducted in Iran and for example in the study of Hashemi et al., Cronbach’s alpha coefficient was reported to be 0.81 (17).
3.3.4. ENRICH Marital Satisfaction Scale
ENRICH Marital Satisfaction Scale (EMSS) has 47 questions and Five-Point Likert Scale. To obtain the total score of EMSS, the total scores of all questions are added together. Higher scores indicate better marital satisfaction. The validity and reliability of this questionnaire were examined by EMSS Arab Alidousti et al. The results of the reliability assessment of the questionnaire were using two methods: Cronbach's alpha and item-scale correlation, with Cronbach's alpha being at least 0.7 and item-scale correlation being at least 0.2 for all items. In addition, the validity of the questionnaire was confirmed using three different methods (18).
3.4. Data Anlysis
The obtained raw data were analyzed using SPSS-Ver.22 and partial least squares (PLS)-Version 3 software, and a predictive model was designed based on the relationship and correlation between the variables.
4. Results
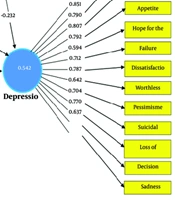
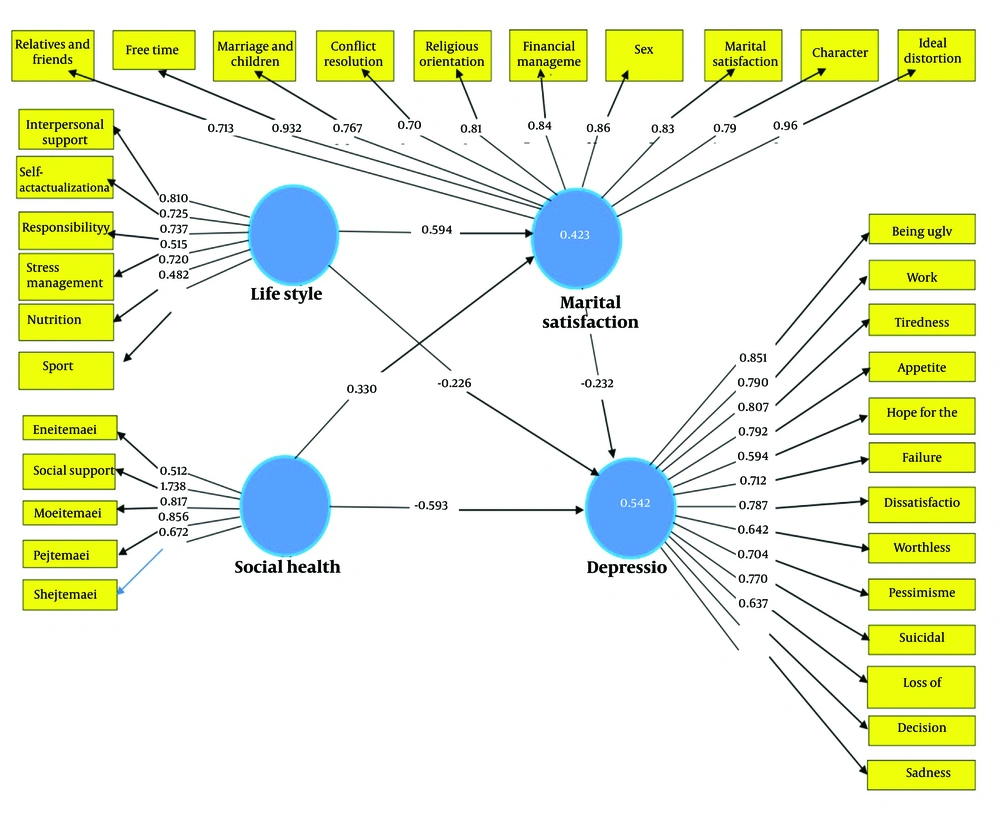
The present study included 360 infertile women, whose demographic characteristics can be seen in Table 1. The findings showed that in terms of social health, the highest and lowest scores were related to the components of social acceptance and social solidarity, respectively (Table 2). In addition, in terms of health-promoting lifestyle, the highest score was related to the component of exercise and the lowest score was related to the components of stress management and self-actualization (Table 3). Based on the results, the scores of the components related to marital satisfaction were almost similar (Table 4). Also, the mean±standard deviation related to depression of the participants of the present study was equal to 7.79 ± 1.32 (Table 5). The findings obtained from the Kolmogorov-Smirnov test showed that all the main variables discussed in the present study have a normal distribution (P > 0.05) (Table 6). The findings of the present study showed that the three main variables including social health, lifestyle and marital satisfaction had an indirect (negative) and significant correlation with the depression variable. While there was a direct (positive) and significant relationship between the three main variables mentioned above with each other in a pairwise manner (Table 7). Also, based on the findings of this study, the lifestyle and social health variables had an indirect effect on depression through the mediation of marital satisfaction (Figure 1).
| Variables | Frequency (%) |
|---|---|
| Age (y) | |
| ≤ 25 | 13 (3.6) |
| 25 - 30 | 79 (21.9) |
| 30 - 35 | 93 (25.8) |
| 35 - 40 | 153 (42.5) |
| 40 ≤ | 22 (6.1) |
| Work status | |
| Housekeeper | 357 (99.2) |
| Employee | 3 (0.8) |
| Education level | |
| Under diploma | 253 (70.3) |
| Diploma and above | 107 (29.7) |
| Number of pregnancies | |
| Zero | 236 (65.6) |
| Once | 122 (33.9) |
| Twice | 1 (0.3) |
| Five times | 1 (0.3) |
| Number of deliveries | |
| Zero | 240 (66.7) |
| Once | 120 (33.3) |
| Number of abortions | |
| Zero | 355 (98.6) |
| Once | 4 (1.1) |
| Three times | 1 (0.3) |
| Other variables (No) | |
| Underlying disease | 360 (100.0) |
| History of depression | 360 (100.0) |
| Taking medication | 360 (100.0) |
| Type of medicine | 360 (100.0) |
| Total | 360 (100.0) |
The Demographic Characteristics of Study’ Participants
| Social Health Components | Samples (No.) | Mean ± SD | Skewness | Kurtosis |
|---|---|---|---|---|
| Social health | 360 | 61.54 ± 8.94 | 0.56 | 0.89 |
| Social solidarity | 360 | 8.73 ± 2.69 | 1.45 | 0.99 |
| Social cohesion | 360 | 9.60 ± 3.27 | 0.65 | 0.78 |
| Social participation | 360 | 15.89 ± 4.02 | 1.23 | 1.71 |
| Social acceptance | 360 | 16.08 ± 3.75 | 0.62 | 0.69 |
| Social prosperity | 360 | 11.23 ± 2.49 | 0.45 | 0.12 |
The Descriptive Statistics Related to the Social Health Variable of the Study’ Participants
| Health-Promoting Lifestyle Components | Samples (No.) | Mean ± SD | Skewness | Kurtosis |
|---|---|---|---|---|
| Lifestyle | 360 | 130.82 ± 24.98 | 0.45 | 0.78 |
| Nutrition | 360 | 26.55 ± 6.78 | -0.58 | -0.36 |
| Exercise | 360 | 34.02 ± 6.59 | 1.12 | 0.89 |
| Responsibility | 360 | 21.21 ± 4.82 | 0.95 | 0.10 |
| Stress management | 360 | 14.87 ± 3.78 | 0.69 | 0.75 |
| Interpersonal support | 360 | 17.57 ± 6.01 | 0.36 | 0.52 |
| Self-actualization | 360 | 16.58 ± 3.64 | 1.20 | 1.55 |
The Descriptive Statistics Related to the Health-Promoting Lifestyle Variable of the Study’ Participants
| Marital Satisfaction Components | Samples (No.) | Mean ± SD | Skewness | Kurtosis |
|---|---|---|---|---|
| Marital satisfaction | 360 | 130.29 ± 26.25 | 0.78 | 1.12 |
| Ideal distortion | 360 | 7.03 ± 2.56 | 0.35 | 1.20 |
| Character | 360 | 12.63 ± 3.92 | 0.58 | 0.68 |
| Marital relationship | 360 | 11.98 ± 4.50 | 0.87 | 0.91 |
| Conflict resolution | 360 | 13.54 ± 3.40 | 1.10 | 1.45 |
| Financial management | 360 | 13.51 ± 3.85 | 0.52 | 0.85 |
| Leisure time | 360 | 16.00 ± 2.99 | 0.36 | 1.23 |
| Sexual relationship | 360 | 15.15 ± 4.81 | -0.45 | 0.78 |
| Marriage and children | 360 | 13.56 ± 3.87 | 0.12 | 0.32 |
| Relatives and friends | 360 | 12.95 ± 3.66 | 1.54 | 0.98 |
| Religious orientation | 360 | 13.89 ± 4.12 | 0.45 | 0.78 |
The Descriptive Statistics Related to the Marital Satisfaction Variable of the Study’ Participants
| Variable | Samples (No.) | Mean ± SD | Skewness | Kurtosis |
|---|---|---|---|---|
| Depression | 360 | 7.79 ± 1.32 | 0.36 | 0.79 |
The Descriptive Statistics Related to the Depression Variable of the Study’ Participants
| Variables | Test Quantity (K-S) | P-Value | Status |
|---|---|---|---|
| Social health | 0.72 | 0.12 | Normal |
| Lifestyle | 0.80 | 0.30 | Normal |
| Marital satisfaction | 0.87 | 0.22 | Normal |
| Depression | 0.77 | 0.41 | Normal |
The Kolmogorov-Smirnov Test for Normality of Data
| Variables | Depression | Marital Satisfaction | Lifestyle | Social Health |
|---|---|---|---|---|
| Social health | -0.55 | 0.48 | 0.52 | 1 |
| Lifestyle | -0.41 | 0.59 | 1 | - |
| Marital satisfaction | -0.61 | 1 | - | - |
| Depression | 1 | - | - | - |
The Pearson Correlation Coefficient Between Research Variables
5. Discussion
The findings showed that there is a direct and negative correlation between the two lifestyle variables and depression, and among the different lifestyle items, social support and exercise components are more strongly correlated with depression. From a psychological perspective, people's lifestyle plays an important role in their mental and social health. In this regard, in a similar study conducted by Njogu et al., it was reported that stress, anxiety, and depression are side effects of treatment for infertile women (19). Also, Alnaeem et al. evaluated anxiety and depression in infertile women with polycystic ovary syndrome and its correlation with lifestyle; the findings of the aforementioned study showed that two-thirds of the women studied had depression, anxiety, and stress, which was correlated with their age, weight, diet, and lifestyle (20).
Based on the findings of the present study, there is a direct and negative relationship between the social health variable and depression. Although all social health components have an impact on depression, this correlation was slightly stronger for the cohesion and participation components and weaker for the flourishing component. Bedaso et al. reported that pregnancy is a time of profound physical and emotional changes, as well as an increased risk of mental illness. They believe that strengthening social support as one of the components of social health is a common factor for reducing mental health risks. Therefore, policymakers and those working in the field of maternity care should consider developing targeted social support programs with the aim of helping to reduce mental health problems among pregnant women (21). In a study conducted on infertile women, Zarif Golbar Yazdi et al. concluded that both women and men are affected emotionally, physically, and socially by infertility, but women are in a more difficult position compared to men (22). The findings of the study by Tafvizi Zavareh et al. showed that there is an inverse and significant relationship between mental health statuses and perceived social support score, which is consistent with the findings of the present study (23).
According to the findings of this study, there was significant and negative correlation between depression and components of marital satisfaction in infertile women. Infertility can cause disruption in the quality of marital relationships, fear of separation, decreased self-confidence, and feelings of rejection from family and society. The combination of these factors can make an individual susceptible to mental and psychological diseases such as depression and anxiety, and lack of enjoyment of marriage. Fazaeli et al. emphasized in their study that marital dissatisfaction is associated with the occurrence of psychological problems including depression and stress (24). The mental and social health of individuals is influenced by a range of psychological, sociological, and demographic factors. In Iran, despite the existing deficiencies, especially in deprived areas, appropriate steps have been taken for the physical health of individuals. Sometimes, in Iran, the mental and social dimensions of health are neglected, and this neglect of the social aspect of health increases the vulnerability of individuals (11, 22). In various studies, the correlation between depression and infertility with marital satisfaction has been evaluated as intertwined factors. Mansouri et al. believe that infertility, as one of the stressors, can create important problems in couples' relationships, including reduced communication with each other, difficulties in sexual activity, and emotional and mental disorders (25).
Also, based on the findings of this study, the lifestyle variable had an indirect effect on depression through the mediation of marital satisfaction. To explain this finding, it can be said that common factors in marital satisfaction and lifestyle lead to life satisfaction and improve mental health. Marital satisfaction is actually positive and enjoyable attitude that makes couples satisfied with various aspects of life, including opportunities, decision-making, income, lifestyle, sexual relationship, etc. In addition, marital satisfaction creates feeling of happiness that has significant impact on the mental health of couples.
The findings of the present study showed that the social health variable had an indirect effect on depression through the mediation of marital satisfaction. Perhaps the social dimension of health is the most complex and at the same time the most controversial aspect of health. Also, the social health of individuals is one of the factors affecting the level of marital satisfaction, which is supported by which family relationships can be understood and predicted. People with appropriate social health and high marital satisfaction do not feel isolated and feel calm and trusting with their family.
Based on the results of the present study, the main hypothesis of this study was confirmed and it can be stated that depression in infertile women can be predicted based on lifestyle and social health components with the mediation of marital satisfaction. Theories of scientists and psychologists as well as similar studies also strengthen the validity of this hypothesis.
5.1. Limitations
Limitations of the study include the following:
- Since the questionnaires were online, the researchers could not track and control whether the participants understood the questions and responded appropriately.
- Due to the COVID-19 pandemic and the decrease in the number of visits to the infertility clinic, sampling was conducted over longer period of time.
- Environmental stressors such as the COVID-19 emergency were not controllable by the researcher.
- Stressors resulting from difficult infertility treatments, disappointment, and family problems were not controllable by the researcher.
5.2. Conclusions
Based on the findings of the present study, it can be said that the three main variables including social health, lifestyle and marital satisfaction have indirect (negative) and significant relationship with the depression variable. While, there was direct (positive) and significant correlation between the three main variables mentioned above with each other in two-by-two manner. Also, based on the findings of this study, the lifestyle and social health variables had an indirect effect on depression through the mediation of marital satisfaction. Based on the results of the present study, the main hypothesis of this study was confirmed and it can be stated that depression in infertile women can be predicted based on the components of lifestyle and social health through the mediation of marital satisfaction.