1. Context
From the distant past, pain has been a part of human experiences that can be protective, stimulating, or destructive and can also make people aware of the existence of an apparent or hidden injury in the human body (1). Pain is a complex combination of physiological, psychological, social, and cultural variables, and each person's sensitivity to it differs (2).
Pain after surgery is still one of the clinical challenges for nurses and the patient's family (3). Improper management of pain after surgery may cause anxiety, insomnia, increased stress, and limited mobility (3, 4). In addition, inadequate pain treatment increases postoperative complications and requires more extended hospitalization (5). The lack of control of acute pain after surgery is associated with many other complications, including increased disease severity, physical dysfunction, reduced quality of life, reduced recovery process, long-term use of narcotic drugs during and after hospitalization, and increased costs (6, 7). Narcotic drugs have many side effects in controlling pain after surgery. For example, morphine has negative effects on the internal regulation of the release of endorphins in the body's natural response to pain (3, 8). In addition, post-operative pain (POP) relief without the use of narcotic drugs reduces nausea and vomiting, reduces the incidence of surgical site dislocation, and facilitates and increases mobility (8, 9).
In addition, early postoperative pain appears to cause persistent pain that may persist for several months after surgery in a significant proportion of patients. Analgesic measures are necessary to prevent the development of acute and chronic pain after surgery and to reduce the occurrence and intensity of pain during and immediately after surgery (3, 5, 6). Pain management is one of the most significant clinical challenges of nursing during the postoperative care period (6). Although the studies show improvements in the current situation, some researchers still indicate insufficient pain management after surgery (10).
Efforts to increase patients' awareness of pain and analgesic options may increase the likelihood of achieving optimal pain control after surgery (11, 12). Patients should be comfortable enough to participate in recovery and continue self-care immediately in the postoperative period with the shortening of hospital stays and the increase of same-day surgery (13). Pre-operative education (POE) is a means to prepare patients for their role in pain planning and the postoperative recovery period (14). Pre-operative education can include information about the importance of pain control, treatment goals, the amount of pain experienced by the patient, and the importance of pain reporting (15, 16).
Pain management options include pharmacological and non-pharmacological methods that should be taught (17). This study evaluated the impact of POE on POP by reviewing previous studies, which were presented as a narrative review.
2. Evidence Acquisition
The current study was a narrative review type, and through the evaluation of the previous study, the research results were collected and became the basis of the present study. For this purpose, relevant studies from 1990 - 2024 were extracted through advanced search in national and international databases, including Web of Science, Islamic World Science Citation Center (ISC), Scopus, PubMed, Magiran, and Google Scholar Iran-Doc. Different keywords were used to search the databases mentioned above, the most important and relevant of which are "operation," "pre-operative," "education," "postoperative," "pain," "perioperative," and "recovery.""surgery," "elective surgery," "pain experience," "preoperative information," "undergoing surgery," "self-efficacy," "self-care," patient," "pain relievers," and "pain relief." Various criteria were used to exclude some searched studies from gathering results for the present review. Unpublished studies and studies published in non-authoritative journals and public Internet databases were not considered. Considering the primary purpose of the present study, only research was selected that focused on POP and pain caused by the disease itself, and before surgery, was not considered. In the first stage of the search, 184 studies were selected, and after applying the inclusion and exclusion criteria, 22 studies were considered for the present review.
3. Results
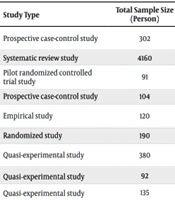
Past research has shown that post-surgery pain is still a severe problem for surgical patients. The available evidence on POE over POP shows various results. Based on the findings, approximately 64% of previous studies reported that POE has a positive and significant effect on POP, and the remaining 36% showed opposite results (Table 1).
| Authors; (Year) | Study Type | Total Sample Size (Person) | Surgery Type | Positive and Significant Effect of POE on POP? |
|---|---|---|---|---|
| Chaudhary and Shankar (2016) (11) | Prospective case-control study | 302 | Lab cholecystectomy, hernia surgery and anorectal surgery | Yes |
| Heydari et al. (2019) (14) | Systematic review study | 4160 | Various surgery | 7 studies (Yes) 6 studies (No) |
| Cooke et al. (2016) (17) | Pilot randomized controlled trial study | 91 | Joint replacement surgery | Yes |
| Pereira et al. (2016) (18) | Prospective case-control study | 104 | General ambulatory surgery | Yes |
| Aberomand et al. (2016) (19) | Empirical study | 120 | General, orthopedic and urology surgeries | Yes |
| Angioli et al. (2014) (20) | Randomized study | 190 | Gynecologic oncology surgery | Yes |
| Porras-González et al. (2015) (21) | Quasi-experimental study | 380 | Ambulatory surgery | Yes |
| Chen et al. (2014) (22) | Quasi‐experimental study | 92 | TKA | Yes |
| Sugai et al. (2013) (23) | Quasi‐experimental study | 135 | Outpatient surgery | Yes |
| Schmidt et al. (2015) (24) | Randomized controlled trial study | 652 | Oncologic surgery | Yes |
| Berge et al. (2004) (25) | Randomized controlled trial study | 40 | THR | Yes |
| Abd-Elghany et al. (2019) (26) | Quasi‐experimental study | 60 | TKA | Yes |
| Kearney et al. (2011) (27) | Quasi‐experimental study | 150 | Joint replacement surgery | Yes |
| Bakhshandeh et al. (2014) (28) | Quasi‐experimental study | 72 | Coronary artery bypass graft | Yes |
| Mohammadi et al. (2017) (29) | Quasi‐experimental study | 130 | Percutaneous nephrolithotomy (PCNL) | Yes |
| Amirmohseni et al. (2016) (30) | Quasi‐experimental study | 64 | Knee arthroplasty surgery | Yes |
| Louw et al. (2014) (31) | Randomized controlled trial study | 67 | Lumbar radiculopathy | No |
| Biau et al. (2015) (32) | Randomized controlled trial study | 209 | THR | No |
| van Dijk et al. (2015) (33) | Quasi-randomized controlled trial | 377 | Various surgery | No |
| Kesanen et al. (2017) (34) | Randomized clinical trial | 100 | Spinal stenosis surgery | No |
| Rapp et al. (2021) (35) | Retrospective matched case control study | 229 | Spinal surgery | No |
| Moharrami et al. (2021) (36) | Systematic review and meta-analysis | Not reported | Lower limb joint replacement surgery | 1 study (Yes) 4 studies (No) |
Abbreviations: THA, total hip arthroplasty; TKA, total knee arthroplasty.
A review by Heydari et al. was conducted on the effect of POE on POP. The results showed that out of thirteen evaluated studies, seven reported positive effects, and six reported no significant impact of POE on POP (14). In another study by Chaudhary and Shankar, the effect of POE on post-operative outcomes was investigated, and educational intervention by the researcher in the pre-operative period through personal counseling was provided to the study group. The findings showed that patients who receive structured, individual, and detailed POE and counseling can better deal with POP in the immediate postoperative period (11).
Cooke et al. showed that preoperative self-efficacy training for routine care for patients undergoing joint replacement surgery to reduce postoperative pain and anxiety also had no significant effect on patient satisfaction (17). Pereira et al. found that the empathetic patient-centered approach positively affects psychological and clinical outcomes in outpatient surgery candidates and significantly reduces POP (18)—the effect of patient education programs on headaches caused by spinal anesthesia. Aberomand et al. evaluated that educational programs significantly reduce headaches (19). In addition, another study on the effectiveness of providing oral or written preoperative information to female patient candidates for oncology surgery by Angioli et al. was conducted, and the findings showed a positive and significant impact of the information provided in reducing POP (20).
In addition, Porras-González et al., which was about the effectiveness of the nursing method in pain management after major outpatient surgery, showed that pre-surgery counseling by nurses caused a significant reduction in POP (21). The effect of POE intervention with face-to-face cognitive-behavioral training on pain and rehabilitation performance of patients who underwent total knee replacement (TKA) by Chen et al. was studied, and the findings showed a significant decrease in POP (22). In Sugai et al., the effectiveness of oral (interactive) and written training by the surgeon was evaluated for elective outpatient surgery patients, and the results of this research also showed that the above-mentioned interventional training method has a significant effect on reducing POP (23). In addition, Schmidt et al. reported that providing an educational booklet one day before surgery for candidates for various surgeries reduces the meaning of POP in patients (24). A randomized controlled trial by Berge et al. selected 40 patients who were candidates for total hip replacement (THR) and were divided into two intervention and control groups. Then, a short psychological pain management rehabilitation program was conducted for the intervention group, and no educational intervention was implemented for the control group. The results showed that patients who learned pain management experienced less pain intensity, discomfort, and sleep disturbance than the control group (25).
Abd-Elghany et al. conducted a study on the efficacy of implementing a pre-operative health education program on postoperative outcomes of patients undergoing total knee arthroplasty. The mentioned study showed significant improvement in the level of general awareness, self-reported actions, and the overall outcome score of knee injury and osteoarthritis in the intervention group compared to the control group after the training (26). In Kearney et al., the effects of POE on patient outcomes after joint replacement surgery were evaluated in 150 operated patients. The findings of the mentioned study showed that patients who participated in the POE class reported that they were more ready for surgery and were better able to control their POP (27). Based on the findings of Bakhshandeh et al. on patients undergoing coronary artery bypass graft surgery (28) and Mohammadi et al. regarding patients undergoing percutaneous nephrolithotomy (29), POE significantly reduces POP in surgical patients. In another study by Amirmohseni et al., a combined training program including face-to-face training, presentation of booklets, and presentation of an educational video one day before surgery was implemented for 32 people (intervention group) of knee arthroplasty surgery candidate patients but the control group (32 people) received routine care. The results showed that the intervention group reported significantly less dry POP than the control group most of the time (30).
Contrary to the research mentioned above, the findings of some other studies have shown that POE does not significantly affect POP. Lowe et al. also presented educational content verbally and face-to-face by a physiotherapist before surgery for patients with lumbar radiculopathy, the results of which showed that this educational method had no significant effect on POP (31). In Biau et al., the nurse taught the pain reliever pump and the care method related to the surgery by the physiotherapist twelve weeks before the surgery for patients who are candidates for THR. The findings showed that the aforementioned educational methods did not significantly affect POP for the studied patients (32). van Dijk et al. (2015) reported that providing an educational video about pain assessment, painkillers, and pain management for 1 - 30 minutes before surgery for surgical candidates did not significantly reduce POP (33). Similarly, in Kesanen et al., POE was provided through a telephone conversation for 21 minutes to patients with vertebral canal stenosis who were candidates for surgery; the non-significant effect on the reduction of POE was reported as the main finding of this study (34). In a retrospective matched case-control study conducted by Rapp et al., 229 candidates for spinal surgery were considered and divided into intervention (113 people) and control (116 people) groups. The intervention group patients participated in educational programs before the operation, but this did not happen to the control group. The results showed that POE for spine surgery candidates does not necessarily lead to improved pain management, shorter length of stay, or greater patient satisfaction (35). Moharrami et al., in a systematic review and meta-analysis study about POE for pain relief after lower limb joint replacement surgery, showed that training before total hip arthroplasty (THA) and total knee arthroplasty (TKA) cannot significantly reduce POP (36).
Most past studies have indicated that POE, as a complex intervention, can reduce POP. The reason for this complexity can be somehow related to the philosophy and nature of education. From the results of this evidence, many factors can be influential in the effectiveness of POE on POP, which include the type of surgery, length of follow-up period, continuity of care, method of providing education, quality of intervention, patient awareness of pain measurement method, Interactive training is accompanied by empathy, and anxiety reduction. Many factors are involved in the teaching and learning process's structure and effectiveness. Using scientific approaches to education according to patients' needs can effectively transfer knowledge and concepts and provide the ultimate goal of increasing knowledge, learning, and changing behavior. Structured and comprehensive educational programs with appropriate educational content will increase patients' awareness and enable them to participate more in self-care, increase self-efficacy, improve pain management, and reduce postoperative complications. The role of the educator, who may be a skilled, trained nurse, becomes more prominent. The importance of the art of communication, interaction, and empathy with patients in the process of education by care providers and providing feedback to patients plays a significant role in meaningful learning and control of patients' pain and anxiety.
4. Conclusions
Based on the results, almost two-thirds of previous studies reported that POE positively and significantly reduces POP. Meanwhile, the findings of one-third of the other evaluated studies showed that POE cannot have a significant impact on POP control. The effectiveness or non-effectiveness of POE on POP depends on various parameters, including the type of surgery, length of follow-up time, continuity of care, method of providing training, quality of intervention, patient awareness of pain measurement method, interactive training with empathy, and reducing anxiety. Due to the positive and significant impact of POE on POP in most studies, nurses and caregivers of patients who are candidates for surgery, according to the type of surgery, are suggested to use appropriate educational content and educational methods to reduce POP in patients. However, before that, the nurses themselves must get enough information about the different techniques of POE so that they can convey the educational content provided to the patients with proper quality and efficiency.