1. Background
In men, the testicles are in charge of producing spermatozoa and testosterone. Seminiferous tubules and germ cells make up between 80 and 90 percent of the testicle's volume (1). As a result, a decrease in these cells results in a reduction in testicular volume. According to recent research, the average testicular volume rises noticeably in the first five months, from around 0.27 to 0.44 cm3, and then declines to about 0.31 cm3 by the time a baby is nine months old (2). When diagnosing disorders that affect the testicle's development and function, it is critical to accurately and reliably measure the testicle's size. Testicle volume, like testicle length and breadth, has a clear correlation with seminal fluid and sex hormone assessment, according to studies done on infertile men (3). Touching and measuring the testicles is one of the assessment steps in a male fertility examination. Measurement of testicular volume in children is used to assess the beginning of puberty or pubertal development, whereas testicular volume in adults is used to assess spermatogenic activity (4). Additionally, the volume of the testicles may sometimes be evaluated while evaluating testicular illnesses such torsion, cryptorchidism, and varicocele. It might be difficult to diagnose scrotal and testicular diseases in children clinically. Various pathologies may have similar manifestations (5, 6).
The size of the testicles is assessed using a variety of diagnostic methods and modalities. For this, some people utilize sliding calipers in addition to common rulers, length and width indexes, and common rulers. One of the other useful methods is the orchidometer (7-9). Each of these diagnostic techniques has flaws and cannot calculate or estimate the testicular volume accurately. Ultrasound is a good method for measuring testicle size since it is accurate, dependable, affordable, accessible, and radiation-free. It may even be used on children (10, 11).
There is no fixed number and range in studies; instead, different sizes and volumes are always indicated for various ages. In a research, Sakamoto et al. used several methods to look at and measure the size of the testicles. According to their study's findings, ultrasonography is a more precise diagnostic tool than other methods, such as using a Prader orchidometer to measure the size of the testicles (1).
2. Objectives
We chose to look into the normal size and normogram of testicular volume in this research due to the fact that understanding the normal limits of testicular volume in children might detect atypical instances and associated diseases. The patients were referred to the imaging department of Pediatric Medical Center of a Hospital, Tehran, Iran.
3. Methods
3.1. Sampling
Our study was a descriptive-cross-sectional study conducted on all boys aged 0 to 15 years in Tehran, Iran. The selected samples were those who had any type of ultrasound performed from 2018 to 2023 at a pediatric hospital or a radiologist's office. In addition, samples were selected whose parents had signed a written consent form to participate in the present study. Children (0 - 15 years old) were divided into age groups with a one-year interval (15 groups). The number of samples required for each group was calculated as 55 using.
3.2. Inclusion and Exclusion Criteria
In this study, the exclusion criteria include the following items:
- Patients with incomplete information
- Those with ambiguous genitalia, hydrocele, or cryptorchidism.
- Those with a history of endocrine or genetic diseases that may affect the testicles, such as Klinefelter syndrome, tuberculosis disease, type 1 diabetes, etc
- Those with chronic debilitating diseases, such as protein-energy malnutrition and tuberculosis
- Those with testicular anomalies.
3.3. Study Implementation
In order to complete the work and avoid interfering with the patient's primary diagnostic and therapeutic process, first a questionnaire was created by the secretary and given to the child's parents. If they would agree and after receiving explanations, an ultrasound of the testicle was carried out separately from the ultrasound at no additional cost. This questionnaire collected data on people's demographics, including their age, height, weight, and BMI, in addition to information from a testicular examination. All participants who fulfilled the requirements to participate in the research were then subjected to testicular ultrasonography. A Siemens S2000 device with a linear probe and frequencies ranging from 5 to 17 MHz was used to conduct the ultrasounds. The sonographers who evaluated the documentation and results included a third-year residency student and a faculty member with 25 years of experience. Based on Sakamoto et al. study, according to the testis' elliptical sphere-like spatial form, the formula length × width × height constant number 0.71 was used to get the volume. This research shows that for determining testicular volume, the constant coefficient of 0.71 offers the maximum diagnostic precision (1). Additionally, a mathematical expert assessed the validity of the aforementioned formula and, if required, to provide a more precise formula in this field.
3.4. Statistical Analysis
All data were first entered into Excel software by the project researcher and then into SPSS-Ver.20 software for statistical analysis. Qualitative data were displayed with frequency and frequency percentage and quantitative data were displayed with mean and standard deviation. Also, statistical differences between quantitative and qualitative changes were examined by t-test and chi-square statistical tests, respectively. P-value less than 0.05 is considered statistically significant.
3.5. Ethical Considerations
All patient information will be kept confidential and will be published collectively and without mentioning the name. Whenever the patient wishes to terminate the cooperation, he can leave the study without interfering with his treatment, if during the research the patient suffers If there is a damage or a problem, his problem will be solved without wasting time. Also, patients will not incur any additional costs in conducting this research. The proposal of this plan with the code IR.TUMS.CHMC.REC.1398.128 has been approved by the ethics committee of Tehran University of Medical Sciences.
4. Results
The findings of the research indicated that the average BMI, height, weight, the left testicle, the right testicle and the overall average volume of both testicles of the patients was 18.72 ± 5.01 kg/m2, 28.8 ± 121.27 cm, 14.52 ± 25.84 kg, 2.14 ± 2.02 cc, 1.93 ± 1.74 cc and 3.42 ± 6.01 cc, respectively. The findings of the research on the comparison of average demographic indicators (BMI, weight and height) among the studied groups are shown in Table 1. The analysis of the applying ANOVA test indicated that there is a statistically significant difference between BMI in the studied groups; so that in older age groups, BMI significantly increases.
| Variables | BMI (kg/m2) | Height (cm) | Weight (kg) |
|---|---|---|---|
| Age group (y) | |||
| 0 - 1 | 15.32 ± 2.25 | 62.56 ± 12.53 | 6.69 ± 3.71 |
| 1.1 - 2 | 15.1 ± 1.45 | 81.61 ± 4.76 | 10.57 ± 1.27 |
| 2.1 - 3 | 15.63 ± 2.36 | 91.50 ± 8.38 | 13.31 ± 5.63 |
| 3.1 - 4 | 15.26 ± 2.04 | 100.56 ± 6.69 | 15.97 ± 2.25 |
| 4.1 - 5 | 14.91 ± 1.26 | 108.01 ± 6.89 | 17.67 ± 2.95 |
| 5.1 - 6 | 15.67 ± 1.74 | 112.96 ± 4.92 | 21.23 ± 3.44 |
| 6.1 - 7 | 15.85 ± 1.90 | 119.41 ± 5.51 | 24.00 ± 4.45 |
| 7.1 - 8 | 16.39 ± 2.09 | 126.34 ± 6.28 | 25.72 ± 5.25 |
| 8.1 - 9 | 18.32 ± 2.52 | 134.36 ± 6.26 | 30.64 ± 5.97 |
| 9.1 - 10 | 18.53 ± 2.62 | 144.18 ± 9.54 | 38.50 ± 8.16 |
| 10.1 - 11 | 20.47 ± 3.96 | 144.55 ± 11.57 | 30.33 ± 11.84 |
| 11.1 - 12 | 21.99 ± 3.91 | 147.09 ± 14.57 | 36.52 ± 14.16 |
| 12.1 - 13 | 24.13 ± 3.51 | 147.60 ± 17.96 | 35.70 ± 12.49 |
| 13.1 - 14 | 25.52 ± 4.03 | 148.03 ± 9.24 | 39.01 ± 18.14 |
| 14.1 - 15 | 27.34 ± 5.06 | 150.52 ± 18.85 | 41.65 ± 18.78 |
| P-value | < 0.0001 | < 0.0001 | < 0.0001 |
a Values are expressed as mean ± SD.
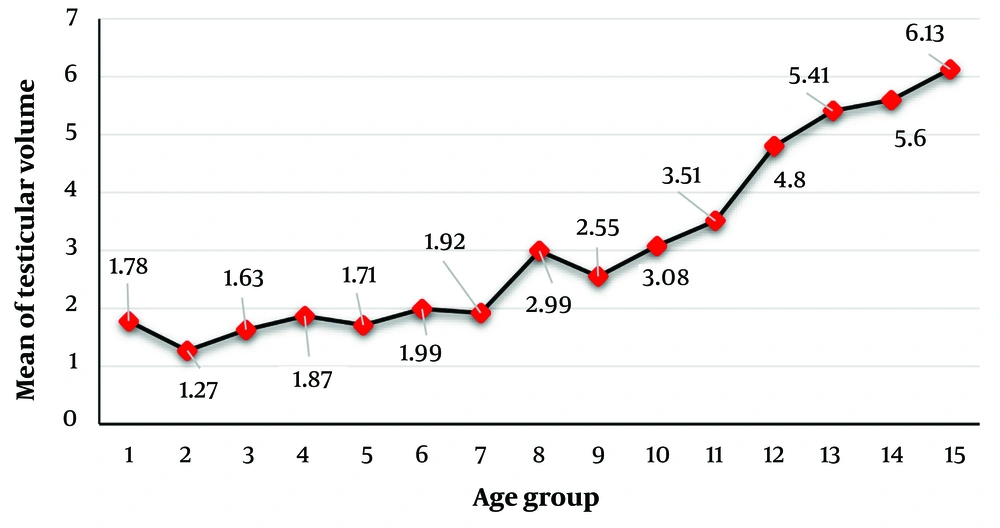
t-test analysis of the study results on the average testicular volume (right, left, and total) in the studied groups indicated that there is a statistically significant difference between the average testicular volume of the right, left, and total testicles in the studied groups; thus, the volume of the testis increases significantly with increasing age (Table 2 and Figure 1).
| Variables | Testicular Volume | ||
|---|---|---|---|
| Left (cc) | Right (cc) | General (cc) | |
| Age group (y) | |||
| 0 - 1 | 0.771 ± 1.01 | 0.808 ± 1.06 | 1.78 ± 3.17 |
| 1.1 - 2 | 0.781 ± 1.12 | 0.710 ± 0.95 | 1.27 ± 0.67 |
| 2.1 - 3 | 0.912 ± 1.03 | 0.815 ± 0.83 | 1.63 ± 0.99 |
| 3.1 - 4 | 0.922 ± 0.85 | 0.846 ± 0.81 | 1.87 ± 1.38 |
| 4.1 - 5 | 0.852 ± 0.85 | 0.867 ± 0.97 | 1.71 ± 1.35 |
| 5.1 - 6 | 0.973 ± 1.07 | 0.869 ± 0.81 | 1.99 ± 1.56 |
| 6.1 - 7 | 1.004 ± 1.24 | 0.909 ± 0.915 | 1.82 ± 1.49 |
| 7.1 - 8 | 1.56 ± 1.31 | 1.54 ± 0.75 | 2.99 ± 1.35 |
| 8.1 - 9 | 1.66 ± 1.08 | 1.53 ± 0.63 | 2.55 ± 1.22 |
| 9.1 - 10 | 2.08 ± 0.95 | 1.63 ± 0.73 | 3.08 ± 1.39 |
| 10.1 - 11 | 2.94 ± 2.47 | 2.29 ± 1.60 | 3.51 ± 2.55 |
| 11.1 - 12 | 3.92 ± 1.91 | 3.09 ± 1.33 | 4.80 ± 2.81 |
| 12.1 - 13 | 4.12 ± 1.38 | 3.84 ± 1.03 | 5.41 ± 1.68 |
| 13.1 - 14 | 4.43 ± 1.67 | 4.20 ± 1.48 | 5.60 ± 1.62 |
| 14.1 - 15 | 5.15 ± 1.59 | 4.97 ± 1.62 | 6.13 ± 1.55 |
| P-value | < 0.0001 | < 0.0001 | < 0.0001 |
a Values are expressed as mean ± SD.
The analysis of the study's findings on the average total volume of the testicles in relation to BMI, weight, and height in the analyzed patients revealed a statistically significant difference between the average total volumes of the testicles in relation to all three variables. So that, the average total testicle volume is considerably greater in patients with higher BMIs than in patients with lower BMIs, in tall patients against short patients, and in overweight patients versus low weight patients (Table 3).
| Variables | Number | General Testicular Volume a | P-Value |
|---|---|---|---|
| BMI (kg/m2) | < 0.0001 | ||
| 15 > | 170 | 1.80 ± 1.29 | |
| 15.1 - 20 | 425 | 3.15 ± 2.98 | |
| 20.1 - 25 | 125 | 4.93 ± 2.77 | |
| 25.1-30 | 76 | 5.11 ± 2.13 | |
| > 30 | 29 | 5.76 ± 1.57 | |
| Height (cm) | < 0.0001 | ||
| < 100 | 183 | 1.61 ± 1.92 | |
| 100 - 139 | 397 | 3.52 ± 1.24 | |
| ≥ 140 | 245 | 4.59 ± 2.28 | |
| Weight (kg) | < 0.0001 | ||
| > 10 | 83 | 1.34 ± 0.85 | |
| 10.1 - 25 | 381 | 3.26 ± 2.48 | |
| 25.1 - 50 | 301 | 3.81 ± 2.28 | |
| > 50 | 60 | 5.31 ± 1.93 |
a Values are expressed as mean ± SD.
The findings of the study on the correlation of TTV with BMI, height and weight variables applying Pearson's test indicated that between TTV and all three variables including BMI (r = 0.181, P < 0.0001), height (r = 0.166, P < 0.0001) and weight (r = 0.140, P < 0.0001) there is a significant positive correlation.
5. Discussion
The obtained results were showed that the mean volume of the left testicle, right testicle and the mean total volume of both testes were 2.14 ± 2.02 cc, 1.93 ± 1.74 cc and 3.42 ± 6.01 cc, respevtively. There was a statistically significant difference between the mean BMI, height and weight between the groups. Also, according to the results, a statistically significant difference was found between the mean volume of right testicle, left testicular volume and TTV in the studied groups. There was a statistically significant difference between the mean TTV in terms of BMI, height and weight; so that with the increase of the mentioned variables, TTV in the patients increased.
Sakamoto et al. examined three diagnostic approaches for measuring testis volume in their study. Prior to bilateral orchidectomy, they used Prader, orchidometer, and ultrasound to determine the size of patients' testicles (1). In the findings of Sakamoto et al. reported that the average real testis volume of the individuals analyzed was 9.3 cm3 (between 2.5 and 23.0). In addition, they reported a significant connection between the estimated testicular volume using three ultrasonography algorithms and the real volume. This study's findings suggested that evaluating testicular volume using ultrasonography is more accurate than other techniques (1). In Osemlak's research, also indicated that testis volume is the most reliable measure of testicular size, and that assessment of testis volume using ultrasound has more diagnostic value than other approaches (external linear measurement with caliper) (12). In a study conducted on 55 children and 110 testes between the ages of 1 month and 17 years by Sotos and Tokar, it was determined that a simple clinical method based on the width of the testes using a simple ruler (cm) can provide an accurate estimate of testis volume comparable to that measured by ultrasound. Additionally, ultrasonography has been able to offer reliable volume measurements for various age groups (13).
Therefore, ultrasonography was used in our study to determine testicular volume in children less than 15 years of age. The average volume of the right testicle in the studied youngsters was 1.93 cc, the average volume of the left testicle was 2.14 cc, and the average volume of the whole testicle was 3.42 cc, as determined by our research. In the research done by Atalabi et al. on 411 male neonates, the average left testicular volume was 0.276 cm3 and the average right testicular volume was 0.278 cm3. This two-sided volume average is not statistically significant (14). No statistically significant difference was detected in the volume of the left and right testicles in the research done by Osemlak (12). The average volume of the left testicle was 18.37 cm3 and the average volume of the right testicle was 18.13 cm3 according to the results of a study conducted by Bahk et al. on people with an age range of 19 to 27 years or an average age of 23.52 years (15); given that the study population of this study consisted of adult men, the larger testicle volume compared to other studies where the study population was children under 15 years old can be confirmed.
The results of our study on the factors influencing the testicular volume of children under 15 years of age revealed a significant positive correlation between the testicular volume and the following variables: Weight, BMI, and height; therefore, the testicular volume increases significantly with the increase of each of the aforementioned variables. In addition, the testicular volume of males aged 0 to 15 years increased with age; however, only weight, height, and BMI are statistically relevant in predicting testicular volume. In their research, Atalabi et al. (2015) found a significant link between testis volume and birth weight, height, and BMI of children; however, there was no significant relationship between testis size and birth age (14), which is similar to our findings. According to Osemlak's research, the primary factor influencing the size of a boy's testis is his age (12). The findings of Bahk's research revealed a modest but substantial correlation between the volume of the testicles and the weight, height, and BMI of persons (15). Lawal et al. also reported in their research that the testicle size of people was correlated with their age, weight, and height, so that only their weight, height, and BMI were adequate statistical predictors of the testicle size of people (16).
Regarding the trend of increasing testicular volume with age, our research revealed that the TTV grows with age in boys under 15 years old. Also, according to the studies, the testicle volume has significantly expanded between the ages of 8 and 12. In Osemlak's research, the testes of males began growing rapidly at the age of 10 years (12). In their research, Lawal et al. reported that the testicular volume of the children tested was 0.74 mL before the age of 9 and around 1.1 mL by the age of 9. At age 15, the average volume of the testes reached around 8.99 mL (16). According to the findings of the mentioned research, the testicle volume seems to begin increasing between the ages of 8 and 9 years.
5.1. Limitations
One of the main limitations of the present study was that samples (individuals) whose parents did not agree to participate in the study were excluded, so this event likely led to bias.
5.2. Conclusions
This research demonstrates the typical values of testicular volume determined by ultrasound in boys aged 0 to 15 years, and these values may be used as a benchmark for evaluating different testicular disorders. Also, according to the data, a substantial positive association was observed between testicular volume and the following characteristics: Weight, BMI, and height. Therefore, when each of these variables grows, so does the testicular volume. In addition, the testicular volume of males aged 0 to 15 years rose with age; however, only weight, height, and BMI are statistically relevant in predicting testicular volume.