1. Background
Coronavirus disease 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), created an unexpected crisis for the healthcare systems and is currently the most critical health threat worldwide (1). As of 22 September 2021, more than 229,373,963 patients were diagnosed with COVID-19, and more than 4,705,111 have died (2). Many observational studies have reported the risk factors for mortality in patients with COVID-19 pneumonia (3-5). Researchers showed that the increased risk of death in patients was associated with risk factors, such as older age, specific diseases, and specific laboratory parameters (6, 7). Moreover, previous studies reported that several pre-existing medical conditions, such as hypertension (HTN), diabetes, chronic obstructive pulmonary disease (COPD), and cardiovascular disease progression increased the risk of mortality in COVID-19 patients (8, 9). Numerous SARS-CoV-2 variants that have appeared worldwide and accounted for the subsequent waves have risen mortality due to COVID-19 globally (10). Most deaths in COVID-19 cases occur in patients with underlying diseases (11) and due to the low impact of vaccination on some coronavirus mutations, which are currently one of the most important factors in augmenting COVID-19 mortality (12). One of the best ways to reduce mortality in these patients is to identify and control the risk factors for mortality in COVID-19 patients with underlying diseases.
2. Objectives
The present study aimed to identify the risk factors associated with chronic diseases in the death of patients with COVID-19.
3. Methods
3.1. Study Design and Participants
This study included hospitalized adult patients aged ≥ 18 years with COVID-19 who were hospitalized in Imam Reza and Dr. Gharazi hospitals in Sirjan, Iran, during March 2020-June 2021. All adult patients with positive reverse transcriptase-polymerase chain reaction (RT-PCR) for COVID-19 who were discharged or expired were included in the study through a complete census sampling method. During the study period, 7350 patients with COVID-19 were hospitalized, while according to our inclusion/exclusion criteria, 7222 patients were evaluated. The exclusion criterion was incomplete file information.
3.2. Ethical Considerations
This study was confirmed by the Ethics Committee of Sirjan School of Medicine with the code of IR.SIRUMS.REC.1399.005 on 14 April 2020.
3.3. Data Collection
Demographic and clinical characteristics of patients were recorded by collecting data from their electronic medical records. Moreover, the outcome of hospitalized patients was recorded. Patients were divided into two groups based on the hospital outcome with and without mortality. Two faculty members of Sirjan University of Medical Sciences performed data collection. Next, the data were evaluated by an infectious disease specialist.
Data collection tools included three questionnaires:
(1) Epidemiologic information questionnaire
(2) Clinical characteristics questionnaire, including vital symptoms and clinical symptoms, such as cough, fever, dyspnea, fever, phlegm, myalgia, fatigue, diarrhea, nausea, and vomiting, as well as the severity of disease as normal, severe, or acute
(3) Questionnaire of underlying diseases included the history of diabetes, heart diseases, HTN, COPD, and cancer
3.4. Statistical Analysis
Data were entered in the SPSS version 16.0 (PASW statistics). Mean ± standard deviation and frequency (percentage) were used to describe the quantitative and qualitative data, respectively. The normal distribution of data was assessed using the Kolmogorov-Smirnov test. Chi-squared and t-test were applied for quantitative and qualitative data to compare the data between the two groups. Univariate and multivariate logistic regression tests assessed the risk factors associated with in-hospital mortality. P-value < 0.05 was considered statistically significant.
4. Results
4.1. Baseline Characteristics
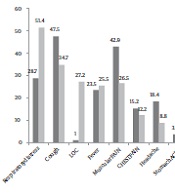
Out of 7222 patients hospitalized with COVID-19, 294 (4.1%) died. The mean age of the hospitalized patients was 48.13 ± 18.03 years. The mean age of the survivors and non-survivors was 47.27 ± 17.49 and 68.36 ± 18.61 years, respectively. Figure 1 shows the percentage of early symptoms in the living and dead subjects.
HTN was the most common underlying disease, followed by diabetes mellitus (DM), cardiac disease, and COPD. Demographics and clinical features of subjects are shown in Table 1.
| Variables | Dead (N = 294) | Alive (N = 6928) | Crude Odds Ratio (95% CI) | P-Value |
|---|---|---|---|---|
| Gender | 0.088 | |||
| Female | 142 | 3698 | 1 | |
| Male | 152 | 3230 | 1.23 (0.97, 1.55) | |
| Age group | < 0.001 | |||
| < 60 | 74 | 5196 | 1 | |
| > 60 | 220 | 1732 | 8.92 (6.82, 11.67) | |
| Inpatient department | < 0.001 | |||
| Other | 138 | 6763 | 1 | |
| ICU | 156 | 165 | 46.33 (35.15, 61.08) | |
| Previous illness | 0.869 | |||
| No | 252 | 6150 | 1 | |
| Yes | 2 | 55 | 0.88 (0.22, 3.66) | |
| Intubation | < 0.001 | |||
| No | 186 | 6819 | 1 | |
| Yes | 108 | 109 | 36.26 (26.82, 49.20) | |
| PO2 | < 0.001 | |||
| > 93 | 40 | 2656 | 1 | |
| < 93 | 254 | 4272 | 3.95 (2.82, 5.53) | |
| Smoking | 0.136 | |||
| No | 289 | 6869 | 1 | |
| Yes | 5 | 59 | 2.01 (0.80, 5.06) | |
| Addiction | < 0.001 | |||
| No | 270 | 6734 | 1 | |
| Yes | 24 | 194 | 3.09 (1.99, 4.80) | |
| Cancer | < 0.001 | |||
| No | 284 | 6908 | 1 | |
| Yes | 10 | 20 | 12.16 (5.64, 26.22) | |
| Liver disease | < 0.001 | |||
| No | 289 | 6911 | 1 | |
| Yes | 5 | 17 | 7.03 (2.58, 19.20) | |
| Diabetes | < 0.001 | |||
| No | 226 | 6326 | 1 | |
| Yes | 68 | 602 | 3.16 (2.38, 4.20) | |
| Immunodeficiency | 0.034 | |||
| No | 292 | 6919 | 1 | |
| Yes | 2 | 9 | 5.27 (1.13, 24.48) | |
| Heart disease | < 0.001 | |||
| No | 243 | 6650 | 1 | |
| Yes | 51 | 278 | 5.02 (3.63, 6.95) | |
| Kidney disease | < 0.001 | |||
| No | 283 | 6892 | 1 | |
| Yes | 11 | 36 | 7.44 (3.75, 14.77) | |
| COPD | 0.737 | |||
| No | 291 | 6870 | 1 | |
| Yes | 3 | 58 | 1.22 (0.38, 3.92) | |
| Mental disease | 0.003 | |||
| No | 287 | 6877 | 1 | |
| Yes | 7 | 51 | 3.29 (1.48, 7.31) | |
| Hypertension | < 0.001 | |||
| No | 199 | 6123 | 1 | |
| Yes | 95 | 805 | 3.63 (2.81, 4.69) |
Demographic, Clinical, Laboratory, and Radiographic Findings of Patients at Admission
4.2. Risk Factors Associated with In-Hospital Mortality
As shown in Table 1, the results of the univariate analysis revealed that age (OR = 8.92, CI: 6.82 - 11.67) was associated with hospital mortality. The odds of hospital mortality were also higher in patients with HTN (OR = 3.63, CI: 2.81 - 4.69), mental disease (OR = 3.29, CI = 1.48 - 7.31), kidney disease (OR = 7.44, CI = 3.75 - 14.77), cardiac disease (OR = 5.02, CI = 3.63 - 6.95), immunodeficiency (OR = 5.27, CI = 1.13 - 24.48), and cancer (OR = 12.16, CI = 5.64 - 26.22). In the multivariable logistic regression model, we found that mental disease (OR = 2.91, CI = 1.05 - 8.10), kidney disease (OR = 3.86, CI = 1.36 - 10.99), cardiac disease (OR = 1.60, CI = 1.01 - 2.53), immunodeficiency (OR = 9.95, CI = 1.60 - 61.82), cancer (OR = 10.79, CI = 4.00 - 29.17), and liver disease (OR = 4.75, CI = 1.12 - 2020) were associated with the increased odds of mortality. The results of examining the factors associated with the death of COVID-19 patients are demonstrated in Table 2.
| Variables | Adjusted Odds Ratio (95% CI) | P-Value |
|---|---|---|
| Age group | < 0.001 | |
| < 60 | 1 | |
| > 60 | 5.37 (3.81 - 7.58) | |
| Inpatient department | < 0.001 | |
| Other | 1 | |
| ICU | 23.9 (17.03 - 33.47) | |
| Intubation | < 0.001 | |
| No | 1 | |
| Yes | 14.67 (9.60 - 22.40) | |
| PO2 | < 0.001 | |
| > 93 | 1 | |
| < 93 | 2.56 (1.71 - 3.84) | |
| Addiction | 0.113 | |
| No | 1 | |
| Yes | 1.61 (0.89 - 2.88) | |
| Cancer | < 0.001 | |
| No | 1 | |
| Yes | 10.79 (4.00 - 29.17) | |
| Liver disease | 0.035 | |
| No | 1 | |
| Yes | 4.75 (1.12 - 20.20) | |
| Diabetes | 0.314 | |
| No | 1 | |
| Yes | 1.25 (0.81 - 1.92) | |
| Immunodeficiency | 0.014 | |
| No | 1 | |
| Yes | 9.95 (1.60 - 61.82) | |
| Heart disease | 0.045 | |
| No | 1 | |
| Yes | 1.60 (1.01 - 2.53) | |
| Kidney disease | 0.011 | |
| No | 1 | |
| Yes | 3.86 (1.36 - 10.99) | |
| Mental disease | 0.041 | |
| No | 1 | |
| Yes | 2.91 (1.05 - 8.10) | |
| Hypertension | 0.417 | |
| No | 1 | |
| Yes | 1.18 (0.79 - 1.77) |
Risk Factors Associated with In-Hospital Mortality
Logistic regression simultaneously examined the effect of the variables shown to be significant in Table 1 (multiple logistic regression). In this model, variables or P-value < 0.05 were entered into the adjusted model. Based on the results obtained in this analysis, although the variables of addiction, diabetes, and blood pressure raised the chance of death, they were not significant in the simultaneous analysis with other variables.
5. Discussion
The findings of the present study showed no significant difference between genders in terms of the mortality rate of patients with coronavirus, while a study conducted in European countries indicated that the death rate was higher in men than in women of all ages, especially in the middle age. This difference might be due to sex hormones and the angiotensin-converting enzyme (ACE)-2 receptor (13). Another research found that men were more prone to intubation, more hospitalized, and had a higher mortality rate following COVID-19 than women (14). In the present study, the mortality rate increased with age, which has been observed in various studies. In a study in China, the overall mortality rate in patients with COVID-19 was 2.3%, which had risen sharply between the ages of 70 and 79, reaching 8% (15).
In one study, the needed characteristics for patients to be admitted to the ICU were defined. Patients who needed to be admitted to the ICU had a higher mortality rate, which is in line with the results of the present study (16). In addition, we observed that most of the patients who lost their lives were intubated, which indicates the weakness of patients. Another study revealed that about 76% of intubated patients died (17). In the present study, there was no significant relationship between smoking and mortality, while a meta-analysis reported that patients who smoked experienced more severe COVID-19 symptoms and had a higher mortality rate (18). An investigation also showed that substance abuse could make COVID-19 symptoms worse, which was also confirmed in the present study (19). Moreover, it has been demonstrated that the paO2 level could be used as a predictor of mortality, which was also observed in the current study (20).
We found that COVID-19 patients with cardiovascular disease had a higher mortality rate, which has been reported in several studies (21-23). Our results showed no significant relationship between previous diseases and mortality rate. This finding in cardiac patients in the study proved that previous history of cardiovascular disease had no relationship with a mortality rate (24). A meta-analysis in Iran showed that the most common underlying disease that could cause death in people with COVID-19 was HTN, which is found in more than 21% of people, followed by diabetes (16.3%), heart disease (14%), and kidney disease (5%), which could lead to death (25). However, another meta-analysis showed that diabetes, chronic lung disease, and malignancies predict patient mortality (26). In the present study, most dead people had HTN, and diabetes was reported in the second place.
A meta-analysis of more than 3.8 million patients with COVID-19 indicated that patients under 70 years of age with chronic kidney disease were more likely to die than those over 70 with no kidney disease. Kidney disease alone can increase the mortality rate in patients with chronic kidney diseases (27), which was also observed in the present study. A meta-analysis published in 2021 found that patients with COPD were three times more likely to die from COVID-19 (28), while the present study did not report a significant relationship between COPD and death. The latter result could be due to the lack of proper diagnosis of COPD in patients. Liver patients were also found to have a higher mortality rate in the present study. In this regard, a study stated that high liver enzymes at the time of the admission of patients could be associated with an augmented mortality rate. On the other hand, hepatitis B was not significantly related to the death rate due to COVID-19 (29).
Furthermore, a study that analyzed more than 19,000 patients reported that the severity of symptoms and death rates were higher in patients with mental disorders (30), which was also found in the present study. The mentioned finding may result from not receiving a vaccine or being unable to care for themselves. Concerning the immune system, the present study suggests that people with a defective immune system are more likely to die from COVID-19, which was also found in another study in the United Kingdom that found that people with a primary or secondary defect were more likely to die. They have a higher mortality rate than the normal population (31).
In another study, dyspnea, weakness, and myalgia were mentioned as three common symptoms in patients who died due to coronavirus infection (26), while in the present study, three common signs of dyspnea, cough, and loss of consciousness were observed. One of the most common symptoms experienced in patients before death due to COVID-19 was the loss of consciousness. Various studies have proven this finding that dementia can be used as a predictor of death in COVID-19 patients (32). Another symptom that patients who died of COVID-19 experienced was fever which was found more than in the surviving patients. In the present study, more than 25% of patients who died experienced fever, which was in line with a study conducted in the United States of America. Fever has also been confirmed to predict patients' death (33).
The limitation of this study was the lack of some information in the patients' files. It is recommended that future studies investigate the relationship between the treatment process and mortality rates of patients. Moreover, evaluating the mortality rate of patients with COVID-19 who have been vaccinated is suggested. Furthermore, prospective cohort studies can provide more information about the consequences of this disease.
5.1. Conclusions
This study showed that underlying diseases could be associated with an increased mortality rate in patients with COVID-19. Among the underlying diseases, blood pressure ranks first, and diabetes ranks second. Moreover, respiratory distress and decreased consciousness can be intense symptoms to predict death. It might be proper for the initial determination of patients who may need life-saving interventions. In addition, these results can be useful for managing COVID-19 and controlling the risk factors associated with mortality due to this disease.