1. Background
Infertility is defined as the inability to conceive after a year of regular, unprotected intercourse. Infertility is categorized into primary and secondary infertility. There is no history of a complete pregnancy in primary infertility, while in secondary infertility, there has been at least one pregnancy resulting in the delivery of a newborn (1). Infertility is estimated to affect 8 - 12% of couples in the reproductive age worldwide (2). According to the World Health Organization (WHO), 10 - 15% of women are infertile all over the world (3). A study reported that 17.3% of Iranian women currently have infertility. Male partners are the primary cause in 29.1% of the cases, while ovarian problems account for 39.7% (4).
Infertility can be a frustrating, emotional experience. It may cause several psychological issues such as tension, anxiety, depression, low self-esteem, and sexual dissatisfaction (5). The resulting psychosocial issues adversely affect females more than males (6, 7), especially in societies where childbearing is considered a fundamental task for women (4, 8, 9). Therefore, an infertile woman may present with high irritability, which affects her relationship with others, including her spouse. Likewise, infertile women are more likely to develop mental illnesses, marital dissatisfaction, and impaired quality of life than fertile individuals (10). While 20 - 30% of infertility cases are attributed to men, in reality, more than 50% of the cases can be explained by men’s health issues (2).
Although infertility is considered a catastrophic phenomenon for couples worldwide, studies show that the adverse psychological effects of infertility are more significant among women than men (2). This is because motherhood has traditionally been accepted as an essential role for women in the Iranian culture. An infertile woman often believes that she cannot imagine a childless life while her spouse may express a different feeling (11, 12). In general, infertile women are more likely than men to seek treatment because of which either the woman or the spouse goes through emotional and financial hardships (13). Studies have reported many complications such as fatigue, depression, stress, and lack of self-esteem as the psychological consequences of infertility among infertile women (12, 14, 15).
Sexual satisfaction is also unfavorably affected by infertility due to decreased self-esteem, depression, and anxiety (15). Sexual dissatisfaction may contribute to the failure of the couple to conceive and may create a defective cycle in which sexual dissatisfaction leads to infertility and vice versa. A depressed woman may feel hopeless, helpless, worthless, or guilty. She may even lose her desire to engage in sexual activity (16, 17). According to a study, 50 - 60% of couples reported significantly reduced sexual satisfaction during the course of infertility treatment (3). Decreased sexual satisfaction has other underlying causes such as a history of trauma, rape, mental illnesses, and divorce (18-20).
Both mental health and sexual satisfaction are psychological factors that may be adversely affected by infertility and the treatment process. Lack of attention to emotional disorders of an infertile couple and infertility consequences such as unfavorable interpersonal relationships, marital dissatisfaction, and decreased sexual desire has created a defective cycle that reduces the success of treatment (21, 22). Due to fertility's social and cultural values in Iran, the study of infertility is imperative (4, 9, 12). Previous studies in Iran were not conducted based on a case-control study design (23, 24).
2. Objectives
The purpose of this study was to compare the severity of depression and sexual dissatisfaction among fertile and infertile women in Iran.
3. Methods
3.1. Study Design and Setting
This case-control study was performed in gynecological hospitals and gynecologists’ offices. Data were collected from April to December 2019.
3.2. Sampling
In this study, the participants were selected from the residents of Lorestan province, Iran, using a combination of multistage and cluster sampling methods. Five politically, socio-economically, and geographically scattered cities in the province were studied. A total of nine clusters were identified in each city. Each cluster represented one of the counties of the province. Five out of the nine clusters were randomly selected based on probability sampling, so the greater was the city population, the more was the selection likelihood. There were two classifications for infertile women in each city. The first category consisted of women referred to gynecological hospitals or infertility clinics selected by non-probability sequential sampling. This means that information on infertile women was collected sequentially until the number of cases and the required information were completed. The second category consisted of women referred to gynecologists’ offices. In each geographic area, two to four offices were selected using systematic random sampling. In each gynecologist’s office, non-probability sequential sampling was used to select the participants.
The process of matching was done individually. For each case, three controls were matched, making the case and control groups as similar as possible, except for the main study variable. In addition, the effects of confounding variables were controlled using an accurate statistical model in contrast to previous studies.
Infertility was defined as the inability to conceive after a year of regular, unprotected intercourse. The inclusion criteria for the control group included not suffering from infertility, not being pregnant during the study, and at least a four-month interval between the last delivery and the start time of the study. Having Persian literacy skills was also one of the inclusion criteria for both case and control groups. The exclusion criteria consisted of having a history of drug abuse, mental or physical disorders, death of loved ones over the previous two years, and unwillingness to participate in the study.
Taking into account α = 0.05, P = 0.11, and d = 0.05, and according to the following formula, the sample size was equal to 150 people for the case group. By a 20% drop-out correction, this amount equaled 180 people. Each participant of the case group was matched with three participants in the control group. A total of 540 women were selected for the control group, resulting in a sample size of 720 people.
3.3. Questionnaire
The questionnaire consisted of three parts.
3.3.1. Demographics
The first part of the questionnaire included items related to the demographic and background information of the participants, such as age, employment status, education of the couple, marriage duration, homeownership, consanguineous marriage, history of illnesses, household income, exposure to toxins, infertility type, and infertility treatment costs.
3.3.2. Beck Depression Inventory
The second part of the questionnaire mainly included the Beck Depression Inventory scale. The depression inventory, second edition, consists of 21 standardized questions. This questionnaire is not a diagnostic instrument but a screening tool to measure the depression severity from mild to severe. Each item has four choices where a score of 0 to 3 indicated a normal to the severe state of the disorder, respectively. A total score of 0 - 9 is considered normal, whereas 10 - 16 indicates mild depression. Likewise, a score of 17 - 29 points to a medium level of depression, and a score of 30-63 suggests the presence of severe depression. Therefore, the scores range from 0 to 63. This questionnaire has a reliability of 0.71 (25). The psychometric assessment of this questionnaire in Iran indicated that the split-half reliability is 0.89, while the test-retest reliability with a one-week interval is 0.94 (26). Internal consistency (Cronbach's alpha) was used to assess the reliability of this questionnaire. The Cronbach's alpha calculated for a sample of 30 participants was 0.91.
3.3.3. Sexual Satisfaction
The questionnaire was developed by Linda Berg in 1997. The validity and reliability of this instrument have been established in previous Iranian studies (23, 24). Sexual satisfaction in this study is shown by the participant's score on the sexual satisfaction scale. It consists of 25 questions rated on a five-point Likert scale by selecting 'always,' 'often,' 'sometimes,' 'rarely,' and 'never' options. The answers ‘never’ to ‘always’ are scored from 1 to 5, respectively. The total score ranges from 17 to 85. Scores from 11 to 17 show poor sexual satisfaction, 67 to 52 indicate modest sexual satisfaction, and 68 to 85 display good sexual satisfaction.
3.4. Statistical Analysis
Frequency, mean, and standard deviations were used to describe the variables. Since the individual-to-individual matching method was used and the data were of a quadratic matching type, for both univariate and multivariate data modeling, the marginal model, specifically the generalized estimation equation (GEE) method, was employed for parameter estimation. Basically, GEE was utilized to estimate the parameters of a generalized linear model with an uncertain correlation between the outcomes (27).
First, the marginal GEE model compared the demographic and contextual variables among fertile and infertile women. This GEE method used the logit link function with the exchangeable covariance matrix structure. The "infertility status" was considered the dependent variable in each GEE, and a single demographic predictor variable was identified as the independent variable. Another marginal GEE model was used to determine the relationship of depression severity and sexual satisfaction with demographic variables. In these GEEs, a cumulative logit regression function was employed. In each GEE, the depression severity and sexual satisfaction were the dependent variables, while the demographics were considered the predicting variables.
The effect of confounding variables was controlled in the study. Since this study aimed to investigate the effect of infertility on depression severity and sexual satisfaction of women, variables with p-values of less than 0.25 were selected in the univariate approach and were included in the multivariate modeling (28-30). Demographic and contextual variables that were significantly or nearly related to both infertility and depression severity/sexual satisfaction were considered the confounding variables.
For multivariate modeling, the cumulative logit link function with exchangeable structure was used for the correlation matrix in the GEE model. Depression severity/sexual satisfaction and infertility status were the dependent and independent variables, respectively. Confounding variables such as homeownership, history of underlying illnesses, and consanguineous marriage were selected for the multivariate model. Finally, the chi-square test and Fisher's exact test were used to investigate the relationship of infertility type, infertility treatment type, and costs with depression severity and sexual dissatisfaction. Data analysis was done by SPSS version 21 software at a significance level of 0.05.
3.5. Ethical Consideration
The study was approved by the Ethics Committee of the Lorestan University of Medical Sciences with a code of lums.REC.1395.81. The participants were informed of the study objectives. Each participant completed a consent form before enrollment in the study. To let participants be comfortable, a female administrator interviewed them, and they were promised that the collected information would be kept confidential.
4. Results
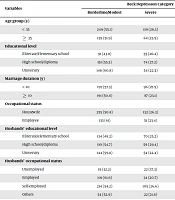
In the present study, 180 infertile women and 540 fertile women were selected from different cities of Lorestan, Iran. The mean age of cases and controls was 33.19 ± 5.9 and 33.11 ± 4.9 years, respectively (Table 1). Primary infertility was recognized as the most common cause of the inability to reproduce (91.1%). The most frequent treatment methods were IVF (45.6%) and drug therapy (43.8%). Among the cases and controls, 70.6% and 69.4% were housewives, respectively (Table 1).
| Variables | Fertility | P-Value | |
|---|---|---|---|
| Fertile | Infertile | ||
| Age group (y) | > 0.999 | ||
| < 35 | 339 (62.8) | 113 (62.8) | |
| ≥ 35 | 201 (37.2) | 67 (37.2) | |
| Educational level | > 0.999 | ||
| Illiterate/elementary school | 156 (28.9) | 52 (28.9) | |
| High school diploma | 204 (37.8) | 68 (37.8) | |
| University | 180 (33.3) | 60 (33.3) | |
| Marriage duration (y) | > 0.999 | ||
| < 10 | 258 (47.8) | 86 (47.8) | |
| ≥ 10 | 282 (52.2) | 94 (52.2) | |
| Occupational status | 0.719 | ||
| Housewife | 375 (69.4) | 127 (70.6) | |
| Employee | 165 (30.6) | 53 (29.4) | |
| Husbands’ educational level | 0.632 | ||
| Illiterate/elementary school | 205 (38) | 73 (40.6) | |
| High school diploma | 152 (28.1) | 49 (27.2) | |
| University | 183 (33.9) | 58 (32.2) | |
| Husbands’ occupational status | 0.463 | ||
| Unemployed | 40 (7.4) | 19 (10.6) | |
| Employed | 126 (23.3) | 38 (21.1) | |
| Self-employed | 296 (54.8) | 99 (55) | |
| Other | 78 (14.4) | 24 (13.3) | |
| Homeownership | 0.079 | ||
| Rented/living in parental housing | 143 (26.5) | 59 (32.8) | |
| Owned | 397 (73.5) | 12 (67.2) | |
| Household income (IRRs) | 0.787 | ||
| < 10000,000 | 115 (21.3) | 42 (23.3) | |
| 10,000,000 - 10,999,999 | 164 (30.4) | 55 (30.6) | |
| ≥ 20,000,000 | 261 (48.3) | 83 (46.1) | |
| Consanguineous marriage | 0.155 | ||
| No | 352 (65.2) | 106 (58.9) | |
| Yes | 188 (34.8) | 74 (41.1) | |
| History of specific disease | 0.003 | ||
| No | 484 (89.6) | 144 (80) | |
| Yes | 56 (10.4) | 36 (20) | |
| Toxin exposure | 0.273 | ||
| No | 506 (93.7) | 164 (91.1) | |
| Yes | 34 (6.3) | 16 (8.9) | |
| Type of infertility | |||
| Primary | 164 (91.1) | ||
| Secondary | 16 (8.9) | ||
| Costs of infertility treatment (US$) | |||
| < 1500 | 35 (19.4) | ||
| ≥ 1500 | 145 (80.6) | ||
| Type of infertility treatment | |||
| Drug therapy | 79 (43.8) | ||
| Surgery | 9 (5.0) | ||
| IVF | 82 (45.6) | ||
| ICSI/IUI | 10 (5.6) | ||
The marginal model with the logit link function showed a significant difference between the two groups of fertile and infertile women in the distribution of underlying diseases’ history (P = 0.003). There was also a significant difference between the two groups regarding the distribution of homeownership and consanguineous marriage (P = 0.07 and P = 0.155, respectively). Based on the aforementioned marginal model, there was no statistically significant difference between the two groups in terms of other underlying and demographic variables (P > 0.05) (Table 1).
Table 2 shows the relationship of depression severity and sexual satisfaction with demographic and underlying variables in women. Confounding variables that correlated with fertility status, depression severity, and sexual satisfaction can be observed in Tables 1 and 2. The marginal model showed that after adjustment for the effects of confounding variables (including marital duration, history of underlying diseases, and consanguineous marriage), infertility increased the odds of relatively high levels of depression by approximately 2.305 times (OR = 2.305, 95% CI = 14.75 - 32.021, P < 0.001). The marginal model showed that after adjustment for the effects of confounding variables (including marital duration, underlying disease history, and consanguineous marriage), infertility increased the chance of a relatively low level of marital satisfaction by 15.560 times (OR = 15.560, 95% CI = 5.089 - 47.571, P < 0.001).
| Variables | Beck Depression Category | P-Value | Sexual Satisfaction Category | P-Value | |||
|---|---|---|---|---|---|---|---|
| Borderline/Modest | Severe | Extreme | Weak/Modest | Good | |||
| Age group (y) | 0.147 | 0.165 | |||||
| < 35 | 249 (55.1) | 119 (26.3) | 84 (18.6) | 12 (2.7) | 440 (97.3) | ||
| ≥ 35 | 139 (51.9) | 64 (23.9) | 65 (24.3) | 12 (4.5) | 256 (95.5) | ||
| Educational level | < 0.001 | 0.026 | |||||
| Illiterate/elementary school | 91 (43.8) | 55 (26.4) | 62 (29.8) | 12 (5.8) | 196 (94.2) | ||
| High school/diploma | 151 (55.5) | 74 (27.2) | 47 (17.3) | 10 (3.7) | 262 (96.3) | ||
| University | 146 (60.8) | 54 (22.5) | 40 (16.7) | 2 (0.8) | 238 (99.2) | ||
| Marriage duration (y) | 0.001 | 0.058 | |||||
| < 10 | 197 (57.3) | 96 (27.9) | 51 (14.8) | 7 (2) | 337 (98) | ||
| ≥ 10 | 191 (50.8) | 87 (23.1) | 98 (26.1) | 17 (4.5) | 359 (95.5) | ||
| Occupational status | 0.002 | 0.030 | |||||
| Housewife | 255 (50.8) | 132 (26.3) | 115 (22.9) | 22 (4.4) | 480 (95.6) | ||
| Employee | 133 (61) | 51 (23.4) | 34 (15.6) | 2 (0.9) | 216 (99.1) | ||
| Husbands’ educational level | 0.001 | 0.054 | |||||
| Illiterate/elementary school | 134 (48.2) | 70 (25.2) | 74 (26.6) | 12 (4.3) | 266 (95.7) | ||
| High school/diploma | 110 (54.7) | 59 (29.4) | 32 (15.9) | 10 (5) | 191 (95) | ||
| University | 144 (59.8) | 54 (22.4) | 43 (17.8) | 2 (0.8) | 239 (99.2) | ||
| Husbands’ occupational status | 0.001 | 0.113 | |||||
| Unemployed | 19 (32.2) | 22 (37.3) | 18 (30.5) | 5 (8.5) | 54 (91.5) | ||
| Employed | 101 (61.6) | 34 (20.7) | 29 (17.7) | 3 (1.8) | 161 (98.2) | ||
| Self-employed | 214 (54.2) | 105 (26.6) | 76 (19.2) | 13 (3.3) | 382 (96.7) | ||
| Others | 54 (52.9) | 22 (21.6) | 26 (25.5) | 3 (2.9) | 99 (97.1) | ||
| Homeownership | 0.323 | 0.575 | |||||
| Rented/living in parental housing | 102 (50.5) | 53 (26.2) | 47 (23.3) | 8 (4) | 194 (96) | ||
| Owned | 286 (55.2) | 130 (25.1) | 102 (19.7) | 16 (3.1) | 502 (96.9) | ||
| Household income (IRRs) | < 0.001 | 0.011 | |||||
| < 1000,000 | 61 (38.9) | 49 (31.2) | 47 (29.9) | 11 (7) | 146 (93) | ||
| 1000,000 - 1999,000 | 108 (49.3) | 69 (31.5) | 42 (19.2) | 5 (2.3) | 214 (97.7) | ||
| ≥ 2000,000 | 219 (63.7) | 65 (18.9) | 60 (17.4) | 8 (2.3) | 336 (97.7) | ||
| History of specific disease | < 0.001 | 0.003 | |||||
| No | 359 (57.2) | 154 (24.5) | 115 (18.3) | 16 (2.5) | 612 (97.5) | ||
| Yes | 29 (31.5) | 29 (31.5) | 34 (37) | 8 (8.7) | 84 (91.3) | ||
| Consanguineous marriage | 0.082 | 0.030 | |||||
| No | 258 (56.3) | 112 (24.5) | 88 (19.2) | 10 (2.2) | 448 (97.8) | ||
| Yes | 130 (49.6) | 71 (27.1) | 61 (23.3) | 14 (5.3) | 248 (94.7) | ||
| Toxin exposure | < 0.001 | 0.039 | |||||
| No | 374 (55.8) | 169 (25.2) | 127 (19) | 20 (3) | 650 (97) | ||
| Yes | 14 (28) | 14 (28) | 22 (44) | 4 (8) | 46 (92) | ||
The chi-square test (Monte Carlo simulation) showed no significant relationship between depression severity and infertility type in infertile women (P = 0.856) (Table 3). Besides, Fisher's exact test showed no significant relationship between infertility type and sexual satisfaction (P = 0.701) (Table 4). The chi-square test results (Monte Carlo simulation) showed a significant relationship between infertility treatment and depression severity among infertile women (P = 0.001). Most cases of severe depression belonged to the IVF treatment group, while the fewest cases appeared in the IUI/ICSI group. The chi-square test (Monte Carlo simulation) showed no significant relationship between infertility treatment and sexual satisfaction level in infertile women (P = 0.242). However, most women who were mildly to moderately satisfied with their sexual relationship were seen in the surgical treatment group, followed by the IVF group (22.2% and 14.6%, respectively) (Table 5).
| Model and Fertility Status | Regression Coefficient | Standard Error | Odds Ratio | 95% Confidence for Odds Ratio | P-Value |
|---|---|---|---|---|---|
| Modeling the Effect of Female Infertility on Depression Severity | |||||
| Without adjustment | |||||
| Infertile | 3.052 | 0.205 | 21.164 | 14.172 - 31.603 | < 0.001 |
| Fertile | Base category | ||||
| With adjustment | |||||
| Infertile | 3.052 | 0.208 | 21.305 | 14.175 - 32.021 | < 0.001 |
| Fertile | Base category | ||||
| Modeling the Effect of Female Infertility on Sexual Satisfaction | |||||
| Without adjustment | |||||
| Infertile | 2.818 | 0.563 | 16.750 | 5.557 - 50.492 | < 0.001 |
| Fertile | Base category | ||||
| With adjustment | |||||
| Infertile | 2.745 | 0.570 | 15.560 | 5.089 - 47.571 | < 0.001 |
| Fertile | Base category | ||||
| Type of Infertility | Depression Severity | P Value | Sexual Satisfaction Level | P Value | |||
|---|---|---|---|---|---|---|---|
| Modest/Borderline | Severe | Very Severe | Modest/Poor | Good | |||
| Primary infertility | 15 (9.1) | 47 (28.7) | 102 (62.2) | 0.856 | 19 (11.6) | 145 (88.4) | 0.701 |
| Secondary infertility | 2 (12.5) | 5 (31.3) | 9 (56.3) | 1 (6.3) | 15 (93.8) | ||
Relationship of Depression Severity and Sexual Satisfaction with Infertility in Infertile Women a
| Method of Infertility Treatment | Depression Severity | P-Value | Sexual Satisfaction Levels | P-Value | |||
|---|---|---|---|---|---|---|---|
| Borderline/Modest | Severe | Very Severe | Modest/Poor | Good | |||
| Drug therapy | 12 (15.2) | 28 (35.4) | 39 (49.4) | 0.001 | 5 (6.3) | 74 (93.7) | 0.242 |
| Surgery | 2 (22.2) | 2 (22.2) | 5 (55.6) | 2 (22.2) | 7 (77.8) | ||
| IVF | 3 (3.7) | 15 (18.3) | 64 (78) * | 12 (14.6) | 70 (85.4) | ||
| IUI/ICSI | 0 (0) | 7 (70) | 3 (30) | 1 (10) | 9 (90) | ||
Relationship of Depression Severity and Sexual Satisfaction with Infertility Treatment in Infertile Women a
The chi-square test (Monte Carlo simulation) showed no significant relationship between infertility treatment costs and depression severity (P = 0.098). As such, the prevalence of severe depression was higher among women who spent more than 50 million Iranian Rials (about 1,187 US$) for infertility treatment than in those who paid less (65.5 vs. 45.7%). Fisher’s exact test showed no significant relationship between sexual satisfaction and infertility treatment costs (P = 0.373). However, it seems that women who spent more than 50 million Iranian Rials for infertility treatment were less satisfied than those who paid less (12.4 vs. 5.7%) (Table 6).
| Infertility Treatment Costs | Depression Severity | P-Value | Sexual Satisfaction Level | P-Value | |||
|---|---|---|---|---|---|---|---|
| Borderline/Poor | Severe | Very Severe | Poor/Modest | Good | |||
| > 50 million IRRs | 5 (14.3) | 14 (40) | 16 (45.7) | 0.098 | 2 (5.7) | 33 (94.3) | 0.373 |
| ≤ 50 million IRRs | 12 (8.3) | 38 (26.2) | 95 (65.5) | 18 (12.4) | 127 (87.6) | ||
| Total | 17 (9.4) | 52 (28.9) | 111 (61.7) | 20 (11.1) | 160 (88.9) | ||
Relationship of Infertility Treatment Costs with Depression Severity and Sexual Satisfaction a
5. Discussion
According to the results, infertile women were 21 times more likely to develop depression than fertile ones. After adjusting for confounding variables such as marriage duration, history of underlying illnesses, and consanguineous marriage, the chance of developing depression remained higher in infertile than fertile women by several times. Since an infertile person cannot go through the reproduction process, she turns this failure into a socio-psychological crisis. A previous study in Iran measured psychological symptoms among infertile women using an instrument similar to the one used in the present study and found infertility as a source of anxiety and depression among infertile Iranian women (12).
Based on a qualitative study that examined the experiences of infertile Nigerian women, most women expressed anxiety and depression as a result of their inability to get pregnant. They also suffered from social self-isolation and marital problems (31). Likewise, a study measured psychological distress in infertile couples using an instrument similar to the present study instrument and showed that about 10% of the participants experienced clinical symptoms of anxiety and depression (15). The present study results are consistent with previous studies showing that anxiety and depression are common manifestations among infertile women.
According to the current study results, the chance of insufficient sexual satisfaction was 15 times higher among infertile women than fertile women. Based on a few Iranian studies, infertile couples' well-being and relationships are more likely to be affected by infertility in countries where girls are trained and expected to be mothers later on (12, 32-37). Various studies have already measured the levels of sexual satisfaction among infertile women using different instruments. For example, a previous study conducted in Iran measured the levels of sexual satisfaction using the Female Sexual Function Index Questionnaire, which showed that the levels of satisfaction are significantly lower in the infertile group than in the fertile group (36). These findings show that sexual satisfaction in infertile Iranian women is assessed similarly by different questionnaires. Likewise, a meta-analysis without language restriction on 11 comparative studies showed that infertility was associated with increased sexual dysfunction (38).
According to the results of previous studies in Iran, the prevalence of sexual dissatisfaction was significantly higher in infertile women than in their husbands, which indicates infertile women were more affected by psychological complications of infertility than their spouses (39). In addition, men and women may differ in their perceptions of sexual satisfaction. For example, a study of 113 infertile couples who attended an infertility clinic showed that a higher proportion of women believed their partners did not understand how infertility issues impacted their marital life. This can be an origin of concern about the longevity of their relationships. In contrast, men reported a significantly lower quality of sex than women (40).
The present study demonstrated that depression severity increased over time in infertile women who received IVF treatment. A systematic review reported that multiple failed IVF treatment attempts might increase the likelihood of developing unfavorable mood conditions, especially depression. For instance, infertility treatment affects changes in an infertile woman's perception, marital relationship, and personality (41).
Previous studies have also shown that infertility treatment can sometimes predict infertility-related stress compared to pregnancy (42, 43). It may be thought that seeking fertility may take the form of obsessive-compulsive behavior, possibly affecting the couples' self-esteem and identity. Couples may feel being responsible for pregnancy outcomes, which raises concerns. This causes couples to neglect other aspects of life, making them susceptible to depressive traits such as declined social and physical activity and decreased interest in daily life (44). There is a mutual relationship between depression and infertility treatment. In a study conducted in North Carolina, the U.S., infertile women who had already started treatment were given the NIH PROMIS screening questionnaire for mental disorders. Infertile women who suffered from depression were less likely to follow oral or IVF treatments than infertile women who were not depressed (45).
The current study demonstrated that low sexual satisfaction was commonly seen in women undergoing infertility treatment through surgery and IVF. Couples' focus on pregnancy may diminish their interest in sexual activity. In addition, sexual problems in infertility treatment may be attributed to hormonal changes produced from medical treatments such as surgery or IVF (46). A previous study in Iran showed that poor general health, stress, and marital dissatisfaction were associated with IVF treatment in infertile women (47). In a study of three target groups, including a successful IVF treatment group, an unsuccessful IVF treatment group with a step kid, and an unsuccessful IVF treatment group with no step kid, there were no significant differences between them regarding sexual satisfaction. They did not have sexual satisfaction (48). This may indicate the negative impact of IVF treatment on sexual satisfaction. Studies show that people who find fertility through medical treatment can experience anxiety, stress, depression, and sexual concerns related to infertility. When infertile women become pregnant utilizing reproductive medical assistance, they show a more significant decline in sexual satisfaction if previously exposed to stressors (49).
In addition, the present study demonstrated that relatively high levels of depression and low levels of sexual satisfaction were seen among infertile women if treatment costs were at least 50 million Iranian Rials. In a study of 85 infertile Iranian women referred to a public clinic to assess sexual satisfaction, treatment costs were significantly associated with sexual function. Women identified as positive in depression screening are more prone to long-term infertility. In contrast, infertile women who are not depressed are less likely to start and continue infertility treatment (50).
The study has many strengths, and the validity of the results is verifiable. The study was a case-control study within a cohort of Lorestan, Iran, which enabled us to minimize the risk of selection bias. Likewise, confounding factors were well identified. Data about confounding variables were available, and their effects were controlled over the multivariate marginal model. Nonetheless, the present study was not without limitations. Because marital issues are considered an extremely private topic, and there are cultural and religious restrictions on this point in Iran, people may not be able to open up and tell the truth. Therefore, the inability of most individuals to express themselves explicitly was beyond the reach of the researchers, so the present study only included the psychological assessment of women. For future studies, it is suggested that data from both women and their spouses be examined simultaneously. In addition, considering that this is a non-longitudinal case-control study, it was difficult to control for some confounding variables. Therefore, prospective longitudinal studies are recommended on this issue.
5.1. Conclusions
The present study showed that depression severity and sexual dissatisfaction were more in the infertile group than the fertile group. There was also a significant relationship between infertility treatment type and depression severity in infertile women. Most cases of very severe depression were seen in the IVF treatment group, which causes a defective cycle and exacerbates depression due to infertility and sexual satisfaction problems. This may reduce treatment success and fertility chances. Therefore, screening women for depression by health personnel is influential because follow-up and subsequent interventions may improve fertility treatment compliance, life quality, and overall sexual pleasure. It is suggested that psychiatric counseling services be available in all infertility treatment centers to address the psychological and behavioral needs and problems of infertile patients from diagnosis to the end of the treatment process.