1. Background
Streptococcus pneumoniae is a major cause of invasive diseases such as meningitis, septicemia and pneumonia. Approximately one million children under five years of age die of pneumococcal disease annually. In addition, the morbidity by S. pneumoniae through respiratory tract infections such as otitis media and sinusitis is enormous. Almost 30% to 50% of all patients with otitis media and a substantial percentage of cases of sinusitis and pneumonia are caused by pneumococci. Risk groups for serious pneumococcal disease include children under the age of two years, elderly and patients with immunodeficiencies (1).
The prevalent serotype distribution had been investigated in Egypt through two surveillance studies, the first one of them was conducted in a network of hospitals across Egypt, during a five-year year period (1998 - 2003) (2). The second study was a laboratory-based surveillance of patients with bacterial meningitis (1998 - 2004). Both studies were concerned with the pneumococcal meningitis only and other types of pneumococcal diseases were not addressed (3). The pneumococcal isolates were serotyped using latex agglutination and the Quellung reaction for confirmation and in both studies, serotypes 6B, 1, 19A, 23F and 6A were the most prevalent in Egypt (2, 4).
The high cost of antisera, subjectivity in interpretation, and technical expertise requirements associated with serologic methods for S. pneumoniae serotyping have resulted in the development of PCR-based serotyping systems. PCR-based serotyping has the potential to overcome some of the difficulties associated with serologic testing and assays for direct detection of serotypes from clinical specimens and is a valuable aid in surveillance, particularly in situations where culture is negative (5-12).
Three pneumococcal conjugated vaccines are registered in Egypt: PCV7, which is also licensed in more than 100 countries, including the United States; it has the serotypes (4,6B, 9V, 14, 18C, 19F, 23F). PCV10, which is also licensed in Canada and Europe but not in the United States; it includes the serotypes (1, 4, 5, 6B, 7F, 9V, 14, 18C, 19F, 23), and PCV13, which includes serotypes (1, 3, 4, 5, 6A, 6B, 7F, 9V, 14, 18C, 19A, 19F, 23F).
Antimicrobial resistance among S. pneumoniae isolates poses a special challenge for the treatment and control of pneumococcal infections, as there is an increase in the pattern of resistance over time. In Egypt, the penicillin resistance has changed over time. In 1993, 71% of the S. pneumoniae isolates were penicillin susceptible (13), decreasing to 63% in 2,000 and to 51% in 2004, when the drug of choice was ceftriaxone (4). Ceftriaxone susceptibility among S. pneumoniae isolates at this point in time was greater than 94% (4). The changes in susceptibility patterns over time suggest that the periodic monitoring of the patterns of antimicrobial resistance is necessary to guide effective treatment (14, 15).
2. Objectives
As the last study in Egypt to assess the serotypes’ distribution and antimicrobial susceptibility was conducted over 10 years ago, more recent data are needed to form a comprehensive and updated understanding of serotype distribution and antimicrobial susceptibility pattern in the region for effective preventive and treatment strategies. The goal of this study is to conduct a reassessment of the prevalent serotypes in Egypt as an essential step in the search for a regional vaccine. In addition, another goal is to monitor the antibiotic susceptibility patterns of pneumococcal strains currently causing infections to evaluate the strategies applied in therapy.
3. Materials and Methods
3.1. Statement of Ethical Approval
All experiments involving any samples taken from patients in this study were conducted in accordance with and approval of the ethical committee at Cairo University, Cairo, Egypt. In addition, all patients who contributed any samples (swabs or any other form), provided written informed consent; in cases of children, written consent from the guardian or parent was obtained.
3.2. Samples Collection
A total of 100 clinical specimens were collected, in the greater Cairo area in Egypt, from 2011 to 2013. Greater Cairo area is an area of area: 1,709 km2 and represents Cairo Governorate, Giza city, Shubra El-Kheima, 6th of October city and Obour city, with a total population estimated at 20,500,000. Pneumonia represented 47% of cases, sinusitis cases were 28%, meningitis were 16%, 7% of cases were otitis media and 2% were conjunctivitis. Both conventional and molecular identification methods were applied to confirm the identification of S. pneumoniae.
3.3. Conventional Identification
All tests for the identification of bacteria were done according to laboratory methods for the diagnosis of meningitis (16), including: microscopical examination, and tests for optochin sensitivity (reagent; ethylhydrocupreine hydrochloride, Oxoid, UK), and bile solubility (reagent; Sodium deoxycholate, SigmaAldrich, USA).
3.4. Molecular Identification of S. pneumoniae Using cpsA Gene Using PCR Assay
For all PCR reactions, DNA was extracted using EZ-10 spin column genomic DNA miniprep kit according to manufacturer’s protocol (BioBasic Inc., Canada). The cpsA gene was used as specific marker for the discrimination of S. pneumoniae from other streptococci (17). For PCR reaction, primers used were cpsA forward primer: 5’-GCAGTACAGCAGTTTGTTGGACTG ACC-3’ and cpsA reverse primer: 5’-GAATATTTTCATTATCAGTCCCAGTC-3’. Both primers would amplify the region corresponding to nucleotides 2,314 - 2,473. All PCR reagents and buffers were from Alliance Bio, USA. PCR thermal cycling was done at initial denaturation temperature of 94°C for four minutes, followed by 30 amplification cycles of denaturation at 94°C for 45s, annealing at 54°C for 45s and polymerization at 65°C for two minutes, 30 seconds, then final extension at 72°C for 10 minutes (12). DNA was extracted from the reference strain S. pneumonae ATCC 49619 under the exact same conditions and used as a positive control.
3.5. Antimicrobial Susceptibility of Streptococcus pneumoniae Isolates
The tested isolates were sub-cultured on blood-agar plates and incubated in 5 % CO2 at 37°C for 24 hours. Direct colony suspension was prepared equivalent to 0.5 McFarland and used on Muller Hinton agar; then, the antibiotic discs Oxoid, UK were applied aseptically. The plates were incubated at 37°C for 24 hand the diameters of inhibition zones were measured. Isolates were classified as susceptible, intermediate or resistant in accordance with the Clinical and Laboratory Standards Institute (18). A list of antibiotics used and their concentrations is in Table 1.
| Antibiotic of Different Class | Symbol | Disc Content, µg |
|---|---|---|
| Penicillin | ||
| Oxacillin | OXA | 1 |
| Amox/clavulanic | AMC | 20/10 |
| Glycopeptides | ||
| Vancomycin | VAN | 30 |
| Macrolides | ||
| Erythromycin | ERY | 15 |
| Azithromycin | AZM | 15 |
| Clarithromycin | CLR | 15 |
| Tetracycline | ||
| Tetracycline | TET | 30 |
| Quinolones | ||
| Ciprofloxacin | CIP | 5 |
| Levofloxacin | LVX | 5 |
| Ofloxacin | OFX | 5 |
| Norfloxacin | NOR | 10 |
| SulphonamidesandTrimethoprime | ||
| Sulphonamides and Trimethoprime | SXT | 23.75/ 1.25 |
| Amphenicols | ||
| Chloroamphenicol | CHL | 30 |
| Aminoglycosides | ||
| Tobramycin | TOB | 10 |
| Amikacin | AMK | 30 |
| Gentamicin | GEN | 10 |
| β-lactams/Cephalosporin, 2nd | ||
| Cefaclor | CEC | 30 |
| Cefurxim | CXM | 30 |
| β-lactams/Cephalosporin, 3rd | ||
| Ceftazidime | CAZ | 30 |
| β-lactams/Cephalosporin, 4th | ||
| Cefepime | FEP | 30 |
| Cefoperazon | CFM | 75 |
| Other β-lactams | ||
| Imepenem | IPM | 10 |
| Linezolid | ||
| Linezolid | LZM | 30 |
3.6. Serotyping of S. pneumonia Isolates Using PCR Assay:
Nine primer pairs were used to target serotypes 1, 5, 6A/B, 14, 16F, 19A, 19F, 20 and 23F (Table 2) (12). The primers target the following genes (serotypes are indicated in parentheses): cap1H (1), wxy (5), wcip (6), cps14H (14), cps19aK (19A), cps19fI (19F), and cps23fG (23F). All primers were synthesized at Sigma-Aldrich, USA. All samples confirmed to have cpsA gene were examined to be one of the serotypes listed. The same conditions used before with the cpsA gene in thermal cycling were applied here.
| Serotype | GenBank Accession Number | Primer Sequence (5’ to 3’) | Nucleotide Positions | Product Size, bp |
|---|---|---|---|---|
| 6A/B | AF316640 | 250 | ||
| F | AATTTGTATTTTATTCATGCCTATATCTGG | 8656 | ||
| R | TTAGCGGAGATAATTTAAAATGATGACTA | 8877 | ||
| 1 | Z83335 | 280 | ||
| F | CTCTATAGAATGGAGTATATAAACTATGGTTA | 10469 | ||
| R | CCAAAGAAAATACTAACATTATCACAATATTGGC | 10715 | ||
| 19A | AF094575 | 478 | ||
| F | GTTAGTCCTGTTTTAGATTTATTTGGTGATGT | 12118 | ||
| R | GAGCAGTCAATAAGATGAGACGATAGTTAG | 12566 | ||
| 23F | AF057294 | 384 | ||
| F | GTAACAGTTGCTGTAGAGGGAATTGGCTTTTC | 12118 | ||
| R | CACAACACCTAACACACGATGGCTATATGATTC | 12566 | ||
| 14 | 34359 | 208 | ||
| F | CTTGGCGCAGGTGTCAGAATTCCCTCTAC | 7968 | ||
| R | GCCAAAATACTGACAAAGCTAGAATATAGCC | 8145 | ||
| 19 | U09239 | 304 | ||
| F | GTTAAGATTGCTGATCGATTAATTGATATCC | 7828 | ||
| R | GTAATATGTCTTTAGGGCGTTTATGGCGATAG | 8100 | ||
| 16F | Nr.34361 | 988 | ||
| F | CTGTTCAGATAGGCCATTTACAGCTTTAAATC | 11521 | ||
| R | CATTCCTTTTGTATATAGTGCTAGTTCATCC | 12478 | ||
| 20 | 34365 | 514 | ||
| F | GAGCAAGAGTTTTTCACCTGACAGCGAGAAG | 9567 | ||
| R | CTAAATTCCTGTAATTTAGCTAAAACTCTTATC | 10048 | ||
| 5 | AY336008 | 362 | ||
| F | ATACCTACACAACTTCTGATTATGCCTTTGTG | 6123 | ||
| R | GCTCGATAAACATAATCAATATTTGAAAAAGTATG | 6450 |
3.7. Detection of Virulence Factors for the Identified Most Prevalent Serotypes
3.7.1. Detection of the pneumolysin (ply) Gene and the autolysin (lytA) Gene
PCR assay used to detect pneumolysin (ply) gene and the autolysin (lytA) gene was performed as previously described (19): primers used were ply forward outer primer, (5’-TTTCTGTAACAGCTACCAACGA-3’) and ply reverse outer primer (5’-GAATTCCCTGTCTTTTCAAAGTC-3’), both primers amplified a 348-bp region of the ply gene, (20, 21). For the (lytA) gene, forward primer (5’-ACGCAATCTAGCAGATGAAGC) and reverse primer (5’-TGTTTGGTTGGTTATTCGTGC), (22), were used to amplify a 101-bp fragment of the lytA gene. PCR thermal cycling was performed with initial denaturation temperature at 95°C for five minutes, followed by 35 amplification cycles of denaturation at 95°C for 45 seconds, annealing at 60°C for 45 s and polymerization at 72°C for 30 seconds and final extension at 72°C for eight minutes.
3.7.2. Detection of the pneumococcal surface antigen A (psaA) Gene
The gene encoding the pneumococcal surface adhesin A (PsaA) protein was confirmed in all S. pneumoniae serotypes (18). The sequences of the primers used to amplify psaA were as follows: 5’CTTTCTGCAATCATTCTTG3’ as the forward primer and 3’GCCTTCTTTACCTTGTTCTGC5’ as the reverse primer (23). PCR thermal cycling was at initial denaturation temperature of 94°C for 15 minutes, followed by 30 amplification cycles of denaturation at 94°C for 30 seconds, annealing at 52°C for 30 seconds and polymerization at 72°C for two minutes and final extension at 72°C for eight minutes (24).
4. Results
4.1. Samples Collection and Conventional Identification
A total of 100 clinical specimens were collected in the greater Cairo area of Egypt, from 2011 to 2013. The samples collected represent a fair distribution across Egypt as they were collected from the main Cairo metropolitan area. Isolates were cultured and identified as S. pneumoniae by both conventional and molecular methods. The whole collection of 100 isolates were identified morphologically as gram positive diplococci. Colonies of S. pneumoniae appeared on Blood agar plate as small, grey, moist characteristically produced a zone of alpha-hemolysis (green). Out of 100 isolates, 12 isolates were found to be optochin-resistant with inhibition zones (< 14 mm), while, only seven out of 100 isolates were bile-insoluble.
4.2. Molecular Identification of S. pneumoniae Using cpsA Gene
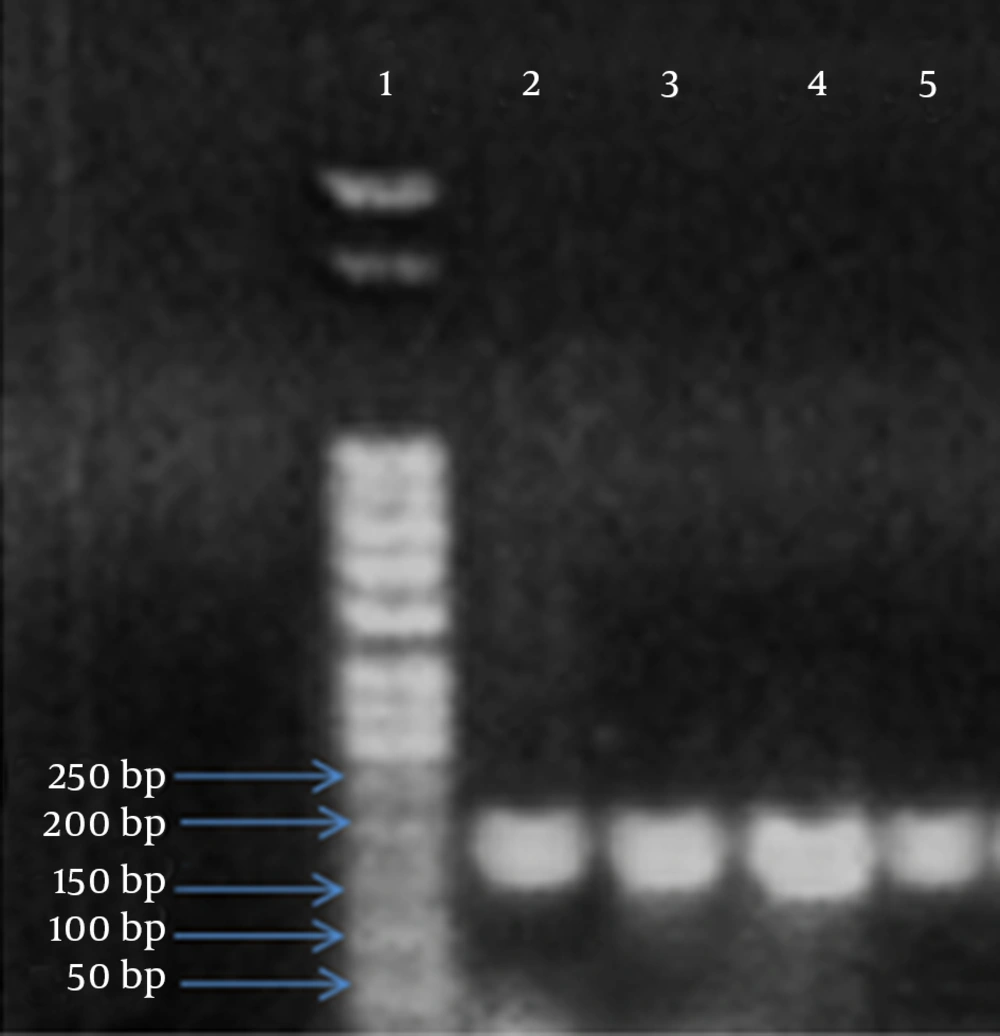
PCR assay for cpsA gene was used to identify all the 100 isolates. PCR assay revealed an amplified product in all tested samples including optochin-resistant and bile-insoluble isolates. The sizes of the amplicon obtained from the tested strains corresponded to the predicted size of 160 bp (Figure 1). A reference strain S. pneumoniae ATCC 49619 was used as a positive control.
4.3. Antimicrobial Susceptibility of S. pneumoniae Isolates
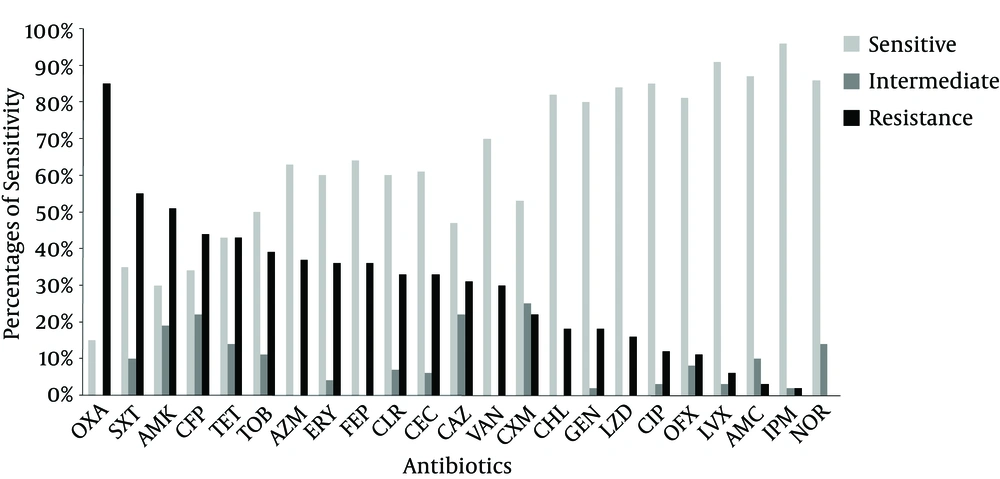
The 100 S. pneumoniae isolates were tested for their susceptibility to 13 antibiotics belonging to nine different classes (penicillin, glycopeptides, macrolides, tetracycline, quinolones, sulphonamides and trimethoprime, amphenicols, aminoglycosides and betalactams) by using disk diffusion method. The antibiotic resistance profiles of the isolates against the 13 antimicrobial agents are presented in Figure 2. The results revealed high resistance to different antibiotic classes, especially to penicillin (85%), tetracycline (55%) and sulphonamides and trimethoprime (43%), whereas, S. pneumoniae still have relatively high sensitivity for macrolides and quinolones (about 60% and 85% respectively).
OXA: oxacillin, SXT: trimethoprim-sulfamethoxazole, AMK: Amikacin, CFP: cefoperazone, TET: tetracycline, TOB; tobramycin, AZM: azithromycin, ERY: erythromycin, FEP: cefepime, CLR: clarithromycin, CEC: cefaclor, CAZ: ceftazidime, VAN: vancomycin, CXM: cefuroxime, CHL: chloramphenicol, GEN: gentamycin, LZD: linezolid, CIP: ciprofloxacin, OFX: ofloxacin, LVX: levofloxacin, AMC: amoxicillin-clavulanic acid, IPM: imipenem, NOR: norfloxacin.
4.4. Serotyping of S. Pneumoniae Clinical Isolates
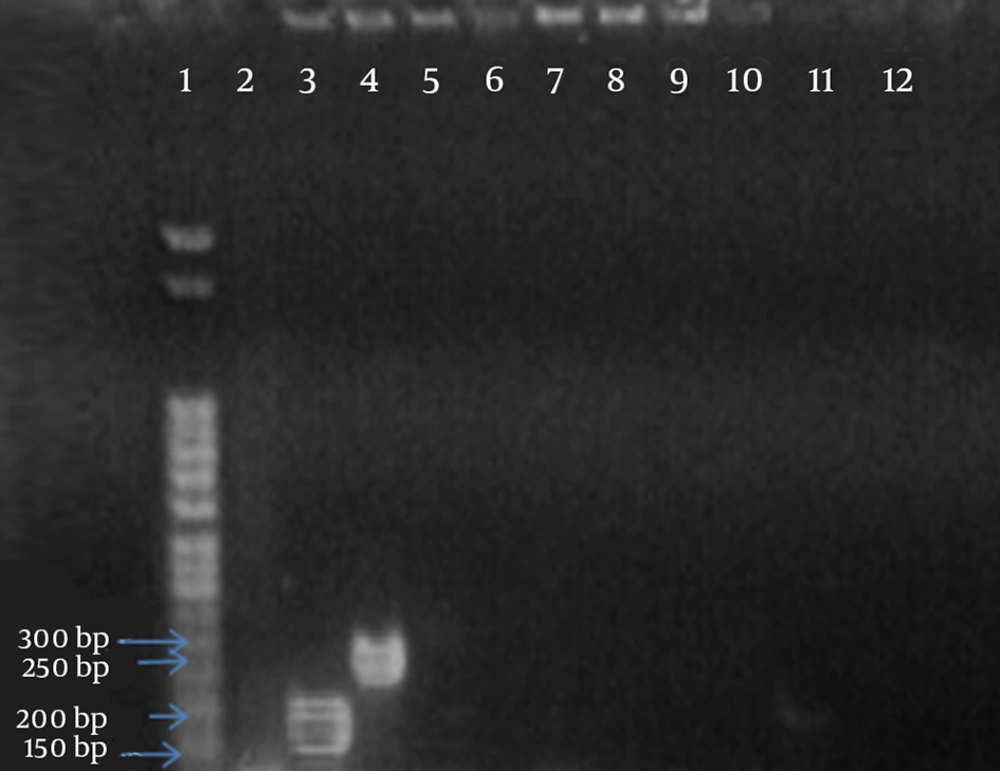
After the confirmation that each clinical isolate has capsular polysaccharide gene, another nine amplification reactions (one reaction for the identification of each serotype 1, 5, 6A/B, 14, 16F, 19A, 19F, 20 and 23F) was done to detect the specific serotype for each isolates. Isolates either were assigned to be one of the serotypes and/or serogroups tested or were designated to be “other serotype” if they failed to give a product with any of the nine serotypes primer pairs. The results of the prediction of pneumococcal serotypes revealed that the most common serotypes are 6A/B (30 %) followed by 19F (18 %). The complete distribution of the serotypes is summarized in Table 3. An example of serotyping with serotype 6A/B is shown in Figure 3.
| Serotype | Number of Isolates |
|---|---|
| 6 A/B | 30 |
| 19F | 28 |
| 5 | 15 |
| 23F | 7 |
| Other serotypes | 20 |
Lane 1, DNA marker; lane 3, represents the amplified products of cpsA gene (160-bp fragment); lane 4, represents the amplified product of serotype 6 A/B (250-bp fragment) and lanes 5 to 12 represent amplified products of serotypes 1, 5, 14, 16F, 19A, 20, 23F and 19F respectively (all negative).
4.5. Antimicrobial Susceptibility for Predominant Serotypes
The two predominant serotypes/groups (19F serotype and 6A/B group) exhibited high rates of resistance to penicillin (82% and 80%), macrolides (77% and 73%) and tetracycline (75% and 50%) respectively.
4.6. Detection of Virulence Factors for Predominant Serotypes
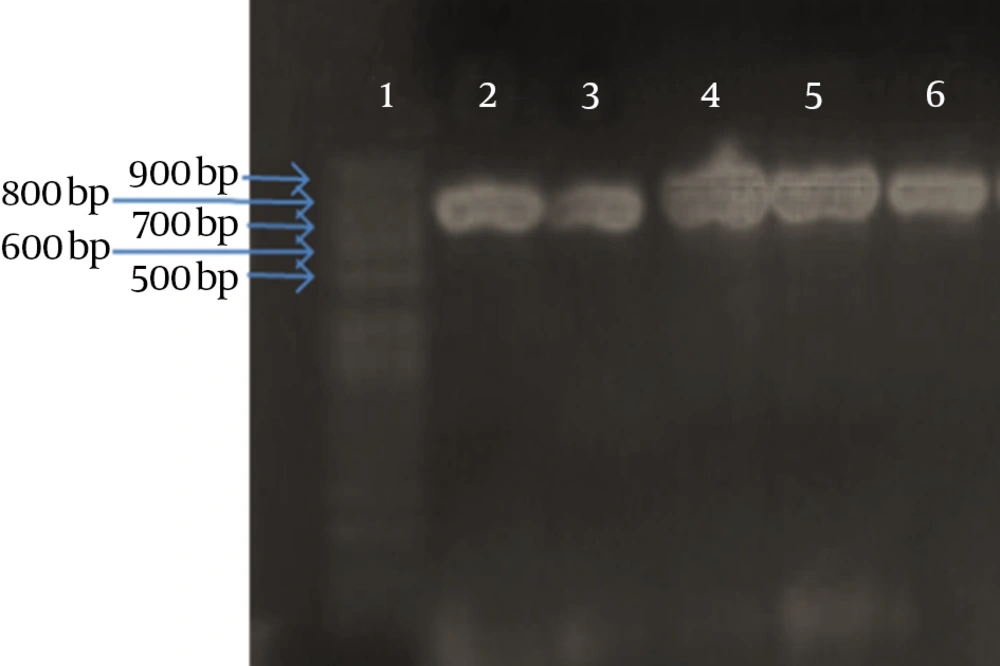
Detection of pneumolysin (ply) gene, autolysin (lytA) gene and the pneumococcal surface adhesin A (PsaA) protein in serotype 6A/B and serotype 19F using PCR assay revealed that, all the 58 isolates (100%) were positive for (lytA) and (psaA) genes, while only 44 out of 5 (75%) isolates were positive for (ply) gene, indicating that (lytA) and (psaA) genes are the most sensitive genes for detection of S. pneumoniae. An example is shown in Figure 4, showing the amplification product observed with psaA gene product with some isolates.
5. Discussion
In previous work investigating the spread of S. pneumoniae, clinical isolates were collected from CSF specimens of patients with meningitis, while few studies addressed pulmonary infection from S. pneumoniae. Here, we worked on serval isolates from different sources, such as nose, throat, CSF, sputum and ear; therefore, it represented a more widespread approach to investigate all types of diseases caused by S. pneumoniae with all aspects of clinical manifestations. In addition, in this study, molecular methods were used both for detection as well as serotyping as compared to prior studies done in Egypt, which all depended on traditional biochemical tests, latex agglutination and quelling reaction.
Due to the large geographic area of the Cairo metropolis, and due to the fact that many residents even in faraway regions all over Egypt do come to Cairo to seek treatment for severe diseases, we believe that our samples cover the distribution across the country.
Numerous studies discussed S. pneumoniae identification and confirmed optochin-resistance among S. pneumoniae isolates, making it difficult to depend on optochin-sensitivity test in S. pneumoniae identification (25-27). Several studies suggested that bile solubility test is more sensitive than the optochin sensitivity test (28); in agreement with these studies, we found that 12 out of 100 isolates showed optochin resistance and only 7 out of 100 isolates was found to be bile insoluble.
Molecular identification of S. pneumoniae using PCR assays has frequently targeted genes that encode pneumococcal virulence factors. These factors include autolysin (lytA) (22), pneumolysin (ply) (29), pneumococcal surface antigen A (psaA) (24). However, some pneumococcal virulence genes of S. pneumoniae have been detected in S. mitis or S. oralis isolates (19, 30, 31). Our study depends on the use of cpsA gene as a novel genomic marker specific for S. pneumoniae which is in agreement with the study done by Park et al. (17), all the clinical isolates were positively identified as S. pneumoniae, since they all showed the presence of this particular gene as the control reference standard strain used.
The antimicrobial susceptibility patterns were investigated using antibiotics belonging to various classes and the results indicated, in general, an increase in antibiotic resistance. Several previous studies reported penicillin resistant S. pneumonia starting from Year 1991 to Year 2005, the percentage of penicillin susceptible S. pneumoniae dropped between the periods of 1993 - 2004. Resistance to oxacillin was only 6% in a study conducted in 1998 to 2000, while in our study, an increase in oxacillin resistance was observed as it reached 85%. Chloramphenicol resistance was variable from 29.7 % in 1993, to 14% and 18 % in 2000, and then dropped to 9% in 2003, then back to an increase in our current study to reach 18%. Tetracycline resistance ranged between 52% and 62%, which were almost similar to our study (57%). The same results were observed with sulphonamides and trimethoprime, which remained almost unchanged from 60% to 65% in our study (4, 13, 15, 32). However, our work is showing promising susceptibility to new antibiotics such as imepenem, with sensitivity over 96%; norfloxacin, having an 85% sensitivity, and linezolid which revealed a sensitivity of 84%.
There is a variation in the prevalent serotype amongst previous different epidemiological studies in Egypt conducted at different time intervals (2, 3, 33, 34). The first study conducted in Egypt in the late 1970s used Quellung reaction, and identified type 1 as the most frequently observed capsular type (33). The epidemiological study by Wasfy et al. (2), between 1998 - 2003, reported that the major serotypes are (6B, 1, 19A, 23F, 6A) from CSF specimens of patients with meningitis. The other epidemiological study conducted by Afifi et al. (4), between 1998 - 2004, confirmed these finding about predominant serotypes in Egyptian patients. On the other hand, our study revealed that currently, serogroup 6 A/B and serotype 19F are the most predominant serotypes. Serotype A/B is the most prevalent with a percentage of 30%; serotype 19F represented 28% of clinical isolates and is now among the most prevalent serotypes of S. pneumoniae. Additionally, another new serotype (5) appeared to represent 15% of all investigated isolates, while the serotype 23F represented only 7%, indicating changes in distribution of serotypes.
Studying the virulence factors among the most prevalent serotypes (6A/B and 19F) revealed that autolysin and psaA were the most sensitive genes for identification of S. pneumonia as they were detected in all 6A/B and 19F isolates (the total 58 isolates, 100 %) while pneumolysin detection had less sensitivity in S. pneumoniae identification as it was only detected among 44 out of the 58 isolates, 75% of the same collection as previously shown in other studies (35, 36).
In conclusion, our study showed that the most prevalent S. pneumoniae serotypes in Egypt were found to be 6A/B and 19F. Our collection of isolates was isolated from different specimens representing different diseases caused by S. pneumoniae. Most isolates exhibited high rates of resistance to various classes of antibiotics. Molecular typing can be used to identify and confirm the different predominant serotypes of S. pneumoniae. Both the virulence factors autolysin (lytA) and pneumococcal surface antigen A (psaA) genes are more sensitive than pneumolysin (ply) gene for S. pneumoniae identification. This work demonstrates the importance of constantly monitoring the prevalent serotypes in any region to modulate the components of the used vaccines. This will aid in the development of more effective vaccines that would help elevate the burden of such disease around the world.