1. Background
Gastric colonization with Helicobacter pylori (HP) causes peptic ulcer (PU) in about 10% - 15.0%, gastric adenocarcinoma in about 1% - 30%, and gastric mucosa-associated lymphoid tissue (MALT) lymphoma in less than 1% of cases (1, 2). Helicobacter pylori-linked virulence elements, the host’s genetic and immunological parameters, and environmental parameters execute critical roles in the development of HP-induced gastrointestinal diseases (3, 4). The cytotoxin-associated gene A (cagA) is known as the strongest virulence agent of HP, and CagA+ bacteria lead to more serious consequences such as PU and malignancy (5, 6). Diverse kinds of immune cells, including neutrophils, eosinophils, dendritic cells (DCs), natural killer cells, and T and B lymphocytes accumulate into the gastric mucosa during HP infection (7, 8).
Chemokines guide leukocytes towards infection and inflammation sites and are categorized into four major subgroups, including CXC-, CC-, XC-, and CX3C, based on their conserved cysteine residues near the N-terminus (9, 10). Accordingly, their corresponding chemokine receptors are named CXCR, CCR, XCR, and CX3CR, respectively (9, 10). Among leukocytes, effector T lymphocytes play a decisive role in the development of HP-related gastrointestinal disorders (2). T helper 1 (Th1)-released cytokines, especially IFN-γ, reinforce the bactericidal capacity of macrophages and proper Th1 cell activation, leading to HP elimination by activated macrophages (2, 11). However, uncontrolled Th1 responses may lead to pathologic outcomes such as PU (2). The CXCL10 chemokine plays a vital role in the migration of Th1 cells since its receptor (CXCR3) is preferentially expressed on these cells (12, 13). On the other hand, Th2-released cytokines mediate antibody production by inducing B cells (11). The protective function of antibodies during HP infection is doubtful; however, there are pieces of evidence indicating that mucosal antibodies, especially IgA, may provide protection via reducing HP colonization (2, 11). Pathogen-specific regulatory T cells (Treg) limit the development of immunopathological consequences through secreting immune repressor cytokines; IL-10, IL-35, and TGF-β (14). However, extreme Th2- and Treg-linked responses may lead to HP-related malignancies (2). The CCL17 and CCL22 chemokines also play important roles in the migration of Th2 and Treg cells because CCR4, as their receptor, is preferably expressed on these cells (15, 16). Th17 cells secrete various kinds of cytokines, especially IL-17A and IL-17F, involved in the recruitment of neutrophils through inducing the release of neutrophil-attracting chemokine, CXCL8, from epithelial cells (17). Th17 cells also play a prominent role in attracting neutrophils into the gastric mucosa during HP infection. However, neutrophils are not able to effectively destroy HP, and their accumulation causes tissue injuries and complications such as gastritis (18, 19). CCL20 is a Th17-related chemokine, and Th17 cells express CCR6, the receptor of CCL20 (20).
Ginger (a plant belonging to the Zingiberaceae family) has been consumed in traditional medicine for a long period of time (21). Some beneficial effects, especially anti-inflammatory, antibacterial, anti-oxidant, anti-hyperlipidemia, and anti-tumorigenic functions, have been declared for ginger and its constituents (14). Ginger and its derivatives have displayed beneficial effects in some human inflammatory illnesses such as rheumatoid arthritis, colitis, osteoarthritis, and type 2 diabetes (14), as well as in experimental animal models of PU (22), allergic asthma (23), neuroinflammation (24), and ulcerative colitis (25).
The protective effects of ginger have been demonstrated in some gastrointestinal disorders such as PU, functional dyspepsia, gastritis, indigestion, bloating, and epigastric discomfort (26-28). Ginger also has potent free radical scavenging activity and anti-oxidant lipid anti-peroxidation properties, which all may also promote gastro-protective functions (26). Furthermore, the direct anti-HP activities of ginger (especially on CagA+ strains) have been indicated in some studies (29, 30).
Since gastrointestinal microbiota can interact with each other, they may affect the host’s response to H. pylori infection by changing the gastric microbiome and transferring genes to each other (31). Physiologically, the stomach is a sterile environment, as evidenced by microbial culture methods, but recently it has been observed that microbiome exists in the stomach of healthy people with a frequency of 102 - 104 CFU/g, and the most prevalent bacteria in the stomach belong to the Prevotella and Streptococci species. However, the stomach microbiome may change during chronic H. pylori infection (31, 32). Ginger may affect the stomach microbiome directly via its antibacterial effects or indirectly through inhibitory effects on other bacteria such as H. pylori, Citrobacter spp., Shigella spp., Salmonella, and E. coli (31). Accordingly, ginger may exert beneficial effects on stomach microbiome. The antibacterial effects of ginger derivatives such as [6]‐dehydrogingerdione, [10]‐gingerol, [6]‐gingerol, and [6]‐shogaol against clinical drug‐resistant Acinetobacter baumannii have also been shown (32). The antibacterial effects of ginger extract (GE) on a variety of Gram-negative and Gram-positive bacteria such as E. coli, Proteus spp., Pseudomonas aeruginosa, Staphylococcus aureus, and Bacillus spp. have also been reported (33).
Inappropriate T cell-related responses and the improper production of Th1-, Th2-, Th17-, and Treg-related chemokines play a fundamental role in the development of HP-related gastrointestinal complications such as PU (2, 33).
2. Objectives
Accordingly, the modulation of the chemokines or their receptors may have therapeutic values. Therefore, our aim was to assess the impacts of GE on the expression of CCL17, CCL20, CCL22, and CXCL10 chemokines and their relevant receptors (CCR4, CCR6, and CXCR3) in the HPCE-induced PBMCs derived from HP-infected patients with PU. Also, HP-infected asymptomatic subjects (HAS) and non-infected healthy subjects (NHS) were enrolled as control groups.
3. Methods
3.1. Preparation of Hydroalcoholic GE
The optimal condition for extracting the functional compounds of ginger, such 6-gingerol, and 6-shogaol, is to use 70% ethanol at 62.29°C - 70°C for 52 - 70 min (34). Thus, 20 g of the dried powder of ginger rhizomes was obtained from the Isfahan Agricultural and Natural Resources Research Center (Isfahan, Iran). The 70% ethanolic GE was obtained from the plant powder (5 g) using the Soxhlet method, which was dissolved in 100 mL ethanol at 70°C (35-37). The GE obtained by the Soxhlet method has more activity compared with other methods such the maceration and ultrasonic methods (37, 38). Ginger extract was dissolved in the DMEM High (Shellmax; China) medium and stored at -20°C.
3.2. Preparation of H. pylori-Derived Crude Extract
Five strains of HP bearing CagA, VacA, UreA-B, and flagella virulence factors were prepared from the Pasteur Institute (Tehran, Iran). For disrupting the bacteria, HP colonies were suspended in sterilized-distilled water and sonicated for five minutes on ice. Bacterial debris and intact cells were removed using centrifugation at 8000 g for 10 minutes at 4°C. After determining protein concentration by measuring OD at 280 nm using a spectrophotometer, the supernatant was sorted and kept at -70°C (39).
3.3. Subjects
Based on a previous study (39) and using the sample size formula of
3.4. Measurement of H. pylori-Specific Immunoglobulins
For this purpose, ELISA kits were used to detect plasma HP-specific IgG and IgA (Ideal-Tashkhis, Iran), according to the manufacturer’s instructions.
3.5. Preparation of and Culturing PBMCs
Based on a previous study, PBMC isolation was conducted using the Ficoll gradient method, which yields the greatest quantity of RNA compared with other techniques such as magnetic separation and CPT tubes (42). PBMCs were isolated from heparinized peripheral blood using a density-gradient centrifugation on Ficoll (Biowest, France) (42). In brief, diluted blood specimens were transferred to Ficoll and centrifuged for 20 minutes at 2000 rpm. The PBMCs were gently removed from Ficoll and washed twice with PBS before being suspended in the DMEM high (Shellmax; China) medium. The viability of PBMCs was determined by trypan blue staining, and when viability was greater than 95%, the cells were cultured for further analysis.
The PBMCs collected from PU, HAS, and NHS individuals were cultured in 24-well plates at the 2 × 106 cells/ml density in the DMEM high medium supplemented with heat‐inactivated FBS (Shellmax; China, 10% V/V), 0.1 mg/mL streptomycin, and 100 U/mL penicillin (Shellmax; China). The PBMCs separated from each participant were cultured in five wells as follows: one well was considered the negative control (without stimulation or GE treatment), and the cells in wells two to five were stimulated with HPCE (10 µg/well) at the presence of either 0, 10, 20, or 30 µg/well of GE, respectively. The doses of GE were chosen according to previous studies (43-45). The plates were incubated at 37°C for 36 hours in a humidified condition with 5% CO2. After this period, supernatants were collected and stored at -70°C for measuring chemokines. Total RNA was also extracted from PBMCs for assessing the gene expression of chemokine receptors.
3.6. RNA Extraction and Gene Expression of Chemokine Receptors
Total RNA was isolated from cultured PBMCs using a commercial kit (ParsTous, Iran) according to the manufacturer’s instructions. The quality of RNA was determined by electrophoresis on 1.5% agarose gel. A spectrophotometer (NanoDrop DNovix, USA) was used to determine the quantity and purity of the extracted RNA based on absorption at 280 and 260 nm.
RNA conversion to complementary DNA (cDNA) was performed using a commercial cDNA synthesis kit (Pars-Tous, Iran) according to the manufacturer’s instructions. The reverse transcription schedule included an initial 65°C for 5 min (in the absence of the reverse transcriptase enzyme). After adding the reverse transcriptase enzyme, incubation continued at 20°C for 1 min (the cooling stage) and 47°C for 60 min. Eventually, the reaction was halted by incubation at 70°C for 10 min to inactivate the reverse transcriptase enzyme.
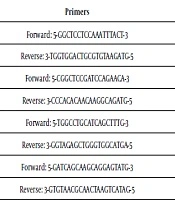
A real-time PCR system (Applied-Biosystems, USA) was used to assess the gene expression of the chemokine receptors of CXCR3, CCR4, and CCR6. The real time-PCR reaction mixture was prepared using a SYBR green master mix (Takara Clontech; Japan) and applying 1 µL of the synthesized cDNA with proper primers (Table 1). Thermal cycling steps entailed 95°C for 15 min and 40 cycles of 60°C for 30 s, 72°C for 40 s, and 95°C for 1 min. The amplified chemokine receptors’ genes were normalized using β-actin as an internal control. The gene expressions of CCR4, CCR6, and CXCR3 in the isolated PBMCs were adjusted according to β-actin gene expression and calculated by the 2-ΔΔCt formula.
| Genes | Primers | Product Size, bp |
|---|---|---|
| CCR4 | Forward: 5-GGCTCCTCCAAATTTACT-3 | 57 |
| Reverse: 3-TGGTGGACTGCGTGTAAGATG-5 | ||
| CCR6 | Forward: 5-CGGCTCCGATCCAGAACA-3 | 55 |
| Reverse: 3-CCCACACAACAAGGCAGATG-5 | ||
| CXCR3 | Forward: 5-TGGCCTGCATCAGCTTTG-3 | 57 |
| Reverse: 3-GGTAGAGCTGGGTGGCATGA-5 | ||
| β-Actin | Forward: 5-GATCAGCAAGCAGGAGTATG-3 | 88 |
| Reverse: 3-GTGTAACGCAACTAAGTCATAG-5 |
3.7. Chemokines’ Levels in PBMC Supernatants
Specific ELISA kits [CCL17, CCL20, and CXCL10 (Bio-Legend, USA), and CCL22 (R & D, USA)] were used to measure the chemokines’ concentrations in PBMC supernatants. The quantities of the chemokines were determined using standard samples with known levels and displayed as Pg/mL.
3.8. Statistical Analysis
Quantitative demographic data was reported as mean ± standard deviation (SD). The levels of CCL17, CCL20, CCL22, and CXCL10 chemokines and the gene expression of their receptors (CCR4, CCR6, and CXCR3) were reported as mean by the General Linear model, Repeated Measures ANOVA. In order to control type I error in hypothesis testing, Bonferroni correction was applied, which revealed the P-value of ≤ 0.005 should be considered significant. Statistical analyses were performed using SPSS statistical software (SPSS, version 20, USA).
4. Results
4.1. Participants’ Demographic Properties
The means of age were 51.80 ± 8.203 years in the PU group, 43.40 ± 13.33 years in HAS individuals, and 41.40 ± 7.021 years in the NHS group (P = 0.109). The ratio of men/women was 12/8 in all the three groups.
4.2. The Effects of GE on Chemokine Production and Chemokine Receptor Gene Expression in PU Patients’ PBMCs
The effects of GE on the production of CXCL10, CCL17, CCL20, and CCL22 by the PBMCs derived from PU patients were indicated in Table 2. In the PU group, the synthesis of CCL17, CCL20, and CCL22 by HPCE-stimulated PBMCs was remarkably greater than unstimulated control cultures (all with P ≤ 0.003). The HPCE-stimulated PBMCs treated with 10, 20, and 30 µg/mL of GE produced significantly lower CXCL10 (all with P < 0.001) and CCL20 (all with P ≤ 0.003) levels compared with untreated HPCE-stimulated PBMCs. The HPCE-stimulated PBMCs treated with 30 µg/mL of GE produced significantly higher CCL17 and CCL22 quantities than untreated HPCE-stimulated PBMCs (all with P < 0.001). Further, CCL22 production by 30 µg/mL GE-treated PBMCs was significantly higher than that of the PBMCs treated with 10 and 20 µg/mL of GE (all with P ≤ 0.001). The production of CXCL10 by the HPCE-stimulated PBMCs treated with 10, 20, and 30 µg/mL GE was significantly lower compared with unstimulated control culture (all with P < 0.001). The production of CCL17 and CCL22 by the HPCE-stimulated PBMCs treated with 10 and 30 µg/mL GE was significantly higher than that of unstimulated control culture (all with P ≤ 0.002). Also, CCL17 production by the HPCE-stimulated PBMCs treated with 20 µg/mL GE was significantly higher compared with unstimulated control culture (P < 0.001).
| Chemokines/ Chemokine Receptors | Groups | PBMC Cultures | P-Values (Intra-Groups) | P-Values (Inter-Groups) | ||||
|---|---|---|---|---|---|---|---|---|
| Control | HPCE | Ginger Extract-Treated (10 µg/mL) | Ginger Extract-Treated (20 µg/mL) | Ginger Extract-Treated (30 µg/mL) | ||||
| CXCL10, Pg/mL | PU | 4550.00 ± 50.00 | 4907.42 ± 118.48 | 3334.74 ± 211.23 | 3262.93 ± 213.48 | 3206.17 ± 75.95 | NSA; P < 0.001B, C, D, E, F, G; NSH, I, J | NSK; 0.002L, M; 0.025N; NSO |
| HAS | 4841.96 ± 86.95 | 5251.17 ± 55.95 | 4509.60 ± 118.93 | 4005.33 ± 78.05 | 3946.78 ± 263.87 | P = 0.005A; NSB; P < 0.001C; P = 0.004D; P < 0.001E, F; P = 0.003G; P < 0.001H, I, J | ||
| NHS | 4485.60 ± 355.01 | 4802.71 ± 52.23 | 4144.69 ± 276.77 | 4021.51 ± 283.52 | 3430.98 ± 250.94 | NSA, B, C, D, E, F; P < 0.001G; NSH, I, J | ||
| CCL17, Pg/mL | PU | 2250.64 ± 65.70 | 2910.42 ± 106.57 | 3450.95 ± 245.10 | 3514.91 ± 169.76 | 3716.91 ± 49.87 | P < 0.001A; P = 0.002B; P < 0.001C, D; NSE, F; P < 0.001G; NSH, I, J | P ≤ 0.001K, L, M, N, O |
| HAS | 1768.74 ± 32.77 | 2016.33 ± 125.50 | 2499.85 ± 278.04 | 2608.69 ± 183.35 | 2697.16 ± 100.51 | NSA, B; P = 0.002C; P < 0.001D; NSE, F; P = 0.005G; NSH, I, J | ||
| NHS | 1524.94 ± 142.07 | 1746.39 ± 87.18 | 2107.29 ± 85.16 | 2217.09 ± 98.88 | 2275.97 ± 161.12 | NSA, B, C, D; P = 0.005E; P = 0.002F; NSG; P < 0.001H; NSI, J | ||
| CCL20, Pg/mL | PU | 894.63 ± 76.53 | 1257.21 ± 25.67 | 872.38 ± 74.88 | 775.01 ± 99.68 | 760.23 ± 111.56 | P = 0.003A; NSB, C, D; P = 0.001E; P = 0.002F; P = 0.003G; NSH, I, J | P < 0.001K, L, M; P = 0.004N; P = 0.009O |
| HAS | 458.74 ± 7.05 | 544.30 ± 11.17 | 528.57 ± 8.41 | 507.75 ± 13.47 | 477.62 ± 7.59 | P < 0.001A, B; NSC, D, E; P = 0.003F, G, H; NSI, J | ||
| NHS | 512.19 ± 21.00 | 823.39 ± 29.63 | 502.24 ± 28.99 | 491.24 ± 32.74 | 470.44 ± 45.28 | P < 0.001A; NSB, C, D; P < 0.001E, F, G; NSH, I, J | ||
| CCL22, Pg/mL | PU | 141.11 ± 13.21 | 223.09 ± 7.37 | 245.83 ± 22.79 | 250.52 ± 32.92 | 355.20 ± 15.52 | P = 0.003A; P = 0.002B; NSC; P < 0.001D; NSE, F, P < 0.001G; NSH; P ≤ 0.001I, J | P < 0.001K, L, M, N, O |
| HAS | 88.62 ± 10.04 | 119.18 ± 12.36 | 134.35 ± 10.92 | 144.32 ± 10.42 | 167.41 ± 10.77 | P < 0.001A, B, C, D; P = 0.002E; P ≤ 0.001F, G; NSH; P < 0.001I , J | ||
| NHS | 290.60 ± 12.62 | 311.97 ± 23.12 | 386.30 ± 14.03 | 423.90 ± 24.98 | 464.62 ± 19.76 | NSA; P < 0.001B, C, D, E, F, G; NSH; P < 0.001I, J | ||
| CXCR3 gene expression (ratio) | PU | 0.782 ± 0.130 | 1.225 ± 0.058 | 0.643 ± 0.059 | 0.410 ± 0.060 | 0.348 ± 0.040 | NSA, B; P = 0.005C; P = 0.002D; P ≤ 0.001E, F, G; NSH; P = 0.002I; NSJ | All comparisons were NS |
| HAS | 0.750 ± 0.073 | 1.200 ± 0.035 | 0.832 ± 0.109 | 0.558 ± 0.098 | 0.328 ± 0.043 | P < 0.001A; NSB; P = 0.003C; P = 0.001D; NSE; P < 0.001F, G; NSH; P = 0.002I; NSJ | ||
| NHS | 1.002 ± 0.126 | 1.278 ± 0.024 | 1.004 ± 0.106 | 0.668 ± 0.120 | 0.324 ± 0.015 | NSA, B, C; P < 0.001D; NSE; P ≤0.001F, G; P = 0.005H; P = 0.002I; NSJ | ||
| CCR4 gene expression (ratio) | PU | 0.781 ± 0.082 | 0.850 ± 0.051 | 1.412 ± 0.154 | 1.434 ± 0.149 | 1.116 ± 0.123 | NSA; P = 0.005B; NSC, D; P = 0.003E; NSF, G, H, I, J | All comparisons were NS |
| HAS | 0.802 ± 0.049 | 0.906 ± 0.019 | 1.310 ± 0.108 | 1.428 ± 0.165 | 1.261 ± 0.117 | NSA, B, C; P = 0.001D; NSE, F, G, H, I, J | ||
| NHS | 0.998 ± 0.109 | 1.108 ± 0.159 | 1.190 ± 0.110 | 1.202 ± 0.184 | 1.400 ± 0.139 | All comparisons were NS | ||
| CCR6 gene expression (ratio) | PU | 0.759 ± 0.152 | 1.400 ± 0.021 | 0.600 ± 0.104 | 0.510 ± 0.067 | 0.492 ± 0.069 | P = 0.002A; NSB, C, D; P = 0.002E; P < 0.001F, G; NSH, I, J | NSK; P < 0.001L; NSM,N; P < 0.001 O |
| HAS | 0.678 ± 0.025 | 1.150 ± 0.033 | 0.608 ± 0.082 | 0.560 ± 0.102 | 0.208 ± 0.015 | P < 0.001 A; NSB, C; P < 0.001D, E, F, G; NSH; P = 0.001I; NSJ | ||
| NHS | 1.00 ± 0.13 | 1.49 ± 0.08 | 0.84 ± 0.09 | 0.74 ± 0.05 | 0.26 ± 0.02 | P = 0.004A; NSB,C; P ≤ 0.001D, E, F, G; NSH; P = 0.001I, J | ||
Abbreviations: HAS, H. pylori-infected asymptomatic subjects; NHS, non-infected healthy subjects, NS, not significant; PU, H. pylori -infected patients with peptic ulcer.
aThe superscripts of A, B, C, D, E, F, G, H, I, and J indicate the differences between, control and HPCE A; control and ginger 10 µg/mL B; control and ginger 20 µg/mL C; control and ginger 30 µg/mL D; HPCE and ginger 10 µg/mL E; HPCE and ginger 20 µg/mL F; HPCE and ginger 30 µg/mL G; ginger 10 µg/mL and ginger 20 µg/mL H; ginger 10 µg/mL and ginger 30 µg/mL I; and ginger 20 µg/mL and ginger 30 µg/mL J. The superscripts of K, L, M, N, O indicate the differences in the gene expression of a row-specified marker between PBMC cultures of control K; stimulated by HPCE L; treated with 10 µg/mL ginger extract M; treated with 20 µg/mL ginger extract N; and treated with 30 µg/mL ginger extract O in the PU, HAS, and NHSgroups, respectively.
The effects of GE on the gene expressions of CCR4, CCR6, and CXCR3 in the PBMCs derived from PU patients have been indicated in Table 2. The expression of CCR6 by HPCE-induced PBMCs was remarkably greater than that of unstimulated control culture (P = 0.002). The HPCE-stimulated PBMCs treated with 10, 20, and 30 µg/mL GE expressed significantly lower CXCR3 and CCR6 (all with P ≤ 0.002) compared with untreated HPCE-stimulated PBMCs. However, the HPCE-stimulated PBMCs treated with 10 µg/mL of GE expressed significantly higher amounts of CCR4 compared with untreated HPCE-stimulated PBMCs (P = 0.003). Also, CXCR3 expression was significantly lower in 30 µg/mL GE-treated PBMCs than in the cells exposed to 10 µg/mL GE (P = 0.002). Likewise, CXCR3 expression by the HPCE-stimulated PBMCs treated with 20 and 30 µg/mL doses of GE was significantly lower compared with unstimulated control culture (all with P ≤ 0.005). Finally, CCR4 was significantly upregulated in the HPCE-stimulated PBMCs treated with 10 µg/mL GE compared with unstimulated control culture (P = 0.005).
4.3. Ginger Extract Effects on Chemokine Production and Chemokine Receptor Gene Expression in PBMCs from the HAS Group
Table 2 exhibits GE effects on the production of CXCL10, CCL17, CCL20, and CCL22 by the PBMCs obtained from HAS subjects. In this group, the production of CXCL10, CCL20, and CCL22 was remarkably greater in HPCE-induced PBMCs than in unstimulated control culture (all with P ≤ 0.005). Also, the HPCE-stimulated PBMCs treated with 20 µg/mL and 30 µg/mL doses of GE produced significantly lower levels of CXCL10 and CCL20 (all with P ≤ 0.003), and those exposed to 10 µg/mL GE showed significantly lower CXCL10 (P < 0.001) compared with untreated HPCE-stimulated PBMCs. In the HAS group, the HPCE-stimulated PBMCs treated with 30 µg/mL GE produced significantly higher CCL17 and CCL22 concentrations than untreated HPCE-stimulated PBMCs (all with P ≤ 0.005). Also, the HPCE-stimulated PBMCs treated with 10 and 20 µg/mL doses of GE produced significantly higher CCL22 compared with untreated HPCE-stimulated PBMCs (all with P ≤ 0.002). The level of CCL22 was significantly higher in the PBMCs treated with 30 µg/mL GE than in the cells treated with 10 µg/mL and 20 µg/mL GE (all with P < 0.001).
The production of CXCL10 by the HPCE-stimulated PBMCs treated with 20 and 30 µg/mL GE was significantly lower than unstimulated control cells (all with P ≤ 0.004), and the production of CCL20 by the HPCE-stimulated PBMCs treated with 10 µg/mL GE was significantly higher than unstimulated control cells (P < 0.001). The HPCE-stimulated PBMCs exposed to 20 and 30 µg/mL doses of GE showed significantly higher levels of CCL17 and CCL22 than unstimulated control cells (all with P ≤ 0.002). Finally, CCL22 level in the HPCE-stimulated PBMCs treated with 10 µg/mL GE was significantly higher than unstimulated control cells (P < 0.001).
Table 2 exhibits the effects of GE on the gene expressions of CXCR3, CCR4, and CCR6 by the PBMCs derived from HAS subjects. The HPCE-induced PBMCs showed remarkably greater gene expressions of CXCR3 and CCR6 than unstimulated control cells (all with P < 0.001). The HPCE-stimulated PBMCs expressed significantly lower levels of CXCR3 (all with P < 0.001) when they were treated with 20 and 30 µg/mL GE and a lower expression of CCR6 after exposition to 10, 20, and 30 µg/mL GE (all with P < 0.001) compared with untreated HPCE-stimulated PBMCs. The expression of CXCR3 and CCR6 in 30 µg/mL GE-treated cells was remarkably lower than in the PBMCs treated with 10 µg/mL GE (all with P ≤ 0.002) and unstimulated control cells (all with P ≤ 0.001). Also, CXCR3 expression in the HPCE-stimulated PBMCs treated 20 µg/mL GE was significantly lower compared with unstimulated control cultures (P = 0.003). Finally, CCR4 expression in the HPCE-stimulated PBMCs treated with 30 µg/mL GE was significantly higher than in unstimulated control cells (P = 0.001).
4.4. The Effects of GE on Chemokine Production and Chemokine Receptor Gene Expression in the PBMCs Derived from the NHS Group
Table 2 displays the effects of GE on CXCL10, CCL17, CCL20, and CCL22 production in the PBMCs derived from NHS subjects. The level of CCL20 in the HPCE-induced PBMCs was remarkably higher than in unstimulated control cultures (P < 0.001). Significantly lower levels of CXCL10 (P < 0.001) in the HPCE-stimulated PBMCs treated with 30 µg/mL GE and CCL20 in the HPCE-stimulated PBMCs treated with 10, 20, and 30 µg/mL GE (all with P < 0.001) were observed compared with untreated HPCE-stimulated PBMCs. On the other hand, the HPCE-stimulated PBMCs treated with 10 and 20 µg/mL GE produced significantly higher CCL17 (all with P ≤ 0.005), and the HPCE-stimulated PBMCs treated with 10, 20, and 30 µg/mL GE produced significantly higher levels of CCL22 (all with P < 0.001) than untreated HPCE-stimulated PBMCs. Further, CCL22 production was significantly higher in 30 µg/mL GE-treated cells than in the PBMCs treated with 10 and 20 µg/mL GE (all with P < 0.001), and CCL17 production was significantly higher in 20 µg/mL GE-treated cells than in the PBMCs treated with 10 µg/mL GE (P < 0.001). In comparison with unstimulated control cells, the HPCE-stimulated PBMCs treated with 10, 20, and 30 µg/mL GE showed significantly higher levels of CCL22 (all with P < 0.001).
Table 2 exhibits the effects of GE on the gene expressions of CXCR3, CCR4, and CCR6 in the PBMCs extracted from NHS subjects. In this group, CCR6 was significantly upregulated in HPCE-induced PBMCs compared with unstimulated control cells (P = 0.004). Treating HPCE-stimulated PBMCs with 20 and 30 µg/mL doses of GE significantly downregulated CXCR3 while exposition to all 10, 20, and 30 µg/mL GE significantly suppressed the expression of CCR6 compared with untreated HPCE-stimulated PBMCs (all with P ≤ 0.001). However, treating HPCE-stimulated PBMCs with different doses of GE had no significant effects on CCR4 expression. Furthermore, CXCR3 and CCR6 gene expressions were significantly lower in the PBMCs treated with 30 µg/mL GE than in the cells exposed to 10 and 20 µg/mL GE (all with P ≤ 0.005). At last, CXCR3 and CCR6 gene expressions in the HPCE-stimulated PBMCs treated 30 µg/mL GE were significantly lower compared with unstimulated control cultures (all with P < 0.001).
5. Discussion
Chemokines play a critical role in the migration of particular types of immune cells towards inflammation and infection sites, affecting the nature of immune responses and the outcomes of acute inflammation (i.e., either termination or progression to chronic inflammation) and the infection (i.e., either deletion, persistence, or the occurrence of immunopathologic reactions) (46).
As a ligand for CXCR3, CXCL10 mainly triggers the migration of Th1 cells to the gastric mucosa and therefore plays a major role during HP infection (47, 48). During inflammatory immune responses, CXCL10 chemokine is secreted from keratinocytes, neutrophils, monocytes, eosinophils, as well as endothelial and epithelial cells in response to IFN-γ, recruiting Th1 cells (49) and triggering cell-mediated immunity against the bacteria and then HP elimination via activating macrophages. Increased CXCL10 expression was observed in HP-infected human gastric mucosa (50, 51), and elevated CXCR3 expression was also detected in murine and human stomach mucosa infected with HP (50-52). The abnormal expression of CXCL10 and its receptor, CXCR3, may contribute to the development of HP-linked PU and gastric cancer (46). The overproduction of CXCL10 recruits a large number of Th1 cells to the gastric mucosa, causing immunopathologic tissue damages such as PU and gastritis (48, 53). Our results indicated that in the HAS group, CXCL10 production by HPCE-stimulated PBMCs was significantly higher than by non-stimulated PBMCs, suggesting that adequate CXCL10 production might limit HP infection rendering the asymptomatic phenotype. However, CXCL10 production was not significantly different between non-stimulated and HPCE-stimulated PBMCs in the PU group. The reasons for these observations remain to be revealed in future investigations. It seems that insufficient CXCL10 production in some stages of HP infection may lead to the induction of a poor Th1 immune response against the bacteria, which in turn leads to HP persistence and HP-induced tissue damage. Our results also indicated that CXCL10 production in GE-treated cells (especially at the dose of 30 µg/mL) was significantly lower compared with HPCE-stimulated PBMCs in the NHS, HAS, and PU groups, suggesting the modulatory effects of ginger on CXCL10 production. Ginger may also directly inhibit CXCL10 secretion from epithelial cells, keratinocytes, endothelial cells, neutrophils, eosinophils, and monocytes (49) or indirectly suppress the inflammatory mediators of IL-12, IL-18, TNF-α, and IFN-γ, which act as CXCL10 inducers (54).
According to the results of the present study, CXCR3 expression in HPCE-induced PBMCs was higher than in non-stimulated PBMCs in the NHS, HAS, and PU groups, reflecting the promotion of Th1 immune responses by HP. The expression of CXCR3 in HPCE-stimulated PBMCs was higher in PU patients than in HAS individuals, suggesting that the uncontrolled activation of Th1 cells may play a role in PU development. The results of the present study indicated that in the NHS, HAS, and PU groups, CXCR3 expression decreased in the HPCE-stimulated PBMCs treated with GE (especially at the 20 and 30 µg/mL doses) compared with untreated HPCE-stimulated PBMCs. These results show that ginger has the capacity to downregulate local Th1 cell responses through reducing the expression of CXCR3, which finally mitigates immunopathological responses. In accordance with these observations, the modulatory effects of GE on the expression of CCR4 and CCR6 chemokine receptors, as well as CXCL10, CCL20, and CCL22 chemokines were indicated in an animal model of EAE (14, 20).
As a ligand for CCR6, CCL20 mainly triggers the migration of Th17 cells toward inflammatory loci (46). Mouse macrophages and human gastric epithelial cells produce CCL20 in vitro in response to HP stimulation (55, 56). Further, HP infection attracts CCR6+ CD4+ T cells towards human stomach mucosa via CCL20, inducing apoptosis in gastric epithelial cells (46). As mentioned, CCL20 recruits Th17 cells, which in turn attract neutrophils through inducing the release of neutrophil-attracting chemokines such as CXCL8 from epithelial cells and APCs (57); however, the recruited neutrophils generally fail to kill HP bacteria but lead to tissue damage. Our results indicated that in the NHS, HAS, and PU groups, the level of CCL20 production was greater in HPCE-induced PBMCs vs. non-stimulated PBMCs, as well as in HPCE-induced PBMCs from PU patients vs. their counterparts from HAS and NHS individuals. These results indicated that PBMCs from PU patients produced greater quantities of CCL20 than the cells obtained from the HAS and NHS groups. Therefore, CCL20 may play an essential role in PU development. In GE-treated cultures (especially at the doses of 20 and 30 µg/mL), CCL20 production was lower compared with untreated HPCE-stimulated PBMCs from NHS, HAS, and PU individuals. Therefore, the beneficial anti-inflammatory effects of ginger may be partly induced through modulating CCL20 production. Our data also indicated that CCR6 expression was higher in HPCE-stimulated PBMCs than in non-stimulated PBMCs in the NHS, HAS, and PU groups. Moreover, CCR6 expression in HPCE-stimulated PBMCs was higher in the PU than in the NHS group. The elevated expression of CCR6 may result in the aggregation of a large number of Th17 cells in the gastric mucosa, which in turn recruits numerous neutrophils that eventually lead to tissue damage. In addition, CCR6 expression decreased in the HPCE-stimulated PBMCs treated with GE compared with untreated HPCE cells. Therefore, it seems that ginger can downregulate local Th17 cell responses and neutrophil recruitment via reducing CCR6 expression and therefore alleviate immune-mediated tissue injury.
The ligands of CCR4 (CCL17 and CCL22) mainly trigger the migration of Th2 and Treg cells toward infectious agents. The elevated expressions of CCL17 and CCL22 have been detected in antrum biopsy specimens from HP-infected persons compared with non-infected subjects (15, 58). In H. felis-induced MALT lymphoma in mice, Treg cells were effectively recruited to the tumour microenvironment via B lymphocyte-derived CCL17 and CCL22 (59). Likewise, CCL17 and CCL22 recruit Treg and Th2 lymphocytes into stomach mucosa, limiting inflammatory and immune responses against the bacteria and leading to HP persistence mainly via secreting anti-inflammatory cytokines such as IL-4, IL-10, IL-35, and TGF-β (46). So, adequate levels of CCL17 and CCL22 may prevent harmful inflammatory responses and tissue damage; however, their overproduction recruits a large number of Th2 and Treg cells to the gastric mucosa, leading to the development of HP-associated malignancies, including gastric cancer and MALT lymphoma (46). In PU patients, we observed that CCL17 and CCL22 production was higher in HPCE-stimulated than in non-stimulated PBMCs. Therefore, it seems that in PU patients, a greater CCL17 and CCL22 production is a compensatory mechanism to limit tissue injury. Our results also indicated that CCL17 and CCL22 production was higher in GE-treated (especially at the dose of 30 µg/mL) compared with untreated HPCE-stimulated PBMCs derived from NHS, HAS, and PU individuals, indicating the modulatory effects of ginger on inflammatory responses through upregulating CCL17 and CCL22.
We also observed that CCR4 expression was higher in HPCE-stimulated PBMCs compared with non-stimulated PBMCs in the NHS, HAS, and PU groups. Also, CCR4 expression in HPCE-induced PBMCs from PU patients was lower than in their counterparts from HAS and NHS subjects. These results indicated that the PBMCs derived from PU patients expressed lower levels of CCR4 compared with the PBMCs obtained from the HAS and NHS groups. Therefore, a low expression of CCR4 may reduce the influx of Treg and Th2 cells into stomach mucosa. This phenomenon results in the hyper-activation of pathogenic Th1 and Th17 cells that play key roles in PU development. The results presented here also indicated that in the NHS, HAS, and PU groups, CCR4 expression increased in the HPCE-stimulated PBMCs treated with GE (especially at the dose of 20 µg/mL) compared with untreated HPCE-induced PBMCs. This finding suggested that ginger might upregulate local Treg and Th2 responses via increasing CCR4 expression, finally mitigating immunopathologic reactions such as PU and gastritis.
The composition of the bacterial microbiota varies in different parts of the gastrointestinal tract. In this regard, the least and most populated areas are the stomach and distal colon, respectively (60). Gastric bacterial microbiota changes during Helicobacter-associated diseases (31). In healthy persons, the bacterial microbiome mainly includes Veillonella spp., Clostridium spp., Lactobacillus spp., Streptococci, Propionibacterium, Staphylococci, Firumicutes, Bacteroidetes, Fusobacteria, Actinobacteria, and Proteobacteria. In chronically H. pylori-infected patients, the number of Actinobacteria, Bacteroidetes, and Firmicutes decreased while the frequency of Spirochetes, Acidobacteriae, and Proteobacteriae increased (31, 61). There are large populations of microorganisms in the gastrointestinal tract, which interact with each other. According to previous studies, some of the bacterial species dwelling in the gastrointestinal tract are sensitive to ginger, and this microbial sensitivity may affect the pattern of HP sensitivity to treatments.
It should be also noted that CagA+HP strains induce more potent inflammatory responses and are associated with more serious HP-linked complications compared with CagA-HP strains (62, 63). Thus, here we investigated the effects of GE on the expression of some chemokines and chemokine receptors induced by CagA+HP. Nevertheless, CagA-HP strains may similarly induce the expression of inflammatory chemokines and chemokine receptors, but at a lower extent. It seems that GE can modulate the expression of the chemokines and chemokine receptors induced by CagA-HP strains. Our study encourages conducting more investigations to clarify the effects of ginger on CagA+HP- and CagA-HP-mediated inflammatory responses.
In conclusion, the results of the present study revealed that the HPCE-stimulated PBMCs derived from PU patients expressed greater amounts of CCL17, CCL20, CCL20, CXCL10, and CCR6 compared with non-stimulated PBMCs. So, ghinger seems to have the capacity to modulate the expression of pro-inflammatory chemokines and their receptors in the PBMCs obtained from PU patients. It is suggested to perform more studies to divulge the therapeutic potentials of ginger for treating HP-related disorders.