1. Background
Postpartum hemorrhage (PPH) is a chief reason for mortality and morbidity, which each year accounts for 25% of maternal death (1). PPH refers to either loss of at least 500 cc blood from the genital tract after completion of the third stage in normal vaginal delivery or greater than 1000 mL in cesarean section (2). PPH is divided into two types of early and late bleeding. The former occurs approximately within the first 4 hours after delivery, and almost 90% of its related death occurs in this period (1). The global prevalence of PPH is 6% (3). According to the World Health Organization (WHO) report (2014), the maternal mortality rate has declined in Iran during the past two decades. Moreover, Iran is reported as one of the successful countries in achieving the Third Millennium Goals (4). PPH may either cause by one of the four disorders of tone, tissue, trauma, and thrombin, or a combination of these conditions, also referred to as the Four T’s (5). Uterine atony is the most common cause of PPH (at least 75% of cases); hence, uterine atony management is of crucial importance for PPH management (6, 7).
On the other hand, continuing PPH can cause complications such as respiratory distress syndrome, iron deficiency anemia, Sheehan’s syndrome, poor lactation, coagulopathy disorder, limb damage following hypotension, and shock (2, 8). Different mechanical, pharmacological, and surgical strategies are used to cease bleeding. For example, suggested mechanical approaches include uterine massage, a Bakri balloon, and a non-pneumatic anti-shock dress (9). Some Pharmacological strategies are also proposed, like ergomethrin, oxytocin, syntocinone, and misoprostol, and stimulate uterus contractions. Oxytocin is the most widely used drug to prevent uterine atony. However, in high doses, it causes side effects such as water poisoning, hypotension, convulsions, coma, and maternal death (2). On the other hand, despite their undeniable benefits, chemical drugs have side effects and are costly. Thus, there is a need for less risky drugs. Simultaneously, the use of herbal products is on the rise worldwide (10). In addition, herbal medicines have fewer side effects than chemical drugs. So, much attention has been paid to their use for bleeding prevention (11).
One of the medicinal plants recommended for lessening PPH is Anethum graveolens (12, 13). Its chemical constituents include tannin, resin material, and a volatile essential oil consisting of limonene, ketone, and carvone, plus a fatty substance. Tannins are often polyphenols that have contractile properties. Its fruits contain antispasmodic effects on the digestive tract and are termed as bleeding and dysmenorrhea reducer, emmenagogue, and breast milk enhancer. Mahdavian et al. (13) investigated the effectiveness of oral extract of Anethum graveolens on reducing postpartum hemorrhage and reported no adverse effects. In another study, Kinage and Chaudhari (14) suggested that receiving the extract of Anethum graveolens after delivery could reduce the PPH, mainly due to its contractional effects on uterine myometrial muscle. In a case study, moreover, side effects of Anethum graveolens (e.g. allergic reactions, diarrhea, nausea, and vomiting) are announced (15).
2. Objectives
Nowadays, the tendency to use plant medicine is increasing. The long history of using Anethum graveolens in human society, as well as the side effects of oral Anethum graveolens, have been investigated by some studies. According to the best knowledge of the authors, no study has evaluated the rectal suppositories; hence, the present study aimed to investigate the effectiveness of rectal suppository of Anethum graveolens on postpartum hemorrhage.
3. Methods
Following a randomized clinical design, 70 eligible pregnant women admitted for vaginal delivery to Umm-al-Banin Hospital in Mashhad (Iran) in 2018 were recruited in this trial. The sample size was estimated based on the average of two populations’ formula, with a 95% confidence interval and a statistical test power of 80%. Based on the results of our pilot study on 10 cases, it was concluded that 28 subjects should be selected for each group (i.e., the intervention and control). However, to ensure the adequacy of the sample size and to increase the reliability of research findings, the final sample size for each group was determined to be 35 (70 subjects in total). The subjects were selected by available method and randomly assigned into the intervention and control groups. The random sequence was performed by a statistical analyst. Potential participants were allocated to their respective groups after evaluating their eligibility. Therefore, in the present study, the analyst was blind to the allocation of participants. Data were analyzed using SPSS version 16.
3.1. Drug Formulation
Initially, the hydro-alcoholic extract of Anethum graveolens was made following the Soxhlet method. To prepare the suppository base, we mixed 60% PEG4000 and 40% polyethylene glycol (PEG) 600 based on trial and error tests, which was melted over mild thermomix heat. Then, the Anethum graveolens extract with a concentration of 290 mg was added to the obtained mixture and then was poured into suppository molds after cooling. Next, the obtained product was standardized based on total phenol by the Folin-ciocalteu method (spectrophotometric).
According to a human study, the toxic dose of Anethum graveolens is two grams, and the safe dose of Anethum graveolens is 1440 mg (13). Anethum graveolens is an Umbelliferous plant under the scientific name of Anethum graveolens. The study is approved by the Faculty of Pharmacy of Mashhad University of Medical Sciences (code: 18-0107-293).
3.1.1. Standardization Method
Initially, 1 g of Anethum graveolens was dissolved suppository in 10 cc of distilled water. Then, it was passed through a filter paper. Afterward, 1 cc of the obtained solution was diluted with 9 cc of distilled water. Then, 0.5 cc of the above solution was combined with 2.5 cc of fullene cicalto reagent and kept at room temperature for 10 minutes away from light. In the next step, 2 cc of sodium carbonate 7.5% was added to the above solution and kept at room temperature again for 30 minutes, away from light.
Finally, the optical absorption of this mixture was calculated using a spectrophotometric device at a wavelength of 765 nm, and the content of gallic acid or tannin (equivalent basis mg gallic acid) in Anethum graveolens was 245 micrograms.
3.2. Intervention
Inclusion criteria were the tendency to vaginal delivery, 38-42 weeks of gestation, 5 - 6 cm of dilatation, a score equal to or greater than 10% according to the PPH prediction nomogram, no history of cesarean section or uterine surgery, no grade 3 and 4 tears of the uterus and cervix, and no history of receiving herbal or chemical drugs before delivery, during labor, and delivery. On the other hand, exclusion criteria included unwillingness to continue the study, hypersensitivity to Anethum graveolens, C-section, and urine leakage during blood collection.
We also used content validity to determine the scientific validity of the research sample selection forms, demographic and pregnancy information, information forms of birth, infant, and placenta, as well as bleeding and laboratory information forms. The partograph form is an instrument that has been validated by the Ministry of Health. The validity of the PPH predictive nomogram is also confirmed by Biguzzi et al. (16) using the bootstrapping method. Furthermore, the validity of the plastic bag of blood collection has been determined by construct validity in various studies (e.g. Abbaspoor and Vaziri (17), Tourne et al. (18), Patel et al. (19), Ambardekar et al. (20)) (17-20). Additionally, the reliability of the partograph tool was evaluated by agreement between the observers on 10 subjects, with r = 0.98. The reliability of the bleeding prediction nomogram form was further evaluated by the observers’ agreement, with r = 0.84. Eventually, Abbaspoor and Vaziri (17) reported the reliability of the plastic bag of blood collection using the observer measurement method; therefore, we used the same method with r = 0.92.
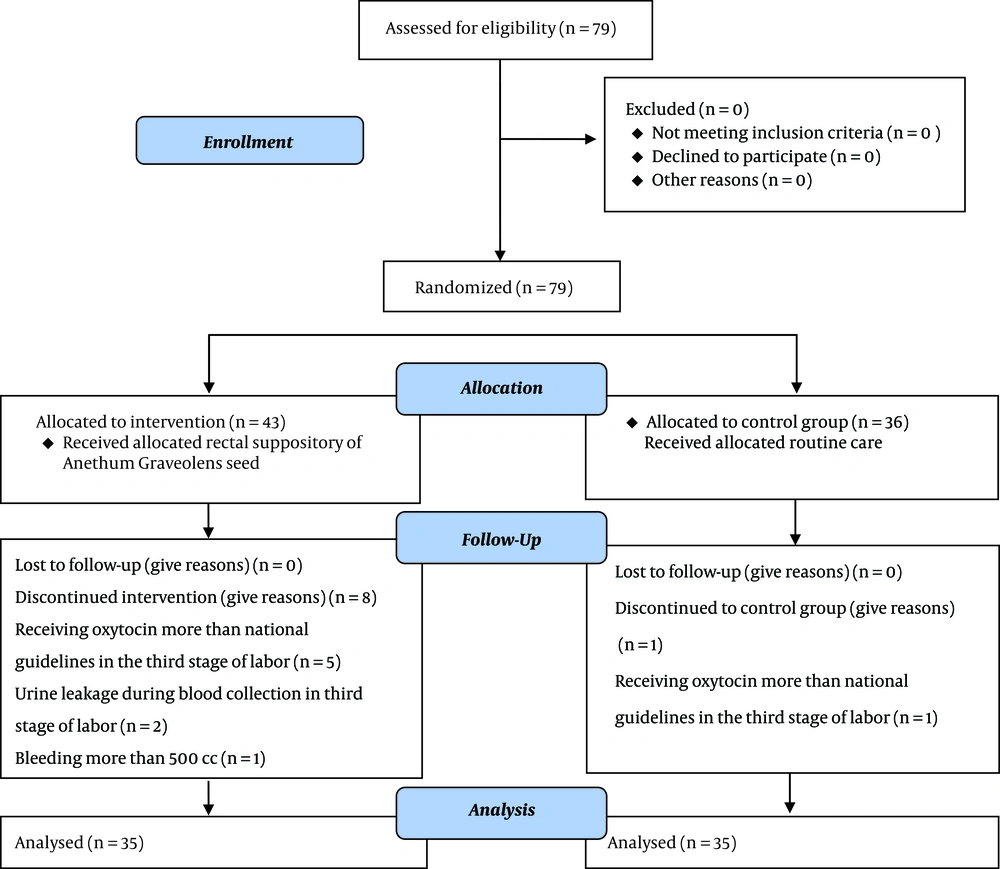
Initially, 79 patients were enrolled in the study, that 6 of them were excluded, due to the history of receiving oxytocin prophylaxis more than the amount recommended by national guidelines in the third stage of labor (five cases in the Anethum graveolens group and one in the control group). In addition, two individuals were excluded from the Anethum graveolens group due to leakage during collection. In addition, another participant in the Anethum graveolens group was also excluded due to bleeding over 500 mL and the subsequent need for aggressive and therapeutic measures. Finally, data of 70 cases (35 in each group) were analyzed (Figure 1).
The included pregnant women were referred to the hospital. After obtaining written consent and completing the sample selection form, they were randomly assigned to one of the intervention and control groups. Random allocation was performed using a random sequence generated by SPSS and cards produced based on this sequence. The researcher was present at the beginning of the active phase of labor at the patient’s bedside and recorded the information of this stage using the relevant information form. Delivery was performed in the lithotomy position, and the researcher recorded all interventions of the second and third stages of delivery.
Immediately after the childbirth, amniotic fluid-impregnated drapes were removed from the mother’s buttock and replaced with a weighed blood collection bag to measure the third stage of hemorrhage. Also, right after the complete expulsion of the placenta, fetal membranes, and uterine massage, the blood collection bag was removed and weighted (and then recorded in the bleeding information form). It worth noting that the initial weight of the blood bag was removed. Also, at this stage, other necessary information on the risk prediction nomogram were completed by the researcher, and, eventually, the score was calculated; cases with a score of ≤ 10% were removed from the study.
Moreover, instantly after the childbirth, routine interventions and injections of 30 units of oxytocin per 1000 cc of crystalloid were performed for all subjects. In the Anethum graveolens group, immediately after the expulsion of the placenta, the first dose of 290 mg of rectal suppository and subsequent doses were administered by the researcher at 30 minutes intervals. In addition, to measure the amount of bleeding at the fourth stage, immediately after removing the blood collection bag, a weighed absorbent underpad was put under the mother, and another weighed pad was given to the mother. Bleeding rates were calculated based on the weight of the during the first 4 h after delivery.
3.3. Statistical Analysis
Data were analyzed by SPSS version 22. The Kolmogorov-Smirnov and Shapirovilk tests were applied to test for a normal distribution The chi-square was used for qualitative variables. The independent t-test was applied for normally distributed variables. The Mann-Whitney test was used for other variables. Statistical significance was considered when P-value < 0.05.
4. Results
There was no significant difference between the two groups concerning demographic characteristics. In addition, laboratory results of hemoglobin and hematocrit, as well as platelet tests, were homogeneous (P > 0.05) (All participants were evaluated regarding pregnancy and delivery characteristics, such as gestational age, the number of pregnancies and delivery, history of PPH, and duration of active labor phase for which there was no statistically significant difference (i.t. they were homogeneous) (P < 0.05) (Table 1).
| Variable | Group | Significance Level | |
|---|---|---|---|
| Anethum graveolens (N = 35) | Control (N = 35) | ||
| Age, y | 25.7 ± 5.5 | 27.5 ± 6 | 0.182b |
| Hb rate, g/dL | 12.5 ± 1.1 | 12.2 ± 0.9 | 0.200b |
| Hct rate, % | 36.8 ± 2.3 | 36.5 ± 2.3 | 0.596b |
| Plt count (103) | 200.3 ± 65.6 | 207.4 ± 60.7 | 0.639b |
| Number of pregnancies | 1.8 ± 1.2 | 2.3 ± 1.4 | 0.090c |
| Number of parturition | 0.8 ± 1.1 | 1.1 ± 1.3 | 0.244c |
| GA, mo | 39.6 ± 1.2 | 39.5 ± 1.2 | 0.750b |
| Case history of PPH | 1.000c | ||
| Yes | 2 (5.7) | 2 (5.7) | |
| No | 33 (94.3) | 33 (94.3) | |
| Total | 35 (100) | 35 (100) | |
| Duration of active phase of labor, min | 75.0 ± 28.0 | 79.7 ± 28.2 | 0.491c |
Comparison of Demographic, Pregnancy and Delivery Characteristics in the Study Sample in Each Groupa
The mean and standard deviation of hemorrhage at the end of the first, second, third, and fourth hours, as well as the first four hours after delivery, were lower in the Anethum graveolens group than that of the control group. The independent t-test revealed a statistically significant difference between the two groups regarding hemorrhage rate at the third phase (P < 0.001), at the end of the first hour (P < 0.001), the third hour (P < 0.001), and the fourth hour (P < 0.001), as well as the first four hours (P < 0.001). The Mann-Whitney test also revealed a statistically significant difference between the two groups at the end of the second hour (P < 0.001) (Table 2). According to the findings, the PPH in the intervention group was significantly lower than the control group (P < 0.001) (Table 2). It should be also noted no side effect or complication was observed (e.g. nausea, vomiting, dizziness) during the study period.
| Bleeding Rate, cc | Group | Test Result | |
|---|---|---|---|
| Anethumgraveolens, mean ± SD | Control, mean ± SD | ||
| Third phase | 60 ± 7.6 | 65.7 ± 7.3 | < 0.001a |
| Fourth phase | |||
| First hour | 53.4 ± 4 | 56.3 ± 3.5 | < 0.001a |
| Second hour | 69.8 ± 5.3 | 75.7 ± 5.0 | < 0.001b |
| Third hour | 48.9 ± 6.7 | 53.1 ± 7.1 | < 0.001a |
| Fourth hour | 50 ± 5.2 | 55.1 ± 7.2 | < 0.001a |
| Total of four hours | 282.4 ± 6.9 | 306.2 ± 11.2 | < 0.001a |
Mean and Standard Deviation of Postpartum Hemorrhage in the Studied Women Separately in the Anethum graveolens seed and Control Groups
5. Discussion
In the present study, a total of 79 pregnant women were recruited, of whom 9 were removed (eight cases from the intervention group and one from the control group). Therefore, the data of 70 subjects were evaluated. According to the findings, the consumption of 1440 mg of rectal suppository of Anethum graveolens could significantly reduce the PPH. The most effective factor in reducing the PPH is the contraction of myometrium muscles. Anethum graveolens is one of the medicinal plants that can stimulate the contraction of the myometrium, which results in declined PPH.
Chemical compounds of Anethum graveolens extract include tannins, resin, and a volatile essential oil consisting of limonene, ketone, carvone, and a fatty substance. Tannins are polyphenols that have contractile properties. The fruit of this plant has antispasmodic effects on the digestive tract and has been termed as bleeding and dysmenorrhea reducer, emmenagogue, and breast milk enhancer. Due to the chemical constituents in the Anethum graveolens and their effects on uterine contractility, it is justifiable to reduce the PPH.
Mahdavian et al. (13), in a study titled “investigation of the effectiveness of oral Anethum graveolens on postpartum hemorrhage”, mentioned higher efficacy of consuming 0.018 g/mg of Anethum graveolens extract during the first and second and the first two hours after delivery on reduction of hemorrhage compared to the oxytocin, and this difference was significant. In the present study, 1440 mg rectal suppository of Anethum graveolens caused a significant reduction of the PPH. These results can be justified by the effects of the Anethum graveolens on the mechanism of uterine contraction, which is in line with the findings of the present study.
Zagami Ebrahimzadeh et al. (21), in a cohort study aimed to investigate the effectiveness of Anethum graveolens on the uterine contraction in pregnant women, reported that uterine contractions were higher in those who received Anethum graveolens than controls, so that uterine contractions were more common with less duration. Since uterine contractions play an important role in controlling the PPH, the effect of Anethum graveolens on PPH control can be justified, which is consistent with the present study.
Esmailizadeh et al. (22), in a study titled “medicinal plants with adverse effects on pregnancy”, showed that among the studied medicinal plants, Anethum graveolens could stimulate the menstrual hormones and induced menstruation and increased uterine contractions. They also reported that this plant was associated with an increased risk of miscarriage by affecting the hypothalamic-pituitary-ovary cycle. Estrogen receptor stimulation and uterine contractions are highly effective in controlling the PPH; so, the role of Anethum graveolens in controlling postpartum hemorrhage is justified, which is in agreement with the findings of the present study.
5.1. Limitations
It is necessary to mention some limitations and biases of our study, including the researcher’s confidence in the accuracy of participants’ responses and not following a double-blind design. On the other hand, the presence of the researcher from the beginning of the active phase of labor at the patient’s bedside and measuring the amount of bleeding up to four h after delivery was one of the strengths of this study.
5.2. Conclusions
According to the findings of the present study, a rectal suppository of Anethum graveolens could effectively reduce the PPH without any side effects.