1. Background
Infertility is a global problem that its prevalence varies from 5% to 30% in various countries (1, 2). Approximately 50% of infertility cases are due to male-factor infertility. The recently observed male-factor infertility is in the form of declined sperm parameters (3). It is hypothesized that these changes in sperm parameters are responsible for the recently observed increase in male-factor infertility (4).
The popularity of complementary medicine and natural remedies is on the rise worldwide, so that the World Health Organization (WHO) announced that more than three-quarters of the world's population has used various complementary methods for the treatment of different diseases at least once (5). In recent years a dramatic rise in people's inclination to use complementary medicine has been observed, mainly due to changed public belief (6). In other words, the people’s and healthcare provider's interests and beliefs toward complementary medicine are on the rise (7).
Royal jelly is the secretion product of the cephalic glands of nurse bees with important impacts on health and fertility. It has a special place in Traditional Chinees medicine, as they believed that infertile people can be cured by the royal jelly of the queen bee. Lewis reported that royal jelly can improve sperm quality in infertile men (8, 9). Royal jelly is also an important source of para-aminobenzoic acid, which is associated with increased fertility (10, 11). Royal jelly has a wide range of biological activities, which can increase seminal fructose, ejaculate volume, number of sperm output, and sperm motility (12).
In Iran, the number of Infertile people is increasing, with a higher incidence among males (13). The application of complementary methods has a long history in Iran. The holistic nature of Iranian and complementary medicines, with more than 3000 years of history, resulted in positive beliefs towards complementary medicine, such that about 70% of Iranians have used such methods at least once (1, 10).
Natural remedies, such as royal jelly, are among complementary methods that have attracted greater interest. The majority of studies intended to evaluate the effectiveness of royal jelly have followed an in vitro animal approach (11). Some human studies also have evaluated its effect on hormonal disorders in postmenopausal and low fertile women (12). Royal jelly compounds can improve testosterone and testicular function, and as a result, it increases testicular resistance to thermal stressors (14, 15).
The effectiveness of royal jelly in the treatment of low fertility is due to its compounds; so that some studies reported its ability to improve low fertility rates (16, 17). Some studies reported improved sperm function of low-fertility men following the application of royal jelly (12, 16). Since people generally have a favorable attitude toward complementary medicine, due to its availability and reasonable price, it is of interest to all, including infertile couples.
2. Objectives
Thus, it was decided to conduct a study with the aim to, firstly, evaluate the effect of royal vaginal jelly on the fertility of women with low-fertile husbands (due to asthenozoospermia) and, secondly, to compare the effectiveness of this method to the first common male-factor infertility treatment measure, namely IUI method.
3. Methods
3.1. Trial Design
The present study is a non-randomized clinical trial. This framework was selected to observe ethical considerations. It is worth noting that the current study was approved by the Ethics Committee of the Mashhad University of Medical Sciences (MUMS). This research benefited from the financial support of the Vice Chancellor for Research of MUMS (Grant number: 921175). It was also approved in Gov.rct NCT03463005. The findings of the present clinical trial are reported following the CONSORT (2010) checklist criteria (18).
3.2. Participants and Setting
The present study was conducted from 2015 to 2017 in the city of Mashhad (northeast of Iran).
Inclusion criteria were healthy women who attended Milad Infertility Treatment Center in Mashhad due to male-factor infertility problems [male-factor infertility is defined as total sperm motility < 40% and sperm concentration < 20 million/mL (19)], willingness to participate in the study, having a normal hormonal profile in the female partner in terms of hormonal profile and hysterosalpingography (HSG), and couples with regular sexual. The exclusion criteria were ovulation dysfunction in the female partner, history of sexually transmitted diseases in couples, and hormonal disorders of each partner.
3.3. Sample Size and Randomization
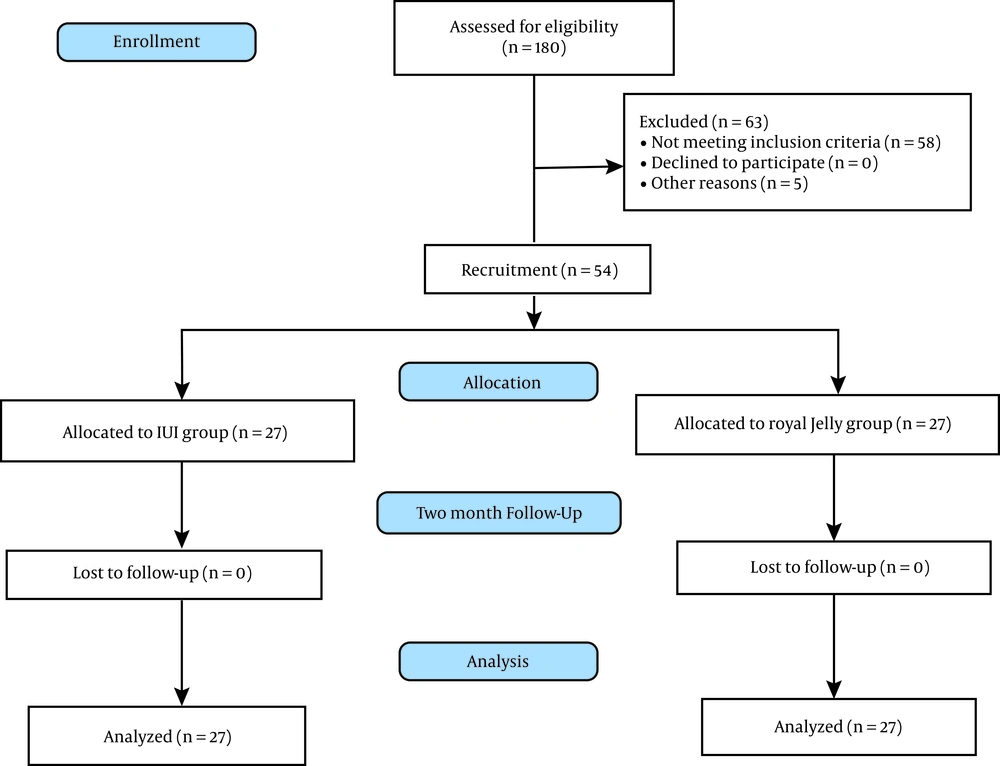
The sample size was determined as 27 subjects per group based on a previous study and using a mean comparison equation with a test power and confidence interval (5) of 80% (β = 0.84) and 95% (α = 0.05), respectively. As explained above, for ethical considerations, randomization was not possible in the present study. The study subjects were selected by purposive sampling, and voluntarily entered one of the two groups of royal jelly (n = 27) or IUI (n = 27). All participants were followed up for two months.
3.4. Study Instruments
Data were collected using a questionnaire on demographic and reproductive factors, including age, occupation, education, social class, number of pregnancies, number of children, primary or secondary infertility, age at menarche, the last menstrual cycle, and duration of infertility.
In addition, for the royal jelly group, a monthly observation checklist was used to evaluate symptoms of infection. The observation was initially performed by a gynecologist, and the checklist was completed when inflammatory and fungal diseases were ruled out. Observations during the follow-up period (i.e. two months) were made by a midwife and recorded in the abovementioned checklist.
3.5. Interventions and Outcomes
The IUI procedure was performed similarly for both intervention and control groups. All the patients received 75 IU recombinant human follicle-stimulating hormone (Cinal-F, Iran) from the second cycle day, and then the follicular size was assessed using transvaginal ultrasonography after the sixth day from menstruation. Then 10000 IU human chorionic gonadotropin was administered when follicular size was more than 16 mm in size. Then IUI was performed after 32 - 36 hours. If menstruation was retarded for more than 7 days, pregnancy was assessed based on βHCG and transabdominal ultrasonography. Subjects with positive pregnancy tests were followed up, and the pregnancy outcome was recorded.
After the selection of subjects and obtaining written informed consent, the quality of royal jelly was evaluated. The quality of royal jelly was determined based on the amount of polyphenol. Polyphenol in royal jelly was evaluated as follows: first, the sample was diluted with ethanol 50% to 1:10 ratio; then, 100µL of the specimen was poured into a test tube, and 750 µL of 1:10 diluted solution of FCR (FolinCiocalteau Reagent) was added and kept at room temperature for five minutes.
Then, 750 µL of sodium carbonate 6% solution was added to each tube, followed by maintenance at dark for one hour to measure the absorption rate (at 780 nm wavelength). The negative control consisted of all reaction compounds, except the sample, for which, ethanol 50% was used instead. The sample concentration was determined using the gallic acid standard. By definition, the desirable quality of polyphenol in natural royal jelly ranges from 0.15 (minimum) to 0.75 mg (maximum) in every 100 grams; in the present study, it was determined as 0.5 mg, indicating a good quality (20).
The study subjects in the royal jelly group used 10ml of the vaginal royal jelly a few minutes before or immediately after intercourse, which was one day after the end of menstruation for two weeks.
Semen samples were collected in sterile plastic caps after 72 hours of sexual abstinence by normal sexual intercourse. Then, for those in the IUI, samples were prepared through the standard swim-up technique. Initially, samples were rinsed with 5% of human serum Albumin and gentamicin. Then, the tubes were centrifuged. Finally, they were analyzed and washed for intrauterine insemination.
The subjects in the IUI group received 75 units of FSH from the second day of the cycle, followed by vaginal ultrasound from the sixth day of the menstrual cycle to determine the right size of the follicle. Also, 10000 units of HCG was administered when follicle diameter reached 16mm, and subjects were prepared for IUI after 32 - 36 hours.
If menstruation was delayed for more than seven days in either group, serum beta HCG was evaluated, and vaginal or abdominal ultrasound was performed to verify pregnancy. Pregnant women were monitored until the end of pregnancy to record the outcomes.
3.6. Ethical Considerations
The study protocol was approved by the Research Council of the Center for Women's Health Studies, affiliated to the MUMS (Code: 921175). Compliance with principles of ethics in research was confirmed by the regional committee of medical ethics of MUMS (IR.MUMS.REC.1393.43). In addition, written informed consent was obtained from all participants before recruitment, and they were ensured about the confidentiality of their information in all stages, including data collection, data analysis, and publication of results. Also, they were informed that they can withdraw from the study at any time.
3.7. Statistical Analysis
Data were described using appropriate statistical tables and indices such as mean. Shapiro-Wilk test was applied to test for a normal distribution. Parametric methods such as the Student t-test were used to analyze data with normal distribution, and the Mann-Whitney test was applied for other data. Data with nominal scale were analyzed using the Chi-square test (likelihood ratio), and logistic regression was used for the combined assessment of the results. SPSS version 18 was administered for data analysis. Statistical significance was considered when p-value < 0.05.
4. Results
A total of 54 spouses were recruited, and all of them completed the study (Figure 1). According to the findings, there was no significant difference between the two groups concerning the spouse's age, occupation, education (husband and wife), or social class (P = 0.745) (Table 1). However, no significant difference was found between the two groups in terms of spouse's age, occupation, education (husband and wife), or social class (P = 0.745).
| Variable | IUI Group | Royal Jelly Group | P-Value a |
|---|---|---|---|
| Age | 29.0 ± 4.5 | 29.3 ± 5.6 | 0.831 b |
| Husband’s age | 32.8 ± 5.7 | 33.3 ± 6.0 | 0.745 b |
| Duration of infertility (y) | 5.5 ± 3.0 | 5.7 ± 4.0 | 0.739 c |
| Occupation, No. (%) | 0.126 d | ||
| Housewife | 22 (81.5) | 17 (63.0) | |
| Employed | 5 (18.5) | 10 (37.0) | |
| Husband’s occupation, No. (%) | 0.378 d | ||
| Employed | 7 (25.9) | 10 (37.0) | |
| Self-employed | 20 (74.1) | 17 (63.0) | |
| Education, No. (%) | 0.776 d | ||
| Nonacademic | 18 (66.7) | 17 (63.0) | |
| Academic | 9 (33.3) | 10 (37.0) |
aSig P > 0.05
bStudent test
cMann-whitney test
dLikelihood ratio test
Comparing the effects of vaginal royal jelly and the first line of conventional treatment of low-fertility due to asthenozoospermia showed no significant difference between the two groups concerning pregnancy outcomes (P = 0.573). Thus, royal jelly and IUI groups were not significantly different in terms of pregnancy rate (Table 2). A logistic regression model was used to evaluate the results. According to the findings, age was the only factor associated with the pregnancy outcomes (P = 0.573) (Table 3).
| Pregnancy Outcome | IUI Group | Royal Jelly Group | Total |
|---|---|---|---|
| Positive | 11 (40.7) | 9 (33.3) | 20 (37.0) |
| Negative | 16 (59.3) | 18 (66.7) | 34 (63.0) |
| Total | 27 (100.0) | 27 (100.0) | 54 (100.0) |
| Probability | P = 0.573 | ||
aValues are expressed as No. (%).
| B | SE | Wald | df | Sig. | Exp(B) | 95% CI for Exp (b | ||
|---|---|---|---|---|---|---|---|---|
| Lower | Upper | |||||||
| Group (IUI VS royal jelly) | 0.311 | 0.634 | 0.241 | 1 | 0.623 | 1.365 | 0.394 | 4.728 |
| Age | ||||||||
| ≤ 30 compared > 30 years | -2.051 | 0.922 | 4.949 | 1 | 0.026 | 0.129 | 0.021 | 0.783 |
| Occupation | ||||||||
| Housewife compared to employed | 0.687 | 0.812 | 0.717 | 1 | 0.397 | 1.988 | 0.405 | 9.757 |
| Education | ||||||||
| Nonacademic compared to academic | -0.843 | 0.736 | 1.312 | 1 | 0.252 | 0.430 | 0.102 | 1.821 |
| Spouse's occupation | ||||||||
| Employed compared to self-employed | -0.190 | 0.776 | 0.060 | 1 | 0.807 | 0.827 | 0.181 | 3.785 |
| Duration of infertility | -0.099 | 0.135 | 0.534 | 1 | 0.465 | 0.906 | 0.695 | 1.181 |
| Model constant | 0.719 | 1.494 | 0.232 | 1 | 0.630 | 2.052 | ||
5. Discussion
The present study intended to evaluate the effect of vaginal royal jelly on the fertility rate in women with low-fertility husbands (male-factor infertility) compared to the first-line infertility treatment measure with male-factor, namely IUI. The results showed no significant difference between success rates of royal jelly and IUI in terms of pregnancy.
Although performing IUI is the first practical stage in treating low fertility and infertility due to various causes, it is used as the first line of treatment in male-factor infertility (21). A systematic review reported that this rate depends on a variety of factors, and it ranges from 5% to 70% for each patient, based on the cause of infertility (22). It appears that the success rate of IUI treatment with a male-factor cause is not high, as Badawy showed that sperm motility, count, and morphology hugely affect the success rate of this method, and a mean success rate of 5.55% in male-factor infertility indicates IUI treatment has not been very successful (23). In the present study, the success rate of IUI treatment was 40.7%. It seems that participant’s age and their awareness about having regular intercourse are the most important items for higher success rates in both groups.
However, the participants were trained about how to have regular intercourse (every 48 hours). In their extensive study on 353 couples, Merviel et al. identified that the highest success rate following IUI treatment was related to women younger than 30 years (24).
In addition to women's age, men's age also affects the success rate of IUI. In a retrospective study on 138 infertile couples, Kdous et al. argued that men younger than 38 years had more success with the IUI method. The mean age of men in both groups was about 33 years (25).
Few human studies investigated the effect of royal jelly. For instance, Al-Sanafi et al. (2007) studied the effect of oral royal jelly on sexual hormones and sperm parameters in men, and reported that the quality of sperm parameters depends on the dose of royal jelly, as men who used a daily dose of 100 grams of the jelly experienced better results (26). Regarding the effect of royal jelly on the fertility rate of women with low-fertility husbands, a study by Abdelhafiz can be cited, which identified a significant difference between royal jelly and IUI in the treatment success rate, such that pregnancy rate was 8.3% in the royal jelly group and 2.6% in the IUI. The difference between Abdelhafiz and the present study can be attributed to the different compositions of royal jelly used. In Abdelhafiz's study, royal jelly contained honey and flower pollen. Thus, the high success rate of treatment, as well as realization of pregnancy in his study, cannot be attributed to royal jelly alone (16).
In the present study, no additive was used with royal jelly, fearing the likelihood of allergy because pollens are the major allergen in Iran. Therefore, this composition was not used to avoid possible allergies (27). The strengths of the present study include the purity of royal jelly, which was not mixed with other substances, examining the amount of polyphenol it contained, and lower price compared to the IUI method.
5.1. Study Limitation
The most important limitation in the present study was the non-randomization of participants because it contradicted participants' wishes as well as research ethics. Another limitation was the lack of placebo use to determine the success rate of royal jelly. Also, the IUI group received control ovulation stimulation, while those in the royal jelly did not receive it.
As the study was non-randomized, its findings do not have the required level of evidence for recommending royal jelly as a therapy. Therefore, there is a need for further randomized clinical trial studies to confirm the findings of this study.
5.2. Conclusions
As treatment success rates of royal jelly and IUI were similar, it seems that royal jelly can be considered as an alternative treatment option. Simplicity, low cost, and not using medications with many side-effects are the most important advantages of royal jelly over IUI.