1. Context
Mouth rinses are commonly used for the removal of microbial plaque. Plaque-induced gingivitis and the inflammation of the periodontium can eventually lead to periodontal diseases. Plaque‐induced gingivitis causes swelling, redness, and the tendency for easy bleeding of the gingiva during brushing or flossing. Inflammation in the bony and soft supporting structures of the teeth ultimately results in periodontal bone defects and tooth loss (1). Periodontal bone defects can also be caused by trauma and congenital anomalies, and ultimately need further bone transplantation in order to regenerate the lost periodontal tissues (2). However, multiple approaches can be used to reduce gingivitis. Mechanical plaque control using toothbrushes, dental floss, and professional scaling and polishing are commonly used methods that are not able to completely prevent the accumulation of bacteria on the surface of teeth and attached gingiva (1, 2). Therefore, using mechanical methods exclusively is ineffective in removing 100% of dental plaque. In such cases, mouthwashes, in addition to mechanical oral hygiene, effectively decrease the number of micro-organisms in the oral cavity (3).
Numerous organic and non-organic mouthwashes are available in the market (4). Chemical mouthwashes, including Triclosan, Listerine, and chlorhexidine are commonly used by people. The approved material in chemical plaque control is chlorhexidine, which effectively reduces plaque accumulation (5). However, this mouthwash cannot be applied for longer periods of time because of its side effects, like restorative materials, brown discoloration of the teeth, tongue and mucosal erosion in high concentrations, swelling of the parotid gland, and an increase in the formation of calculus (6, 7).
Due to the adverse effects of chlorhexidine, herbal medicine as an alternative has recently received a considerable research attention. With the development and increasing reputation of natural products, the Aloe vera mouthwash has been introduced to aid plaque control and treat gingivitis with no remarkable side effects (8). Aloe vera belongs to the Liliaceae family with mucilaginous tissue in its leaf’s center. This medicinal plant has taken on added importance in clinical research. It has been widely used to treat gastrointestinal issues, sunstroke, and ulcers (9).
The pharmacological effects of Aloe vera include anti-arthritic, anti-inflammatory, anti-viral, antioxidant, anti-fungal, anti-bacterial, and hypoglycemic effects (10). Studies have reported the anti-inflammatory effect of Aloe vera, where the gel exerts its anti-inflammatory property through inhibition of COX2, prostaglandins, and bradykinins, through the inhibition of TNF-α, I.N.L.- 1β, and extracellular signal-regulated kinase pathway. Studies have also demonstrated that the Aloe vera gel's main active components are saponin, aloin, aloemannan, aloe-emodin, acemannan, sterols, aloeride, amino acids, and vitamins (11). The pulp of Aloe vera contains 98.5% of water, and the remaining include a range of compounds like vitamins, organic acids, carvacrol, anthraquinones, lignin, and sugar (12).
Furthermore, Aloe vera has been used to treat many dental and oral disorders, like oral lichen planus (13), aphthous stomatitis (14), oral submucous fibrosis (15), and bone regeneration (16). Recently, studies have investigated the effect of Aloe vera on issues other than periodontal diseases to show the positive impact of this plant on treating different oral diseases. This study aimed to determine the quality of reliable articles investigating the effects of Aloe vera mouthwash on the treatment of mucositis (17), periodontal surgery sites (18), and the number of colony-forming units during scaling and root planning (19). Overall, the present study aimed to review the available databases in order for evaluating the efficacy of Aloe vera mouthwash compared to other similar mouthwashes by considering the given conditions.
2. Methods
2.1. Search Strategy
The data examined in the present review were extracted from papers published from 2000 to 2020 and retrieved from official databases, including Scopus, PubMed, and Microsoft. The titles and abstracts of all documents were screened by two individuals, and irrelevant articles were excluded. An internet search was conducted to find all relevant articles using the keywords Aloe vera, Aloe vera mouthwash, Aloe vera mouth rinse, as well as dentistry and, then, randomized controlled trial articles with detailed information regarding Aloe vera mouthwash and its clinical effects were selected. Two authors extracted full texts of all qualified studies and assessed them separately.
2.2. Data Extraction
Two authors collected information on study design, the number of participants, age range, gender, duration, journal of the indicated article, clinical parameters, author and country of study, and the main outcomes of each article, independently.
2.3. Literature Search and Study Selection
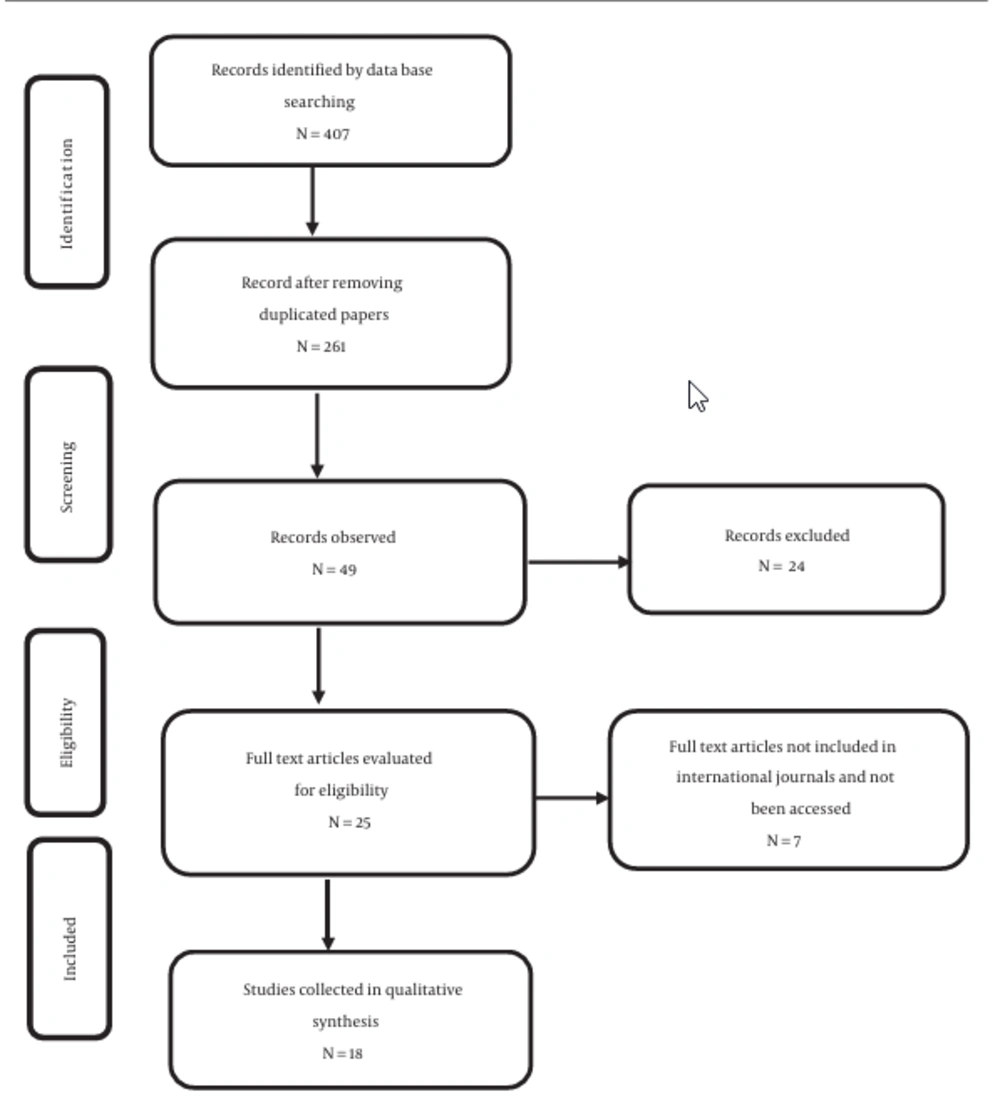
The initial searching included 407 (Scopus = 129, PubMed = 128, and Microsoft Research = 150) studies. Of these, 146 were duplicated and finally removed. The full texts of 25 studies were retrieved by two independent reviewers. Three of these papers were excluded because they were not published in international journals. Two studies were not accessible through official web pages (17, 20). Two studies were excluded since they failed to meet the inclusion criteria of the present study. The remaining 18 studies were included in this review (Figure 1).
3. Results
3.1. General Features of the Included Studies
A total of 18 randomized controlled trials (RCTs) on 1731 patients were evaluated. These studies were designed in different countries, including India, Iran, Malaysia, and Syria. The enrolled subjects had been generally healthy in all intended studies with no history of the systematic disease, except for the enrolled patients in one study who had been afflicted with head and neck cancer (17). The main exclusion criteria in these studies were the current use of anti-inflammatory, anti-biotic, anti-histamines, smoking, alcohol drinking, having a history of allergy to any herbal mouthwashes, and pregnancy. The evaluation period of all studies varied from 4 days to 8 weeks. One study assessed the efficacy of Aloe vera in reducing aerosol contamination during ultrasonic scaling (19). Thirteen studies had reported both gender and age of volunteers (age range: 8 - 73). Three studies had reported the gender of the participants and described the age of participants with exact details. Two studies had not included the gender or the age of the participants.
3.2. Intervention and Comparison of Different Groups
The effect of Aloe vera and those of different herbal and chemical mouth rinses had been compared by these studies, including CHX (0.2% and 0.12%), Triphala, tea tree oil, emoform, Benzydamine, matrica, Cholorin dioxide, and 1% PVP-1. Two studies had evaluated the effect of Aloe vera as an adjunct to SRP (21, 22), and one study had compared the effect of the combination of Aloe vera and green tea with the effects of other groups (23).
3.3. Clinical Parameters
Different periodontal indices including gingival index (GI) (Leo and Sillness, Lobene), plaque index (PI) (Loe and Sillness, modified Loe and Sillness, Quigley Hein PI, Turesky modification of Quigley Hein PI), gingival bleeding index (GBI) (Ainamo and Bay, Saxton), plaque area (PA) (Renton and Claydon) and dental stain index (Lobene) had been used in all studies investigating periodontal disease.
Other parameters having been evaluated included:
• Microbiological analysis to determine the salivary S.mutans account (24),
• Edema, trismus, dry socket prevalence, and VAS for pain (25),
• Mucositis severity (17),
• Colony-forming units (CFUs) (19)
3.4. Main Outcomes
3.4.1. Gingival Index
Five Studies had concluded that the differences between Aloe vera and chlorhexidine groups regarding the decrease in gingival inflammation had been statistically significant and equally efficient. Also, the impact of Aloe vera- green tea mouthwash had been found equivalent to chlorhexidine and more significant than the matrica mouthwash (23). However, two studies had demonstrated that the Chlorhexidine group had shown a maximum decrease in the GI than the Aloe vera group; however, the differences had been described as insignificant (P > 0.05) (20, 26). A study by Penmetsa et al. had shown that the Triphala group had effectively demonstrated a higher GI reduction than the Aloe vera group (P = 0.00) (27). Chlorhexidine, compared to Aloe vera, had been found to significantly reduce the gingival index scores in two studies. Chlorhexidine, compared to Aloe vera, had also been detected to significantly reduce gingival and plaque scores (28, 29). The results of two studies had revealed that gingival inflammation reduction had been higher in groups treated with SRP and Aloe vera mouth wash (P < 0.05) (21, 22).
3.4.2. Plaque Index
Seven studies had reported that Aloe vera had been as effective as chlorhexidine regarding plaque index reduction because no statistically significant difference had been observed between the two groups. Nonetheless, four papers had found that chlorhexidine had been more effective than Aloe vera in reducing plaque; however, the differences had been described as statistically insignificant (26, 30). Two studies had shown that the effect of chlorhexidine on reducing the plaque index had been markedly higher than that of Aloe vera group (28, 31). The Alnouri et al. study had demonstrated that the decrease in plaque index in the Aloe vera group had been significantly greater than that in the chlorhexidine group (P = 0.00) (32).
3.4.3. Gingival Bleeding Index
A higher and similar reduction had been seen in the Triphala and chlorhexidine groups, which had been significantly different from that in Aloe vera group (27). The Chandrahas et al. study had shown that chlorhexidine had been somewhat more effective than Aloe vera in reducing the bleeding index (28). Aloe vera- green tea mouth rinses had represented a similar reduction of the bleeding index compared to matrica and was described as effective as chlorhexidine in studies by Alnouri and Yaghini et al. (23, 32).
3.4.4. Plaque Area
Only one study reported this variable. The mean plaque area in the Aloe vera mouthwash had been between the other two test rinses (negative and positive test rinses). A significant difference had been recorded for plaque parameters when comparing chlorhexidine with Aloe vera and placebo mouth rinses (P < 0.0001) (31).
3.4.5. Dental Stain Index
One study assessed the effects of Aloe vera-green tea, matrica, and chlorhexidine on the dental stain index. They had concluded that the alterations in the chlorhexidine stain index had been markedly greater compared to those in the other three groups (P < 0.001); however, the difference between other two groups had not been significant in terms of the given index (P-value for ALV = 0.17, P-value for matrica = 0.054) (23).
3.4.6. Other Parameters
Fallahi et al. reported that the Aloe vera group had shown less edema compared to the normal-saline group a few days after usage. However, the data was only significant on day three (P < 0.029). Postoperative pain had been markedly reduced in the Aloe vera group than that in the normal saline group (P < 0.023). Also, the prevalence of trismus and dry socket had been reported to be less in the Aloe vera group than in the control group over the follow-up days. However, no statistical significance had been observed for this reduction (25).
Salivary S. mutans accounts had been evaluated in one study. A highly significant decrease had been observed in scores and counts in the Aloe vera, tea tree oil, and chlorhexidine groups for these parameters. No significant difference had been detected in the parameters when the three groups were compared with each other (24). The amount of mucositis severity recorded in the study designed by Sahebjamee et al. had shown that changes in the severity of mucositis over the following days had been statistically similar in both given groups. Both treatments failed to exert a significant effect over time (17).
Only one study counted the number of colony-forming units (CFUs) on blood agar plates. According to the results, a statistically significant difference had been discovered between the chlorhexidine and PVP-I* groups, and Aloe vera and PVP-I groups regarding the CFU counts. No difference had been observed between the chlorhexidine and Aloe vera groups in any regions (P = 0.456) (19).
3.5. Side Effects
Ten studies had documented no side effects after using Aloe vera compared to other mouth rinses, including chlorhexidine, clorindioxide, Triphala, and benzydamine, which had shown significant side effects. In a study by Gupta et al., staining (mild brown discoloration of teeth) was observed in 70 patients in the chlorhexidine group. Also, 65 subjects in the chlorhexidine group experienced a sense of unpleasant taste after using this mouthwash. At the same time, no such side effects had been recorded for the Aloe vera group (8). Furthermore, Chhina et al. argued that 40% and 25% of the subjects in chlorhexidine group had complained of stains and taste changes, respectively; while the participants in Aloe vera group had experienced no (0.00%) stains and only 2% of them had complained of taste change (30). The presence of stains on teeth surfaces and the tongue had led to an increase in the risk of bias. Therefore, the reasonable period for evaluating mouth rinses' efficacy on periodontal indices had been considered to be two weeks.
4. Discussion
To the best of our knowledge, the present study was the first narrative review conducted to evaluate the potency and efficiency of Aloe vera mouth rinses compared to other chemical and herbal mouth rinses as an adjuvant or primary treatment. Due to their productive pharmaceutical contents, chemical mouthwashes, including Triclosan, Listerine, and chlorhexidine, are among the most appropriate adjuvant treatments adjacent to SRP or any common oral surgeries (28). Chlorhexidine has been considered a gold standard due to its significant effect on removing microbial plaque and inflammation. This mouth rinse is able to maintain its anti-microbial properties for up to ten hours in the oral cavity (5). Despite food and drug administration validation, using this mouthwash for extended periods of time may cause side effects, including teeth and tongue staining, taste sensation changes, enhancement in the formation of calculus, unilateral and bilateral swelling of parotid glands, and cancerous effects (6). Therefore, using chlorhexidine mouthwash for more than two weeks is contraindicated as it can induce the regrowth of microbial plaque and recurrent periodontal diseases (7). The Aloe vera plant has anti-fungal, anti-inflammatory, antioxidant, immune-modulating, and anti-bacterial properties (26). Numerous in-vitro and in-vivo studies on gingivitis have shown that inflammatory factors such as TNF-α and INL-1β are decreased after treatment with Aloe vera extract (20).
The Central gel of Aloe vera leaves contains valuable substances such as aleosin, aloe-emodin, aloin, vitamins, and amino acids. They inhibit cyclic oxygenase enzymes and prevent converting arachidonic acid to prostaglandins. The antiplaque anti‐inflammatory properties of Aloe vera could lead to a decrease in gingivitis (11). In contrast, the effect of chlorhexidine on reducing inflammation is due to its antiplaque effects (33). In our review, it was argued that Aloe vera mouth rinse was safe and tolerated mainly by patients with no or very few side effects compared to other similar mouthwashes (33). According to primary results of the present review, a decrease was observed in periodontal indices, and parameters, including salivary S. mutans account mucositis severity and colony-forming units after the application of Aloe vera mouthwash.
Fifteen studies that assessed the Aloe vera efficacy on plaque indices were investigated in the present review. Although five studies had demonstrated that Aloe vera rinses may have been as effective as chlorhexidine in decreasing the plaque index, two papers had reported that chlorhexidine had been significantly more effective in reducing plaque than Aloe vera. The differences were not significant statistically. Moreover, two studies had shown that the reduction of gingival inflammation had been higher in the group receiving SRP and Aloe vera mouth wash (21, 22). One study revealed that Aloe vera and green tea mouthwash combination had been similar to chlorhexidine and stronger than matrica in reducing gingival bleeding and the gingival index (23). A higher and equal reduction of sulcus bleeding index had been recorded for Triphala and chlorhexidine groups, which had been significantly different from that for Aloe vera group (27). This was consistent with the result from Chandrahas et al. study, which had reported that chlorhexidine had been more efficacious in reducing the mean bleeding index than Aloe vera mouthwash (28).
Comparing their results with findings from a study by Yaghini et al., however, Aloe vera- green tea mouth rinses was found to have shown a similar reduction of the bleeding index compared to matrica and been as effective as the chlorhexidine mouthwash (23). Plaque-induced areas had been evaluated in only one study, and the mean plaque area in the Aloe vera mouthwash had been between the other two test rinses (31). One study had reported the effect of Aloe vera-green tea, matrica, and chlorhexidine on dental stain index. It indicated that the mean changes had been markedly higher in the chlorhexidine group than in other groups (23). Fallahi et al. had shown that Aloe vera had presented less swelling, trismus, dry socket, and Postoperative pain than the control group over the follow-up days (25). Salivary S. mutans accounts had been evaluated in one study; it had found a highly significant decrease in counts and scores in chlorhexidine, Aloe vera, and tea tree oil mouth rinses. No significant difference had been recorded in the mentioned elements when comparing all groups with each other (34). The mean changes in the severity of mucositis in the benzydamine and Aloe vera groups had been statistically similar, as both treatments' efficacies had not changed significantly over time (17). The effect of Aloe vera rinse on reducing aerosol contamination during SRP had been equal to that of chlorhexidine, and the number of colony-forming units (CFUs) had been reported to be lower than 1% PVP-I in both groups (19).
The reviewed studies faced certain limitations, one of which was the lack of studies assessing the effects of Aloe vera mouth rinse and its properties on other issues in dentistry other than periodontal disease. Only three studies had concluded that Aloe vera may had been applied for treating mucositis severity in patients with head and neck cancer (17) as well as for decreasing the amount of S. mutans in the oral cavity (24) and the number of colony-forming units during SRP (19). All these studies had been conducted in particular countries – in India and Iran, particularly. Thus, our study results may not have been generalizable to populations in other regions. Moreover, the failure to retrieve the full text of two articles relevant to this subject was another limitation of the present study (18, 35).
4.1. Conclusions
It was concluded that Aloe vera mouthwash was as beneficial as other commercial mouthwashes and, therefore, it may have been considered as a suitable alternative to other chemical mouthwashes. It showed promising results in alleviating the severity of radiation-induced mucositis and periodontal disease, reducing the amount of S. mutans and the number of colony-forming units during SRP, and dealing with other situations needing a mouth rinse for treatment.