1. Background
Female sexual dysfunction (FSD) is defined as varying degrees of persistent or recurrent decline in sexual activity or sexual aversion, arousal disorder, inability to reach orgasm, and pain during sexual intercourse, as a single complaint or a group of complaints lasting more than six months. The prevalence of sexual dysfunction is higher in postmenopausal women and reaches 68 to 86.5%, depending on the study location (1). Most sexual problems in postmenopausal women occur in sexual desire, arousal, orgasm, and sexual activity. Hormone replacement therapy improves sexual function in postmenopausal women (2). Major side effects associated with hormone replacement therapy include cardiovascular disease, breast cancer, ovarian and endometrial cancer, stroke, and thromboembolism (3).
In recent years, herbal medicine has become one of the most common options for improving sexual function. Approximately 51% of women use complementary and alternative medicine, and more than 60% of them believe that complementary medicine is effective in treating sexual dysfunction (4-7).
The vitex plant (Vitex agnus-castus), with the common name "Chaste tree," is a flowering plant of the Verbenaceae family. This plant is native to Central Asia. Its exact mechanism for improving sexual desire has not been proven. However, it seems to reduce the release of follicle-stimulating hormone and prolactin and increase the release of luteinizing hormone from the pituitary gland by affecting the hypothalamic-pituitary axis. Its chemical compounds include flavonoids (casticine, tetramethyl ether, trimethyl ether, hydroxy kaempferol, and quercetagenin), iroid glycosides (genocide and aucubin), essential oils (alpha and beta-pinene, cineole 1 and 8, sabinene, bornyl acetate, and p-cymol), and fatty acids (8-11).
Laurus cinnamomum, with the common name "Cinnamon," is a medicinal plant with various uses. Different parts of this plant, including cinnamon bark, expose many healing properties. In traditional medicine, it is used as the main drug to strengthen the heart, stomach, and intestines, improve kidney function, and increase sexual potency. It contains cinnamic aldehyde, eugenol, tannin, starch, safrole, cinnamyl acetate, mucilage, calcium oxalate, sugar, mannitol, cinnamon, essential oil, and resin. Cinnamon essential oil, the only important part of cinnamon, is present in the barking amount of 1% and is also obtained by water distilling. This essential oil is bright yellow when fresh, but over time, due to oxidation, it turns golden yellow and then reddish brown. This essential oil primarily consists of cinnamic aldehyde (12).
Menopause, midlife crisis, and aging affect women's sexual intercourse and quality of life. On the other hand, considering the side effects of hormone therapy, herbal medicines and supplements have become very popular in treating and managing menopausal symptoms and complications (13). Cinnamon and vitex may also improve sexual function due to the mentioned therapeutic properties.
2. Objectives
Considering that limited interventional studies have been conducted on the effect of cinnamon or vitex on improving the sexual function of postmenopausal women inside and outside Iran, this study aimed to investigate and compare the effect of cinnamon and vitex oral capsules for improving sexual function in postmenopausal women in Tehran.
3. Methods
3.1. Study Design
This triple-blind randomized clinical trial was conducted in health service centers in Tehran, Iran, in 2020, with the ethical code IR.SBMU.PHARMACY.REC.1398.234 and clinical trial code IRCT20200504047999N1. This study was conducted following the Declaration of Helsinki (14).
With a type I error of 5% (α = 0.05) and a power of 95% (β = 0.95-1), the sample size in each group was calculated to be 32 people. There were 35 participants in each group to consider the dropout (total n = 105). As we had three groups (r = 3), the analysis of the variance table was used to determine the sample size. To use this table, the number of groups in this study was 3; the Δ/σ quantity must also be known, where σ is the standard deviation, and Δ is the difference between the maximum and minimum average score of sexual function (15).
The random number table method was used for the random selection of health service centers for sampling. Four centers were randomly selected. By referring to the selected comprehensive health service centers, the researcher found the files, addresses, and phone numbers of postmenopausal women, invited them through the health interface, and organized a meeting for them. In the meeting, after introducing and familiarizing them with the nature of the intended research, they were included in the present study if they gave their consent and met the research criteria.
A random number function was used to randomize and assign individuals to groups. Randomization was done using Excel software: Firstly, groups were entered in one column as title group A, group B, and group C accordingly. In the opposite column, random numbers were generated using the RAND command. In the next step, using the sort command, the generated random numbers were sorted from small to large, which changed the order of the groups, i.e., C, A, and B. Using the new order, people were assigned to different groups. Informed consent was obtained from the participants. All research information was kept confidential. Also, the researcher, participants, and statistical consultant were blinded.
Inclusion criteria for menopausal women were Iranian nationality, passing at least one year after the last menstruation, no desire or obligation to use hormone replacement therapy, no chemical or herbal medicine use, being sexually active, not being addicted to smoking, drugs, or alcohol, no recent use of antidepressants and anti-anxiety drugs, no known mental illness, and not using herbal teas while taking medicine. Subjects who showed a possible allergy to capsules did not take the capsules for a week or more or were unwilling to continue treatment were excluded from the study. At first, Beck and Spielberger's scale was used to assess depression and anxiety. The reliability of the Beck questionnaire has been reported to be 0.83 to 0.96 using Cronbach's alpha coefficient (16, 17). Marteau and Bekker (1992) and Spielberger and Gorsuch (1983) reported good validity and reliability for the Spielberger State-Trait Anxiety Inventory (18).
If the participants did not have depression and anxiety, they were given the demographic and midwifery profile and the Female Sexual Function Index (FSFI) questionnaires, in sequence. The Female Sexual Function Index was developed in 2000 (19) to assess female sexual dysfunction based on the models described in DSM-5 and ICD-10 (20). This questionnaire includes 19 items that measure sexual function in the areas of sexual desire, arousal, orgasm, moisture, sexual satisfaction, and pain during intercourse (21). The total score of 26.55 has been determined as the optimal cutoff point for differentiating women with sexual dysfunction from women without the disorder (20). This questionnaire has internal consistency (Cronbach's alpha ≥ 0.82) and high open-test reliability for each domain (Spearman = 0.79 - 0.86) (22).
In this study, each of the cinnamon and vitex groups consumed 400 mg oral capsules containing the extract powder of these plants, such that the desired dose was determined according to the daily therapeutic dose of cinnamon and vitex in the Physicians' Desk Reference (PDR) book and confirmed by the research's pharmacist (11). The placebo group also received 400 mg capsules containing dry bread powder. These capsules were prepared and coded by the pharmacist in the Faculty of Pharmacy of Shahid Beheshti University of Medical Sciences and were similar in appearance. The capsules were put together so that they did not smell different. The researcher, research units, and statistical consultant professor were unaware of the coding and what kind of medicine each envelope contained, and only the pharmaceutical consultant of the research was aware of the coding of the envelopes and the type of drugs. Nevertheless, due to ethical issues, there was an immediate notification mechanism about the codes so that if a problem occurred in the menopausal lady, her doctor would be aware of the medicine she was taking.
Participants in groups A, B, and C took two capsules daily, one after breakfast and the other after dinner, for two months (11). Each week, the participants were monitored by phone call for correct drug use and possible side effects, and the researcher's phone number was provided to the participants.
At the end of the study (two months later), the FSFI questionnaire was given to the participants again. Because the FSFI measures the level of sexual function in the last month, one month after the end of the intervention, the sexual function questionnaire was given to the participants again. Then, the scores of FSFI before and after the intervention were compared.
Descriptive and analytical statistics were utilized in the present study. One-way ANOVA, Kruskal-Wallis, chi-square, Fisher tests, two-way ANOVA, and Bonferroni test were used to describe the groups. SPSS version 21 software was used for analysis.
4. Results
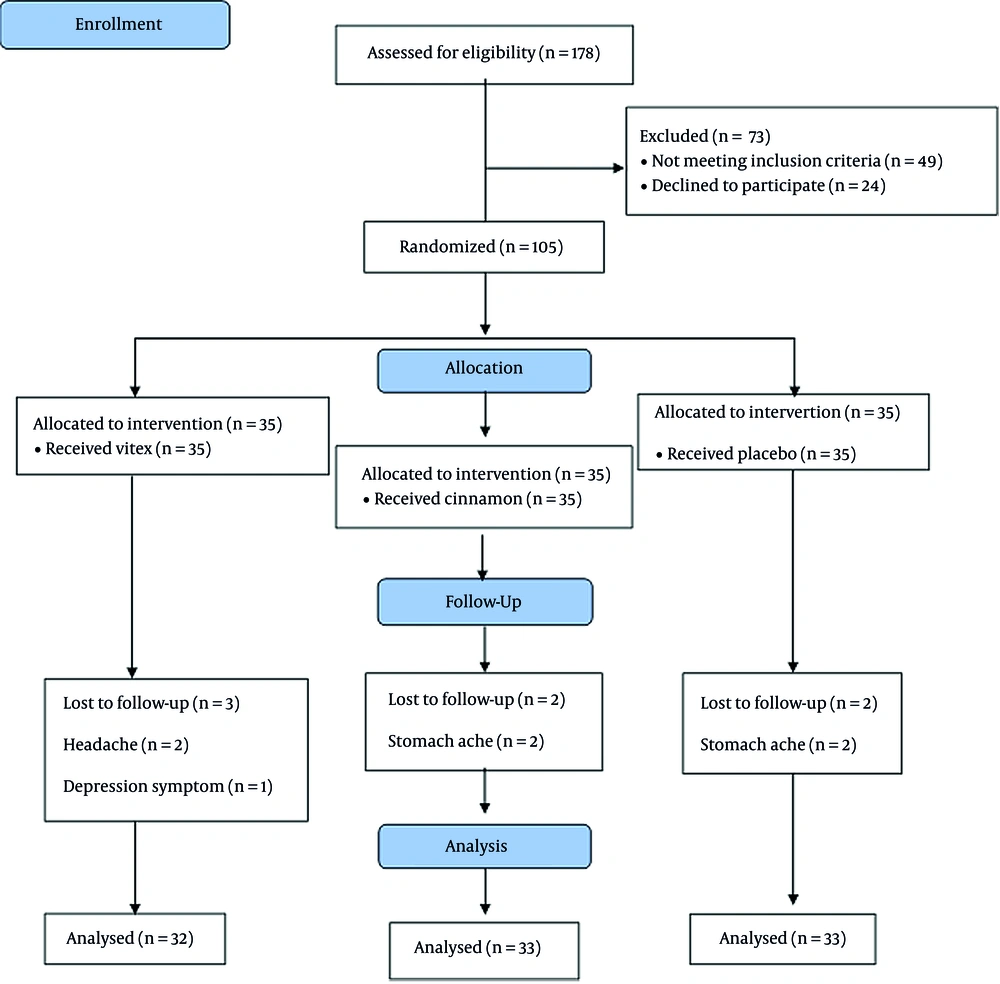
The CONSORT flow chart demonstrates the study process (Figure 1).
Tables 1 and 2 show no statistically significant differences between the three groups in terms of demographic and obstetric characteristics (P > 0.05) (Tables 1 and 2).
| Groups | Placebo | Cinnamon | Vitex | P-Value (One-way ANOVA) |
|---|---|---|---|---|
| Age | 55.30 ± 4.14 | 53.96 ± 3.33 | 54.09 ± 3.64 | 0.282 |
| Spouse age | 60.48 ± 4.71 | 60.45 ± 5.05 | 59.25 ± 3.91 | 0.471 |
| Duration of marriage | 30.33 ± 4.18 | 32.03 ± 3.48 | 31.87 ± 3.89 | 0.150 |
Demographic Profile of Vitex, Cinnamon, and Placebo a
| Groups | Placebo | Cinnamon | Vitex | P-Value |
|---|---|---|---|---|
| Job | 0.8 | |||
| Employed | 9 (27.3) | 10 (30.3) | 12 (37.5) | |
| Houseewif | 20 (60.6) | 17 (51.6) | 16 (50) | |
| Retired | 4 (12.1) | 6 (18.1) | 4 (12.5) | |
| Spouse job | 0.8 | |||
| Employed | 28 (84.8) | 25 (75.7) | 25 (78.2) | |
| Housewife | - | - | - | |
| Retired | 5 (15.2) | 8 (24.3) | 7 (21.8) | |
| Education | 0.5 | |||
| Primary | 6 (18.2) | 3 (9.1) | 4 (12.5) | |
| Secondary | 24 (72.7) | 24 (72.7) | 22 (68.8) | |
| Higher education | 3 (9.1) | 6 (18.2) | 6 (18.7) | |
| Spouse education | 0.83 | |||
| Primary | 3 (9.1) | 4 (12.1) | 4 (12.6) | |
| Secondary | 16 (48.5) | 18 (54.6) | 14 (43.7) | |
| Higher education | 14 (42.4) | 11 (33.3) | 14 (43.7) | |
| Family groom sponsorship | ||||
| Enough | 17 (51.5) | 14 (42.5) | 16 (50) | 0.53 |
| Less than enough | 11 (33.3) | 10 (30.3) | 10 (31.2) | |
| More than enough | 5 (15.2) | 9 (27.2) | 6 (18.8) | |
| Gravida | 0.83 | |||
| 1 | 4 (12.2) | 1 (3.0) | 2 (6.2) | |
| 2 | 16 (48.5) | 23 (69.7) | 21 (65.7) | |
| 3 | 11 (33.3) | 8 (24.3) | 9 (28.1) | |
| 4 | 1 (3.0) | 1 (3.0) | - | |
| 5 | 1 (3.0) | - | - | |
| Parity | 0.93 | |||
| 1 | 4 (12.2) | 1 (3.0) | 2 (6.2) | |
| 2 | 19 (57.6) | 26 (78.8) | 23 (71.9) | |
| 3 | 9 (27.2) | 6 (18.2) | 7 (21.9) | |
| 4 | 1 (3.0) | - | - | |
| Abortion | 0.83 | |||
| 0 | 30 (91.0) | 30 (91.0) | 30 (93.8) | |
| 1 | 2 (6.0) | 2 (6.0) | 2 (6.2) | |
| 2 | - | 1 (3.0) | - | |
| 3 | 1 (3.0) | - | - |
Demographic Profile of Vitex, Cinnamon, and Placebo a
After intervention (two and three months later), the overall score of sexual function increased significantly in the vitex and cinnamon groups (P = 0.001) according to the subsequent Bonferroni test (Table 3).
| Groups | Vitex | Cinnamon | Placebo |
|---|---|---|---|
| Desire | |||
| Before intervention | 3.56 ± 0.17 | 3.85 ± 0.15 | 3.76 ± 0.15 |
| Two months after intervention | 3.67 ± 0.16 | 3.87 ± 0.15 | 3.78 ± 0.14 |
| Three months after intervention | 3.84 ± 0.17 | 3.92 ± 0.16 | 3.78 ± 0.14 |
| P-value | 0.00 | 0.26 | 0.65 |
| Arousal | |||
| Before intervention | 3.35 ± 0.11 | 2.85 ± 0.14 | 3.12 ± 0.15 |
| Two months after intervention | 3.36 ± 0.10 | 2.84 ± 0.14 | 3.14 ± 0.15 |
| Three months after intervention | 3.47 ± 0.10 | 2.87 ± 0.15 | 3.13 ± 0.15 |
| P-value | 0.02 | 0.40 | 0.53 |
| Lubrication | |||
| Before intervention | 3.52 ± 0.11 | 2.78 ± 0.17 | 3.32 ± 0.16 |
| Two months after intervention | 3.53 ± 0.11 | 3.37 ± 0.15 | 3.35 ± 0.15 |
| Three months after intervention | 3.62 ± 0.11 | 3.63 ± 0.15 | 3.37 ± 0.16 |
| P-value | 0.03 | 0.00 | 0.02 |
| Orgasm | |||
| Before intervention | 3.28 ± 0.15 | 3.27 ± 0.18 | 3.09 ± 0.21 |
| Two months after intervention | 3.28 ± 0.15 | 3.27 ± 0.18 | 3.06 ± 0.21 |
| Three months after intervention | 3.28 ± 0.15 | 3.28 ± 0.18 | 3.09 ± 0.22 |
| P-value | 1.00 | 0.77 | 0.55 |
| Satisfaction | |||
| Before intervention | 3.36 ± 0.14 | 3.66 ± 0.19 | 3.47 ± 0.17 |
| Two months after intervention | 3.35 ± 0.14 | 3.70 ± 0.18 | 3.49 ± 0.17 |
| Three months after intervention | 3.33 ± 0.14 | 3.75 ± 0.19 | 3.47 ± 0.18 |
| P-value | 0.60 | 0.03 | 0.56 |
| Pain | |||
| Before intervention | 3.98 ± 0.14 | 3.07 ± 0.20 | 3.74 ± 0.14 |
| Two months after intervention | 4.01 ± 0.14 | 3.22 ± 0.18 | 3.78 ± 0.14 |
| Three months after intervention | 4.04 ± 0.14 | 3.31 ± 0.18 | 3.75 ± 0.15 |
| P-value | 0.13 | 0.07 | 0.44 |
| Overall | |||
| Before intervention | 21.03 ± 0.41 | 19.51 ± 0.71 | 20.54 ± 0.59 |
| Two months after intervention | 21.20 ± 0.39 | 20.33 ± 0.65 | 20.63 ± 0.59 |
| Three months after intervention | 21.60 ± 0.39 | 20.81 ± 0.64 | 20.62 ± 0.59 |
| P-value | 0.00 | 0.00 | 0.41 |
Mean Scores of Sexual Function Domains in Vitex, Cinnamon, and Placebo Groups Before and After Treatment
The sexual desire score after the intervention increased in the vitex group compared to before the intervention (P = 0.00).
The increased score of lubrication was generally significant for the vitex (P = 0.03), cinnamon (P = 0.001)), and placebo (P = 0.02) groups, while their subsequent test showed significance only for the cinnamon group after two and three months compared to before the intervention.
The sexual satisfaction score increased for the cinnamon plant (P = 0.03), but the subsequent test showed that it was insignificant in any period.
There were no statistically significant differences in orgasm scores and pain during sexual intercourse between the vitex, cinnamon, and placebo recipients over time (P > 0.05).
Also, the difference between the three groups is significant only in terms of lubrication, arousal, and pain (Tables 3 and 4).
| Domains Groups | Desire | Arousal | Lubrication | Orgasm | Satisfaction | Pain | Overall |
|---|---|---|---|---|---|---|---|
| One-way ANOVA | |||||||
| Vitex | 0.00* | 0.02* | 0.03* | > 0.99 | 0.60 | 0.13 | 0.00* |
| Cinnamon | 0.26 | 0.40 | < 0.00* | 0.77 | 0.03* | 0.07 | < 0.00* |
| Placebo | 0.65 | 0.53 | 0.02 | 0.55 | 0.55 | 0.44 | 0.41 |
| Two-way ANOVA | 0.50 | 0.02 | 0.04 | 0.74 | 0.16 | 0.00 | 0.45 |
| Bonferroni test | |||||||
| Vitex | |||||||
| Before vs. 2 m later | 0.16 | 1.00 | 0.00* | 0.97 | - | - | 0.00* |
| Before vs. 3 m later | 0.00 | 1.00 | 0.00* | 1.00 | - | - | 0.00* |
| 2 m vs. 3 m later | 0.01* | 0.63 | 0.02* | 1.00 | - | - | 0.00* |
| Cinnamon | |||||||
| Before vs. 2 m later | 0.97 | 1.00 | 1.00 | 0.481 | - | - | 0.05* |
| Before vs. 3 m later | 0.63 | 0.11 | 0.11 | 0.09 | - | - | 0.00* |
| 2 m vs. 3 m later | 0.97 | 0.08 | 0.09 | 0.31 | - | - | 0.00* |
| Placebo | |||||||
| Before vs. 2 m later | 0.97 | 0.97 | 0.97 | 0.97 | - | - | 0.97 |
| Before vs. 3 m later | 1.00 | 1.00 | 0.97 | 1.00 | - | - | 1.00 |
| 2 m vs. 3 m later | 1.00 | 0.97 | 0.60 | 0.97 | - | - | 0.97 |
The Results of One-way ANOVA, Two-way ANOVA, and Bonferroni Test in Vitex, Cinnamon, and Placebo Groups a
5. Discussion
Some notable strengths of this study include using the random assignment method, blinding method, and careful phone call follow-up until two and three months after the intervention.
According to the presented data, cinnamon improved sexual function after three months. In this regard, the study by Safavi et al. showed that the total score of sexual function in women of reproductive age increased after two months of cinnamon drops (23). There is no study about the effect of cinnamon on sexual function, so it was impractical to review our result and compare it to other studies. Nevertheless, few studies, including the study by Kianitalaei et al. in 2020, showed that alcea benefits the sexual function of postmenopausal women (24). Also, in Malakouti et al.'s study, inhalation aromatherapy with a combination of lavender, fennel, geranium, and red rose improved the sexual function of postmenopausal women (25). According to the results of these studies, it can be decided that medicinal plants can generally be effective for the sexual function of postmenopausal women.
Lubrication and sexual satisfaction scores increased in the cinnamon group, while a study by Safavi et al. in 2018 also showed that two months of cinnamon drops increased lubrication and sexual satisfaction in women of childbearing age (23). Also, in the study by Taavoni and Haghani in 2014, the results showed that aphrodite improved the sexual satisfaction of postmenopausal women, which was also statistically significant (26).
In the present study, other areas of sexual function for the cinnamon and placebo groups, namely sexual desire, orgasm, arousal, and intercourse pain, did not improve significantly. One study showed that aphrodite improved sexual desire and orgasm in postmenopausal women after four weeks of intervention (27). Also, a study by Safavi et al. in 2018 showed that rose, ginger, and cinnamon drops improved sexual desire, orgasm, arousal, and intercourse pain in women of childbearing age (23). According to the results obtained in the present study and the research mentioned above, it can be concluded that cinnamon generally improves sexual function. The different results observed for each domain could be due to differences in sample size, instruments to measure sexual function, prescribed doses of drugs, drug preparation methods, or target groups.
Vitex can improve sexual function after three months. In this regard, Sadeghi et al. showed that vitex improves sexual function in postmenopausal women (28). Mazaro-Costa also stated that plants such as vitex, fennel, ginkgo, Tribulus terrestris, red clover, black cohosh, Angelica archangelica, hops, and ginseng, according to a search in the PubMed database, have the greatest impact on the reproductive system of menopausal women and improve sexual function (8). Contrary to the results of our study, van Die et al. showed that after 16 weeks of consuming vitex, the sexual function of postmenopausal women did not improve (29). Also, Naseri et al. could not obtain any significant improvement in the sexual function of postmenopausal women after eight weeks of vitex consumption (30).
However, it should be noted that the tools used in these two studies are different from the present study. In the study by van Die et al. (29), vitex tablets were used for the intervention, and in the study by Naseri et al., the sample size (26 in each group) and the dose used for the intervention (30 mg of vitex) were less than in the present study. As a result, due to the lack of sufficient studies and contradictory results, it is not possible to comment definitively on the effectiveness of vitex on the sexual function of postmenopausal women.
The sexual desire and arousal domains in the vitex group were the only domains that showed significant improvement. Similarly, a 2002 study by Lucks et al. found that vitex oil improved sexual desire in postmenopausal women (31). These results are also evident in a 2005 study by Smolinski et al., in which sexual desire improved in postmenopausal women 16 weeks after consuming vitex (32). Another study by Heirati et al. showed that the difference between the vitex and placebo groups was not significant in any domain, but there was a significant difference in the overall sexual function mean score, so the intervention group had a higher score than the placebo group after 16 weeks (P < 0.05) (33).
Side effects included headache in two participants and depressive symptoms in one participant of the vitex group, and stomachache in the cinnamon (two participants) and placebo (two participants) groups. Also, two participants in the cinnamon group stated that taking the capsules caused vaginal spotting, but they did not stop taking the capsules. Participants with side effects were referred to a health center physician and psychologist.
Different side effects reported in studies on cinnamon and vitex can be due to differences in drug preparation, target groups, intervention doses, consumption methods, duration of use, and research methods.
Like Farahmand and Ramezani Tehrani's study, this study showed that appropriate plants could effectively treat sexual disorders; however, more studies in this field are needed (34).
There were also limitations to this research, including the fact that the subjects avoided expressing sexual problems or unusual sexual relations due to cultural reasons and the subject's sensitivity. Subjects were assured that the completed questionnaires and their information would remain confidential. Stress and anxiety of subjects while taking the capsules due to COVID-19 and the subsequent negative impact on study results was another limitation of this study.
5.1. Conclusions
Cinnamon and vitex improved sexual function in menopausal women. More studies in this field may be conducted to introduce them as an appropriate herbal remedy for older women.