1. Context
Sexual dysfunction refers to dissatisfaction with sexual function leading to distress (1). According to the Diagnostic and Statistical Manual of Mental Disorders (DSM), female sexual dysfunction (FSD) includes sexual desire/arousal, orgasm, and genito-pelvic pain/penetration disorders (2). These disorders root in vascular, nervous, hormonal, or psychological causes (3). Forty-one percent of women of reproductive age worldwide mention sexual dysfunction as a common medical problem (4). There is a powerful link between sexual dysfunction and quality of life, known as a common health problem all over the world (5). Sexual dysfunction can have devastating effects on women’s self-respect, a sense of being total and complete, and interactive relationships while also contributing to mental disorders. FSD can cause conflicts and ultimately lead to divorce or negative effects on fertility (6). Women's sexual life and fertility are strongly affected by their sexual disorders, while various biological, psychological, and social factors contribute to the prevalence of sexual disorders. Persistently notable risk factors for sexual dysfunction include disability, mental disorders, tension, miscarriage, urogenital problems, female genital mutilation, miserable relationship, and sexual harassment and rape (7).
Many treatments, including chemical drugs, have been investigated to improve FSD. However, complementary medicine has been proposed as an appropriate alternative for improving sexual function disorders due to concerns about the side effects of chemical drugs (8). Hence, many affected individuals often seek alternative treatments, such as herbal medicines, despite developing new drug therapies for sexual dysfunction (3). The mechanism of action of these medicines is not fully known; however, according to recent research, the medicinal substances in these herbs can enhance sexual function by affecting the brain, endocrine system, and gonads. Herbal medicines also have antioxidant and anti-inflammatory properties that may improve sexual function (9). However, there is no effective herbal or even chemical treatment approved by the US Food and Drug Administration (FDA) for FSD so far, or the therapeutic effects have been limited to placebo and trial and error. Accordingly, new studies continue to prove the medical efficacy of herbs and find effective herbal remedies (10).
2. Objectives
Chemical medicines have many side effects. If the effects of herbal medicines on the improvement of female sexual function and sexual satisfaction are investigated and confirmed, these medicines can replace chemical medicines. Therefore, considering the high outbreak of FSD among women of reproductive age and the tendency of the affected individuals to use complementary medicine, this systematic review aims to investigate the effects of herbal medicines on sexual function and sexual satisfaction of women of reproductive age.
3. Data Sources
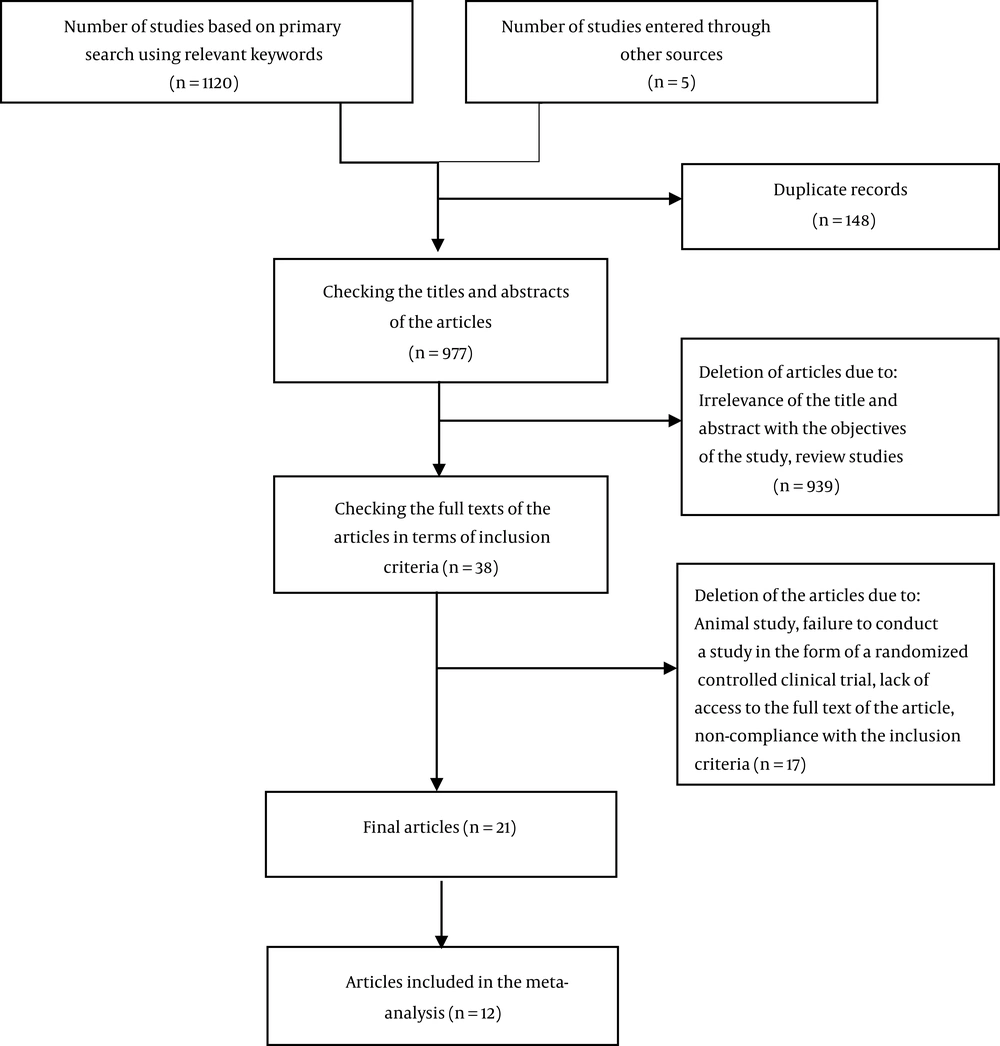
The research population of the current systematic review included all randomized clinical trial studies on the effects of herbal medicines on sexual function and sexual satisfaction of women of reproductive age. The researchers searched the international databases of Google Scholar, Web of Science, Scopus, Science Direct, PubMed, Cochrane Library, and the national SID database. A manual search was also carried out to find the articles that could not be retrieved in the electronic search. This study examined only English or Persian language articles. All relevant articles published from 2000 to February 28, 2022, were reviewed by two independent researchers. The keywords of "sexual function, sexual dysfunction, sexual health, sexual disorders, sexual disorder, sexual satisfaction, herbal medicine, herbal treatment, herb, women, and female" were selected using the MeSH tool to find related articles in the databases, combined with Boolean operators of OR and AND. The search in the mentioned databases resulted in the retrieval of 1120 articles, which were then entered into EndNote software. Accordingly, 148 duplicate articles were identified and removed using EndNote software, followed by the examination of the titles and abstracts of 977 articles. Of the remaining articles, 939 were removed because they were not related to the objectives of the present study, after which the full texts of the remaining 38 articles were studied. The corresponding author was contacted and asked to provide the article’s full file when it was not available online. A manual search was also performed in related articles to obtain a bigger sample. Finally, 21 articles were included in the study (Figure 1) after reviewing the inclusion criteria, and their quality was evaluated by two independent authors using Verhagen’s checklist.
4. Study Selection
The inclusion criteria included randomized controlled clinical trial studies published in English or Persian on a sample of women aged 15 - 51 years without depression investigating sexual function or sexual satisfaction in which the control group had received herbal medicines. Papers whose full texts were not available, observational, qualitative, and review studies, article abstracts, and letters to the editor were excluded.
5. Data Extraction
A researcher-made form was used to extract data from the texts of the selected articles. The form included details such as the author’s name, publication year, research location, study design, sample size, participants’ age, intervention type, side effects, data collection tools, findings, and results of evaluating the quality of the article.
5.1. Evaluating the Quality of the Articles
The quality of the articles was evaluated using Verhagen's checklist, designed to measure the quality of randomized clinical trial studies. The instrument consists of eight items to examine the randomization method and latent allocation, similarity of prognostic factors at baseline, specification of eligibility criteria, blinding of evaluators, providers, and participants, presentation of point estimates for outcome measures, and intention-to-treat analysis. For each question, the “Yes/No” and “No Idea” answers were given 1 and 0 points, respectively (11). Articles with a score of ≥ 3 were included in the study.
6. Results
According to the research objectives, this study examined all published articles in electronic databases. A total number of 1120 articles (Google Scholar = 737; Cochrane Library = 37; Web of Science = 23; Scopus = 169; Science Direct = 112; PubMed = 24; SID = 18) were extracted through primary search using relevant keywords. Finally, 21 articles with a total sample size of 1625 were evaluated after the removal of duplicate articles by a review of the titles, abstracts, and then the full texts (Figure 1). Two studies were excluded due to lack of access to the full text, and one study was excluded due to re-reporting results in a new study. All articles were randomized controlled clinical trials published during 2014 - 2022. Among the included studies, only one had a cross-sectional, and others followed a parallel design. Most of the studies were conducted in Iran (17 studies), two in America, and in Bulgaria, Brazil, Australia, India, and South Korea, one study each. In this review, there were four articles on Russian olive, two on chaste tree, two on bindii, two on ginseng, one on carrot seed, one on fenugreek, one on saffron, one on rose flower, one on palm pollen, one on celery seed, one on winter cherry, one on lemon balm, one on pomegranate peel, one on squill bulb, and one on a mixture of oak gall, pomegranate peel, and fenugreek seed. All studies used a placebo control group except for one study in which the control group received no medication. All studies used the female sexual function index (FSFI) (Table 1). A summary of the studies included in the systematic review and the herbs used in the studies is provided in the following.
| Study | Author/Year | Country | Design | Sample Size (Intervention/Control) | Age | Type of Intervention | Control Group | Duration | Side Effects | Questionnaire | Results | Quality Assessment |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Evaluation of the effect of carrot seed (Daucus carota) in women of fertile age with hypoactive sexual desire disorder: A randomized double-blind clinical trial (12) | Sadeghi et al., 2020 | Iran | Randomized double-blind clinical trial, parallel | 30/30 | 18 - 45 | Carrot seed capsule 500 mg, 3 times a day | Placebo | 12 weeks | No adverse effect | FSFI | Compared to the placebo, carrot seed improved the total score of sexual function and domains of desire, lubrication, arousal, satisfaction, orgasm, and pain (P < 0.001). In the intervention group, the total score of sexual function increased from 19.2 ± 4.1 to 27.5 ± 3.6. Sexual satisfaction also increased from 3 ± 1.3 to 4.8 ± 1.1. | 7 |
| 2. The effect of the Vitex agnus-castus plant on the sexual function of women of reproductive age (13) | Dalil Heirati et al. 2020 | Iran | Randomized double-blind clinical trial, parallel | 51/51 | 15 - 44 | 3.2 – 4.8 mg dried extract of Vitex agnus-castus, once a day | Placebo | 4 weeks | Nausea (1 sample) | FSFI | There was no statistically significant difference between the two groups in terms of the total score of sexual function and its domains (P ≥ 0.05), and comparing the scores within the group, only the orgasm domain score improved (P = 0.02). The mean score of the total sexual function was 24.04 ± 6.20 before the intervention and 24.30 ± 6.06 after the intervention. The mean difference before and after the intervention in the vitagnus group was -0.25 ± 1.13. The sexual satisfaction score reached from 4.55 ± 1.25 to 4.60 ± 1.14. The mean difference before and after the intervention was -0.04 ± 0.39. | 7 |
| 3. The 4-month effect of Vitex agnus-castus plant on sexual function of women of reproductive age: A clinical trial (14) | Dalil Heirati et al., 2021 | Iran | Randomized double-blind clinical trial, parallel | 51/51 | 15 - 44 | 3.2 - 4.8 mg dried extract of Vitex agnus-castus, once a day | Placebo | 16 weeks | Nausea (n = 1) | FSFI | The total score of sexual function in the vitagnus group was significantly higher than the placebo group (P < 0.05); however, the difference between the two groups in each domain was not significant (P ≥ 0.05). The total score of sexual function in the intervention group increased from 24.04 ± 6.20 to 26.52 ± 4.70. The sexual satisfaction score reached from 4.55 ± 1.25 to 4.99 ± 0.79. | 7 |
| 4. Effect of herbal composition (Oak Gall, pomegranate peel, and Fenugreek Seeds) on the sexual satisfaction of women at reproductive age (15) | Ghavami et al., 2020 | Iran | Randomized double-blind clinical trial, parallel | 30/30 | 15 - 45 | Vaginal suppository 150 mg herbal composition (oak gall, pomegranate peel, and fenugreek seeds), 1 to 2 hours before the sexual relationship, twice a week | Placebo | 1 month | No adverse effect | FSFI, Larson sexual satisfaction questionnaire | The orgasm domain score was significantly higher in the herbal suppository composition group (P < 0.001), but the two groups had no significant difference in terms of sexual satisfaction (P = 0.14). In the intervention group, the orgasm domain score increased from 2.85 ± 0.92 to 4.80 ± 0.56. The sexual satisfaction score went from 42.20 ± 1.95 to 44.47 ± 1.69. | 7 |
| 5. Comparison of the effect of Elaeagnus angustifolia flower capsule and sildenafil citrate tablet on female sexual interest/arousal disorder in the clinical trial study (16) | Zeinalzadeh et al., 2019 | Iran | Randomized double-blind clinical trial, parallel | G 1: 41, G 2: 42, G 3: 42 | 18 - 40 | Group 1: 4.5 g of Elaeagnus angustifolia flower in two divided doses (2 capsules every 12 hours) for 35 days; Group 2: 50 mg of sildenafil citrate tablets for 4 weeks, one hour before sexual relationship | Group 3: Placebo for 35 days | Group 1 and Group 3: 35 days; Group 2: 4 weeks | - | FSFI | Both interventions were effective in improving sexual interest/arousal (P = 0.007). The score of the sexual desire domain in the Elaeagnus angustifolia flower and sildenafil citrate groups increased from 2.98 ± 0.99 and 3.15 ± 0.94 to 3.79 ± 0.76 and 3.51 ± 0.88, respectively. The frequency of sexual interest/arousal before the intervention was 53.7%, 50%, and 66.7% in the Elaeagnus angustifolia, sildenafil citrate, and control groups, respectively (P = 0.269); however, after the intervention, these values were 19.5%, 33.3%, and 52.4%, respectively (P = 0.007). | 4 |
| 6. Investigation of the effect of Elaeagnus angustifolia flower capsule on sexual satisfaction and levels of androgenic hormones in 18 - 40-year old married women with low sexual desire (17) | Zeinalzadeh et al., 2017 | Iran | Randomized double-blind clinical trial, parallel | 42/42 | 18 - 40 | Elaeagnus angustifolia flower, 4 capsules a day (2 capsules every 12 h) | Placebo | 35 days | - | FSFI, Enrich marital satisfaction questionnaire | Elaeagnus angustifolia significantly reduced the frequency of sexual desire disorder from 53.7% to 19.5% (P = 0.001) but did not improve the levels of sexual satisfaction and androgenic hormones (P > 0.05). (The mean scores of sexual desire and sexual satisfaction were not mentioned). | 3 |
| 7. Efficacy of Tribulus terrestris for the treatment of premenopausal women with hypoactive sexual desire disorder: a randomized, double-blinded, placebo-controlled trial (18) | Vale et al., 2018 | Brazil | Randomized double-blind clinical trial, parallel | 20/20 | 18 - 44 | 750 mg/day (250 mg, 3 pills per day) of Tribulus terrestris | Placebo | 120 days | No adverse effect | FSFI, QS-F | Tribulus terrestris improved the total score of sexual function and the domains of desire, arousal, lubrication, orgasm, pain, and satisfaction. In the intervention group, the total score of sexual function increased from 15.44 to 23.27 (P < 0.001). Sexual satisfaction improved from 3.02 to 4.36 (P = 0.001). | 7 |
| 8. Influence of a Specialized Trigonella foenum-graecum seed Extract (Libifem) on Testosterone, Estradiol and Sexual Function in Healthy Menstruating Women, an RCT with Placebo (19) | Rao et al., 2015 | Australia | Randomized double-blind clinical trial, parallel | 40/40 | 20 - 49 | Libifem capsule 300 mg, twice a day | Placebo | 8 weeks | Exacerbation of migraines (n = 2), indigestion/reflux (n = 2) | 1. FSFI, 2. DISF-SR | Fenugreek seed improved desire and arousal compared to the placebo. A significant change between groups was observed in the arousal domain score (P = 0.026), but no significant change was observed in the total score of FSFI and other domains (mean scores not mentioned). The frequency of sex in the intervention group increased significantly from 1 - 2 times a month to 1 time a week (P = 0.013). A significant rise in the level of free testosterone and estradiol was noted in the intervention group (P < 0.05). | 5 |
| 9. The effect of saffron on sexual dysfunction in women of reproductive age (20) | Rahmati et al., 2017 | Iran | Randomized double-blind clinical trial, parallel | 35 - 34 | 18 - 39 | 15 mg of saffron extract capsule, twice a day | Placebo | 8 weeks | - | FSFI | Saffron significantly improved the total score of sexual function and all its dimensions except moisture and dyspareunia (P < 0.001). After 8 weeks, the frequency of individuals with sexual dysfunction in the intervention group decreased by 34.3%. (Mean scores not mentioned). | 6 |
| 10. The effect of the soft oral capsule of rose oil on sexual dysfunction in women of reproductive age (21) | Motaharinezhad et al., 2021 | Iran | Randomized triple-blind clinical trial, parallel | 37/35 | 15 - 49 | 2 soft capsules containing 15 mg of rose oil daily | Placebo | 8 weeks | No adverse effect | 1. FSFI, 2. BDI | The difference in the mean total score of sexual function between the case and control groups at the end of the eighth week was statistically significant (P < 0.001). The mean score of sexual function in the Rose oil group improved significantly from 20.90 ± 3.34 to 26.7 ± 5.13 (P < 0.001). The mean score of sexual satisfaction in the intervening group improved from 3.70 ± 0.93 to 4.65 ± 0.95 (P < 0.001). | 8 |
| 11. The effect of date palm on sexual function in infertile couples: a double-blind controlled clinical trial (22) | Jahromi et al., 2022 | Iran | Randomized double-blind clinical trial, parallel | 64/64 | 15 - 49 | Date palm pollen capsule 300 mg, once a day | Placebo | 30 days | No adverse effect | FSFI | The total score of sexual function in the intervention group significantly increased from 21.06 ± 2.58 to 27.31 ± 2.59 in the intervention group (P < 0.0001). Also, the score of other domains (arousal, orgasm, lubrication, pain during intercourse, satisfaction) in the intervention group increased significantly compared to the control group, which was statistically significant (P < 0.0001). The sexual satisfaction score in the intervention group improved from 4.49 ± 0.61 to 5.46 ± 0.67 (P < 0.0001). | 8 |
| 12. The effect of Elaeagnus angustifolia flower essence inhalation on dyspareunia and sexual satisfaction of women at reproductive age: A randomized clinical trial (23) | Jafari et al., 2021 | Iran | Randomized clinical trial, parallel | G 1: 30, G 2: 31, G 3: 33 | 18 - 45 | Group 1: Elaeagnus angustifolia flower essence inhalation 3 times a day for 20 minutes each time for 4 weeks; Group 2: Elaeagnus angustifolia flower essence once only 20 minutes before intercourse as inhalation | Group 3: No intervention | 4 weeks | No adverse effect | FSFI | The mean scores of pain (P = 0.004) and sexual satisfaction (P < 0.001) had a statistically significant difference in the three groups. However, the mean scores of pain and sexual satisfaction increased significantly only in intervention group 2. The mean score of sexual pain in the first intervention group, the second intervention group, and the control group were 4.0 ± 3.8, 4.0 ± 2.9, 4.0 ± 0.8 before the intervention, and 4.0 ± 3.8, 4.0 ± 7.7 and 4.0 ± 0.8 after the intervention, respectively. Sexual pain significantly improved only in the second intervention group (P < 0.05). The mean score of sexual satisfaction in the first intervention group, the second intervention group, and the control group were 4.0 ± 1.7, 4.0 ± 2.7, 3.0 ± 8.5 before the intervention, and 4.0 ± 2.7, 4.7 ± 0.9 and 3.8 ± 0.5 after the intervention, respectively. Based on the results of the intragroup test, sexual satisfaction increased significantly only in the second intervention group (P < 0.001). | 4 |
| 13. Treatment of women’s sexual dysfunction using Apium graveolens L. Fruit (celery seed): A double-blind, randomized, placebo-controlled clinical trial (24) | Hessami et al., 2021 | Iran | Randomized double-blind clinical trial, parallel | 40/40 | 18 - 44 | 500 mg of celery seed 3 times a day | Placebo | 6 weeks | No adverse effect | FSFI | The improvement of the total sexual function score in the intervention group was significantly higher than the placebo group (P < 0.001) and increased in the intervention group from 14.72 ± 2.88 to 23.02 ± 3.10; this increase is mainly due to the improvement of sexual desire, arousal, lubrication, and pain. The sexual satisfaction score in the intervention group increased from 3.08 ± 1.42 to 3.50 ± 1.47, and no statistically significant difference was observed between the two groups (P = 0.281). | 8 |
| 14. Vitamin E and ginseng supplementation to enhance female sexual function: a randomized, double-blind, placebo-controlled, clinical Trial (25) | Ghamari et al., 2020 | Iran | Randomized double-blind clinical trial, parallel | 31/31 | 18 - 45 | Vitamin E and ginseng supplement (100 IU vitamin E, 67 mg Korean ginseng, and 40 mg Siberian ginseng) 1 tablet a day | Placebo | 6 weeks | Undesirable effects in groups were of no clinical concern. | FSFI | Changes in the total score of sexual function and its domains in each group were significant (both P < 0.001), but there was no statistically significant difference between the two groups (P = 0.153). In the intervention group, the total score of sexual function increased from 13.87 ± 2.76 to 22.40. The supplement only improved the domains of desire (P = 0.030) and satisfaction (P = 0.028) compared to the placebo, and the satisfaction score in the intervention group increased from 1.97 ± 0.88 to 3.89. There was no notable difference between the treatment groups regarding the scores of other domains. | 8 |
| 15. Efficacy and Safety of Ashwagandha (Withaniasomnifera) Root Extract in Improving Sexual Function in Women (26) | Dongre et al., 2015 | India | Randomized double-blind clinical trial, parallel | 25/25 | 21 - 50 | Ashwagandha root extract capsule, 300 mg, twice a day | Placebo | 8 weeks | No adverse effect | FSFI, FSDS, SAR | Compared to the placebo, Winter cherry root significantly improved the total score of sexual function (P < 0.001) and the scores of arousal (P < 0.001), lubrication (P < 0.001), orgasm (P = 0.004), satisfaction (P < 0.001), the FSDS (P < 0.001) and the number of successful sexual encounters (P < 0.001). In the intervention group, the total sexual satisfaction score increased from 13.63 to 23.86, and the sexual satisfaction domain score increased from 2.35 to 3.79. | 6 |
| 16. Effect of Melissa officinalis (Lemon balm) on Sexual Dysfunction in Women (27) | Darvish-Mofrad-Kashani et al., 2018 | Iran | Randomized double-blind clinical trial, parallel | 22/21 | 18 - 50 | 500 mg of aqueous extract of M. officinalis twice a day | Placebo | 4 weeks | No serious side effects (diarrhea 4.5% and constipation 4.5%) | FSFI | Increased desire (P < 0.001), arousal (P < 0.001), lubrication (P < 0.005), orgasm (P < 0.001), satisfaction (P < 0.001), pain (P < 0.002), and total sexual function scores (P < 0.001) were significantly higher in the Lemon balm group than in the placebo group. In the intervention group, the total sexual function scores improved from 18.5 ± 4.2 to 27.9 ± 6.0, and the sexual satisfaction score improved from 3.30 ± 0.86 to 5.18 ± 0.77. | 7 |
| 17. The Effect of Korean Red Ginseng on Sexual Function in Premenopausal Women (28) | Chung et al., 2015 | South Korea | Randomized double-blind clinical trial, crossover | 12/11 | 31 - 51 | Korean red ginseng capsule, 1 g, 3 times a day | Placebo | Step 1: 8 weeks,Washout period: 2 weeks; Step 2: 8 weeks | Mild gastric discomfort (n = 1) | FSFI | The mean total score of sexual function increased after treatment with ginseng (from 20.13 ± 2.87 to 23.98 ± 4.10, P = 0.015) and control group (from 20.06 ± 2.64 to 23.78 ± 3.28, P = 0.003); however, this treatment is the same in both groups (P = 0.702). Ginseng significantly improved the domains of desire, arousal, orgasm, and satisfaction; however, there was no therapeutic effect compared to the placebo. Sexual satisfaction in the intervention group improved from 3.40 ± 0.50 to 4.00 ± 0.85 (P = 0.027); there is no change between the two groups (P = 0.894). | 7 |
| 18. Tribulus terrestris for treatment of sexual dysfunction in women (29) | Akhtari et al., 2014 | Iran | Randomized double-blind clinical trial, parallel | 30/30 | Intervention group: 36 ± 6.24; control group: 36.13 ± 5.88 | Terrestris extract 7.5 mg, daily | Placebo | 4 weeks | Grade 1 abdominal cramp (n = 1) | FSFI | Compared to the placebo, Tribulus terrestris significantly improved the total score of sexual function (P < 0.001) and the domains of desire (P < 0.001), arousal (P = 0.037), lubrication (P < 0.001), satisfaction (P < 0.001) and pain (P = 0.041). In the intervention group, the total score of sexual function improved from 22.41 ± 2.87 to 26.80 ± 3.03 and the sexual satisfaction score improved from 3.44 ± 1.15 to 4.61 ± 0.93. | 6 |
| 19. The effect of pomegranate peel gel on orgasm and sexual satisfaction of women in reproductive age: A triple-blind, randomized, controlled clinical trial (30) | Mohammadzadeh et al., 2019 | Iran | Randomized triple-blind clinical trial, parallel | 49/49 | 18 - 45 | Pomegranate peel vaginal gel 1 applicator, 15 minutes before sexual relationship, three times a week | Placebo | 8 weeks | The itching was similar in both groups | FSFI | The mean scores of orgasm and sexual satisfaction in the intervention group, compared to the placebo group, showed a statistically significant increase (P < 0.001). The sexual satisfaction score in the intervention group improved from 3.92 ± 0.91 to 5.33 ± 0.70, which was statistically significant (P < 0.001). | 8 |
| 20. Comparison of Elaeagnus angustifolia Extract and Sildenafil Citrate on female orgasmic disorders (31) | Akbarzadeh et al., 2014 | Iran | Randomized clinical trial, parallel | G 1: 41, G 2: 42, G 3: 42 | 18 - 40 | Group 1: 4.5 g of E. angustifolia extract in two divided doses for thirty-five days; Group 2: 50 mg of sildenafil citrate tablets for 4 weeks 1 hour before sexual relationship | Group 3: Placebo in similar packages to E. angustifolia capsules | 35 days | - | FSFI | Both E. angustifolia extract and sildenafil citrate effectively reduced the frequency of orgasmic disorders in women (P = 0.004). The orgasm score in the group of E. angustifolia and sildenafil was 3.31 ± 1.0 before the intervention and 3.48 ± 0.94 after the intervention, respectively, and increased to 4.03 ± 1.01 and 4.15 ± 0.89. There was a significant difference between the two groups in terms of sexual satisfaction after the intervention (P = 0.03) compared to the beginning of the study, and both interventions caused a significant improvement in sexual satisfaction. The sexual satisfaction score in the group of E. angustifolia and sildenafil before the intervention was 3.82 ± 1.31 and 4.25 ± 0.8, respectively, and increased to 4.75 ± 1.2 and 4.73 ± 0.78 after the intervention. | 4 |
| 21. Effect of Squill on the sexual function among women of reproductive age (32) | Abbasi Pirouz et al., 2018 | Iran | Randomized double-blind clinical trial, parallel | 30/30 | 15 - 45 | 0.5 cc of squill oil, 5 minutes before sexual relationship topically on the clitoris, 1 to 3 times a week | Placebo | 4 weeks | No adverse effect | FSFI | Squill oil improved the total score of sexual function and the domains of desire, lubrication, orgasm, pain, and arousal compared to the placebo (P < 0.001). The total score of sexual function in the intervention group improved from 8.8 ± 0.7 to 33.2 ± 4.4. | 7 |
Abbreviations: FSFI, female sexual function index; FSDS, Female Sexual Distress Scale; SAR, sexual activity record; BDI, beck depression inventory; DISF-SR, derogatis interview for sexual function-self report; QS-F, Sexual Quotient Female Questionnaire.
6.1. Carrot Seed (Daucus carota)
In Sadeghi et al.’s (2020) study, carrot seed improved the total scores of sexual function (7.329 ± 0.830, P < 0.001), desire (4.1 ± 0.7, P < 0.001), moisture (4.7 ± 0.8, P = 0.019), arousal (0.8 ± 4.1, P < 0.001), satisfaction (1.1 ± 4.8, P < 0.001), orgasm (0.9 ± 3.9, P < 0.001), and pain (1 ± 5.4, P = 0.001) (12).
6.2. Chaste Tree (Vitex agnus-castus)
According to Dalil Heirati et al.’s (2020) study, there was no statistically important difference between the two groups in terms of the total mean scores of sexual function and its dimensions after one month of intervention (P ≥ 0.05). Only the score of orgasm showed an improvement in the comparison of intragroup scores (P = 0.02) (13). The results of another study by Dalil Heirati et al. (2021) showed no significant differences between the dimensions of sexual function after 16 weeks of intervention. However, there was a statistically significant difference in the total score of sexual function, according to which the vitagnus group had a higher score than the placebo after two months (P < 0.05) (14).
6.3. The Herbal Composition of Oak Gall (Quercus infectoria), Pomegranate Peel (Punica granatum L.), and Fenugreek Seeds (Trigonella foenum-graecum)
As shown by Ghavami et al. (2020), the orgasm dimension scores were significantly higher in the group taking herbal composition compared to the control group (P < 0.001); however, the two groups are the same in terms of sexual satisfaction (P = 0.14) (15).
6.4. Russian Olive (Elaeagnus angustifolia)
There were four studies on the Russian olive. In Zeinalzadeh et al.’s (2017) study, sexual desire disorder dropped significantly from 53.7 to 19.5 after the intervention (P = 0.001). However, there were no significant differences between the two groups in terms of sexual satisfaction score (0.89 vs. 0.96) and mean androgenic levels pre- and post-intervention (P > 0.05) (17). In another study by Zeinalzadeh et al. (2019), the number of sexual urge/excitement was 53.7%, 50%, and 66.7% in the Russian olive, sildenafil citrate, and control groups, respectively, before the intervention (P = 0.269), but these values were 19.5%, 33.3%, and 52.4%, respectively, after the intervention (P = 0.007). Therefore, Russian olive and sildenafil citrate were effective in improving sexual desire/arousal (16). As shown by Jafari et al. (2021), the mean sexual pain score was 4.3 + 0.8 in the first intervention group, 4.7 + 0.7 in the second intervention group, and 4.0 + 0.8 in the control group post-intervention. The intervention led to a significant increase only in the second intervention group (P < 0.05). The mean score of sexual satisfaction was 4.2 + 0.7 in the first intervention group, 4.7 + 0.9 in the second intervention group, and 3.8 + 0.5 in the control group. According to the results of the intragroup test, the intervention led to a significant difference only in the second intervention grouping (P < 0.001) (23). In a study by Akbarzadeh et al. (2019), the frequency of orgasm disorder was 41.5%, 40.5%, and 57.1% in the Russian olive, sildenafil citrate, and control groups before the intervention (P = 0.23), but these values were 29.3%, 16.7%, and 50%, respectively, post-intervention (P = 0.004). Sexual satisfaction was significantly different post-intervention compared to pre-intervention between the two groups (P = 0.003). Also, the greatest decrease in changes after the intervention (58.82%) was detected in the sildenafil citrate group. According to these findings, the extracts of Russian olive and sildenafil citrate both effectively reduced the frequency of orgasm disorders in women (31).
6.5. Bindii (Tribulus terrestris)
According to Vale et al.’s (2018) study, the total scores of sexual function (P < 0.001) and the dimensions of desire (P < 0.001), sexual awakening (P = 0.005), moisture (P = 0.001), orgasm (P < 0.001), painful sex (P = 0.030), and sexual pleasure (P = 0.001) improved in the group treated with bindii, while placebo treatment did not improve the moisture and pain scores. According to the Sexual Quotient Female Questionnaire (QS-F) scores, patients who used bindii experienced an improvement in terms of sexual desire (P = 0.012), arousal/moisture (P = 0.002), pain (P = 0.031), orgasm (P = 0.004), and satisfaction (P = 0.001), while women receiving placebo treatment showed no improvement. The levels of free (P = 0.046) and bioavailable (P < 0.048) testosterone increased in women who received bindii (18). Akhtari et al.’s (2014) study revealed that the patients of the bindii group had a significant improvement in the total scores of sexual function (P < 0.001) and the dimensions of desire (P < 0.001), arousal (P < 0.037), moisture (P < 0.001), satisfaction (P < 0.001), and pain (P < 0.041) at the end of the fourth week (29).
6.6. Fenugreek (Trigonella foenum-graecum Seed or Libifem)
Rao et al. (2015) found a considerable rise in free testosterone (P = 0.043), estradiol (P = 0.013), and desire and arousal (P = 0.026) in the intervening group. Also, the intervention group reported a significantly higher frequency of intercourse compared to the placebo (P = 0.013) after two months of intervention. According to their results, fenugreek extract may be a therapeutic item to increase women’s arousal and desire (19).
6.7. Saffron or Colchicum autumnale (Saffron crocus)
Rahmati et al. (2017) compared two intervention and control groups four weeks after the start of the intervention and found a significant difference between their excitement and sexual desire (P < 0.05). However, two months after administrating saffron and placebo, both groups were significantly different in their total scores of sexual function and all its dimensions except moisture (P < 0.05). It was, therefore, concluded that Saffron could improve sexual function and its dimensions in women (20).
6.8. Rose (Rosa damascena)
The findings of Motaharinezhad et al.’s (2021) study showed that the rose oil group significantly improved female sexual function (P < 0.001) two months after the intervention (26.5 ± 7.13) compared to before the intervention (20.90 ± 3.34) and the control group (P = 0.320). The mean scores of sexual function in the two groups were statistically significant (P < 0.001) (21).
6.9. Date Palm Pollen (Phoenix dactylifera L.)
Jahromi et al. (2022) reported that the total score of sexual function significantly increased from 21.06 ± 2.58 to 27.31 ± 2.59 in the intervention group (P < 0.0001). Sexual arousal, orgasm, moisture, dyspareunia, and satisfaction also increased considerably in the intervention group (P < 0.0001) (22).
6.10. Celery Seed (Apium graveolens L. Fruit)
In Hessami et al.’s (2021) study, the improvement in the total score of sexual function was significantly elevated in the celery seed group than in the placebo group at the final week of six weeks of intervention (P < 0.001). The increased total score of sexual function was mainly due to the improvement of sexual urge or desire (P < 0.001), arousal (P < 0.001), moisture (P < 0.001), and painful sex (P = 0.033) at the end of the study (24).
6.11. Korean Ginseng (Panax Ginseng) and Siberian Ginseng (Eleutherococcus senticosus)
Ghamari et al. (2020) showed that the total scores of sexual function and its dimensions changed significantly in both intervention and control groups. However, ginseng and vitamin E supplements (100 units of vitamin E, 67 mg of Korean ginseng, and 40 mg of Siberian ginseng) only improved the domains of desire (P = 0.030) and sexual satisfaction (P = 0.028) (25). In Chung et al.’s (2015) study, the total score of sexual function increased after treatment with Korean red ginseng (from 20.13 ± 2.87 to 23.98 ± 4.10, P = 0.015) and placebo (from 20.06 ± 2.64 to 23.78 ± 3.28, P = 0.003). However, this interchange has not been considered significantly between the two groups (P = 0.702). Medication with Korean red ginseng also improved the dimensions of desire, arousal, orgasm, and satisfaction significantly, while there were no therapeutic effects compared to the placebo (28).
6.12. Winter Cherry (Ashwagandha or Withania somnifera)
Dongre et al. (2015) showed that treatment with winter cherry root extracts significantly improved the total score of sexual function (P < 0.001) and the scores of arousal (P < 0.001), moisture (P < 0.001), orgasm (P = 0.004), satisfaction (P < 0.001), the Female Sexual Distress Scale (FSDS) (P < 0.001) and the number of successful intercourse (P < 0.001) (26).
6.13. Lemon Balm (Melissa officinalis)
Darvish-Mofard-Kashani et al. (2018) reported a statistically significant increase in desire (P < 0.001), arousal (P < 0.001), moisture (P < 0.005), orgasm (P < 0.001), satisfaction (P < 0.001), pain (P < 0.002), and the total score of sexual function (P < 0.001) in the intervention than in the placebo group (27).
6.14. Pomegranate Peel (Punica granatum L.)
In Mohammadzadeh et al.’s (2019) study, there was a statistically significant improvement in the mean scores of the orgasm and sexual satisfaction dimensions in the intervening group than in the placebo group after four and eight weeks (P < 0.001) (30).
6.15. Squill (Drimia maritima)
As shown by Abbasi-Pirouz et al. (2018), squill bulb oil could significantly improve female sexual function in dimensions of desire, moisture, orgasm, and arousal compared to the placebo after one month of administration. (P < 0.0001) (32).
6.16. Meta-Analysis
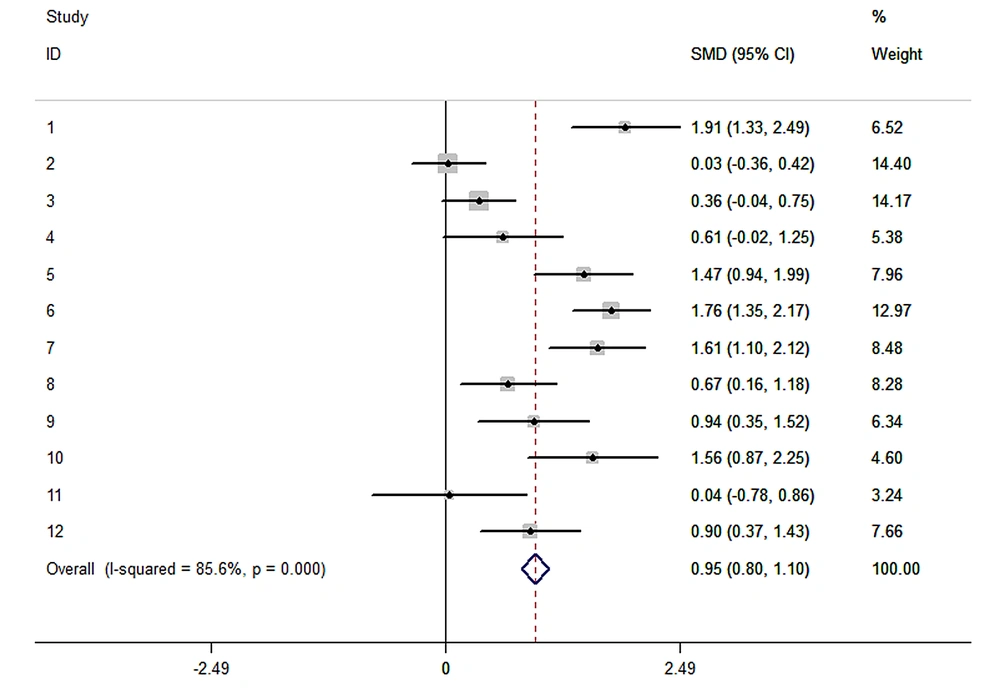
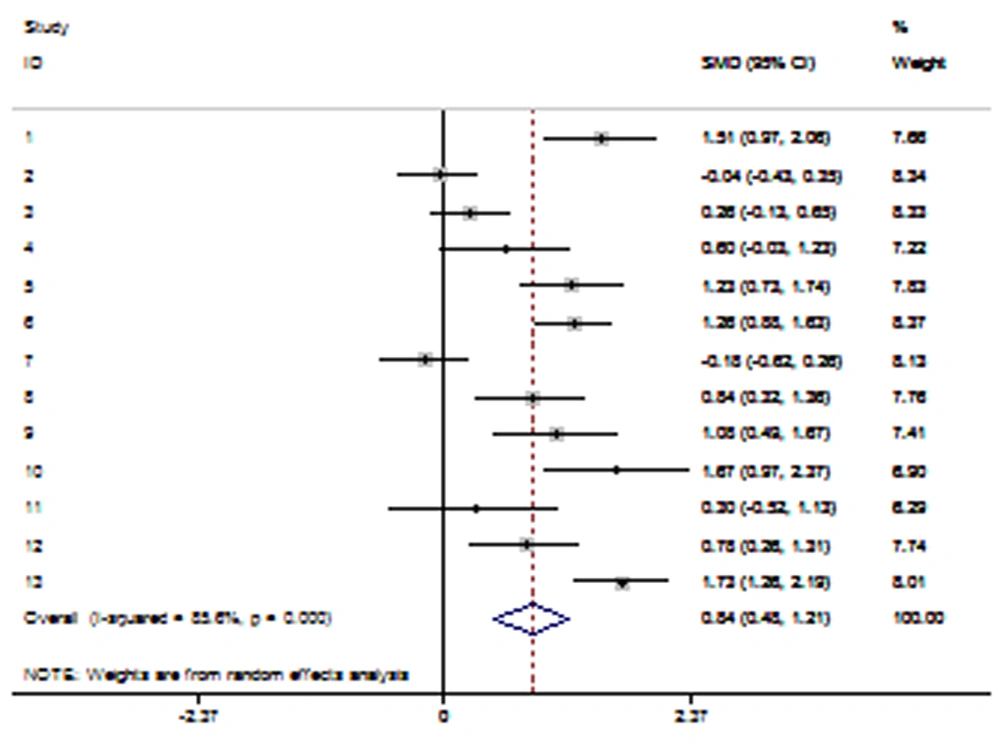
The findings of 12 studies were combined in a meta-analysis. Considering that the I-SQUARED statistic was > 50% (85.6%) in the total score of sexual function, and given the data heterogeneity, the random effect was used instead of the fixed effect to integrate the data. According to the meta-analysis results, the difference in the mean scores of the two groups was 0.95 at a confidence level of 95% (CI: 0.803 - 1.097), which was significant (z = 12.64, P = 0.001) and revealed an improvement in the total score of female sexual function in the intervention group (Figure 2).
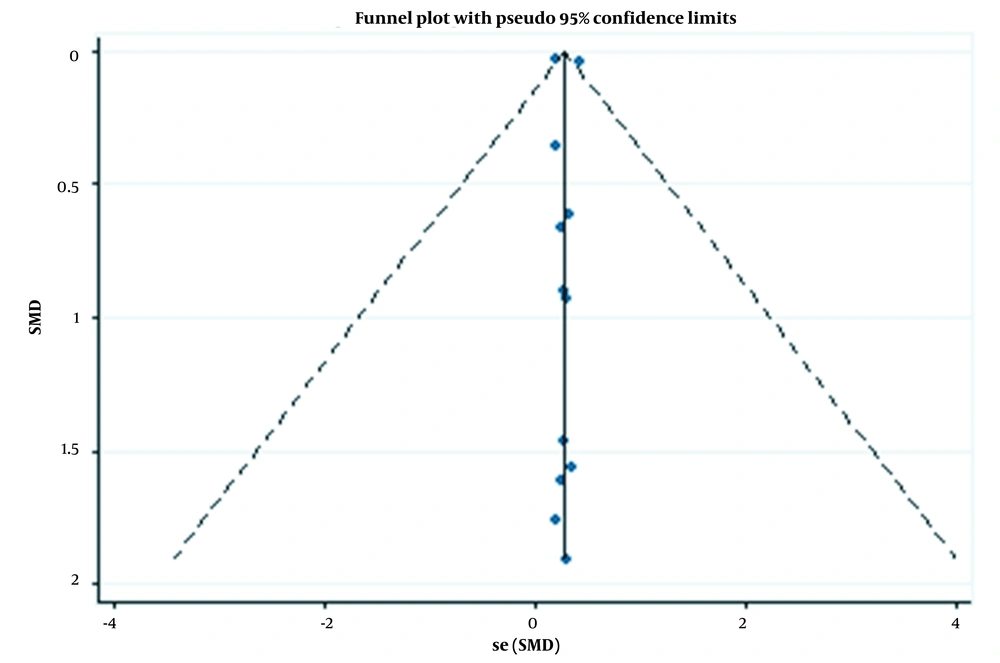
The publication bias was checked using the funnel plot and Begg’s and Egger’s methods (Table 2 and Figure 3). The results of both Begg’s (z = 0.14, P = 0.891) and Egger’s tests showed the absence of the publication bias (t = 0.17, P = 0.867), but the slope of the line was significant (t = 7.25, P = 0.000).
| Std_Eff | Coef | Std. Err | t | P > |t| | [95% Conf. Interval] |
|---|---|---|---|---|---|
| Slope | 0.2741103 | 0.0378233 | 7.25 | 0.000 | 0.1898347 - 0.3583859 |
| Bias | 0.0784932 | 0.4551406 | 0.17 | 0.867 | - 0.9356233 - 1.09261 |
Abbreviation: Std, Standard.
Considering that the I-SQUARED statistic was > 50% (83.2%) in the case of sexual satisfaction, and given the data heterogeneity, the random effect was used instead of the fixed effect to integrate the data. According to the meta-analysis results, the difference in the mean score of the two groups was 0.84 at a confidence level of 95% (CI: 0.476 - 1.21), which was significant (z = 4.5, P = 0.001) and revealed an improvement in the total score of female sexual satisfaction in the intervention group (Figure 4).
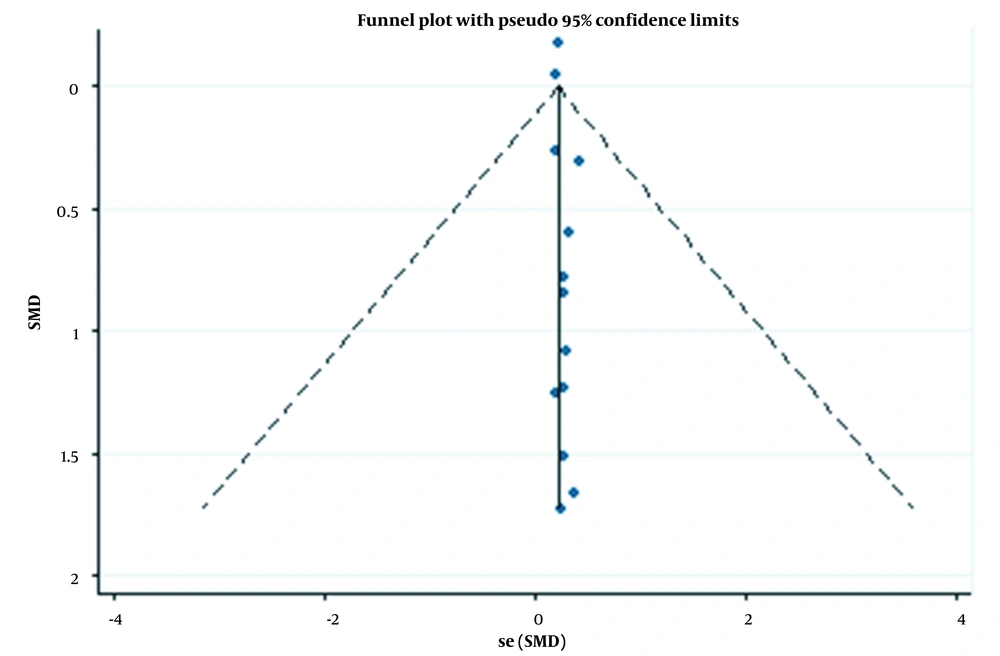
The publication bias was checked using the funnel plot and Begg’s and Egger’s methods (Table 3 and Figure 5). The results of both Begg’s (z = 0.55, P = 0.583) and Egger’s tests showed the absence of the publication bias (t = 0.187, P = 0.089), but the slope of the line was significant (t = 24.96, P = 0.000).
| Std_Eff | Coef | Std. Err | t | P > |t| | [95% Conf. Interval] |
|---|---|---|---|---|---|
| Slope | 0.2067544 | 0.0082847 | 24.96 | 0.000 | 0.1885199 - 0.2249889 |
| Bias | 0.1079386 | 0.0578633 | 1.87 | 0.089 | - 0.0194177 - 0.2352949 |
Abbreviation: Std, Standard.
7. Discussion
Most of the articles included in the present study reported positive effects on the sexual function of women of reproductive age. Also, most studies investigated the side effects of herbal medicines and reported that the side effects were insignificant or there were no side effects. However, this evidence is not conclusive, and more research is required. In addition, few studies have investigated the effects of herbal medicines on sexual function and satisfaction among women of reproductive age, most of which have been conducted in Iran. Thus, it is crucial to do more research with wider and various sample sizes in different regions of the world. The majority of studies were conducted on Russian olive (4 studies), followed by bindii, ginseng, and vitagnus, each with two studies. The findings of the studies conducted on Russian olive showed that it improved some dimensions of sexual function, including desire, arousal, satisfaction, and orgasm in women. Russian olive, vitagnus, palm pollen (13), fenugreek, pomegranate peel (15), etc., are among plants with phytoestrogen properties.
Phytoestrogens are compounds with estrogenic properties found in plants with estrogenic and anti-estrogenic properties. The exact mechanism of the effect of these compounds is not still known, but it seems that phytoestrogens affect the hypothalamus-pituitary axis. As a result, they lead to decreased secretion of follicle-stimulating hormone (FSH) and prolactin, regulated secretion of luteinizing hormone (LH), and increased sex hormones, such as estrogen and androgen, resulting in increased sexual desire, arousal, efficiency, and orgasm (13).
Sha'ari et al.’s (2021) systematic review of the beneficial consequence of natural products on FSD showed that Korean ginseng and bindii significantly and positively affected improving female sexual function. In contrast, other natural products did not improve FSD significantly compared to the placebo (33). This study only included English-language articles, whose samples were all women ≥ 18 years. However, none of the two aforementioned articles reported a significant positive effect of ginseng on the sexual function score of women in the intervention compared to the placebo group. A systematic review by Martimbianco et al. (2020), designed to assess the consequence of bindii on FSD, indicated a significant increase in sexual function scores in premenopausal and postmenopausal women treated with this herb (34). The findings of this study were consistent with the results of the current research.
Jurado et al.’s (2020) systematic review to study the effects of natural products on sexual dysfunction in women of all age groups concluded that despite the low quality of many studies, the large amount of herbal product interventions seemed to upgrade sexual dysfunction, particularly hyposexuality disorders, including the primary and medicine-induced types (35). However, our study examined only women of reproductive age with primary sexual dysfunction.
One limitation of this study was the selection of articles only in English and Persian, which led to excluding non-English or non-Persian articles. In addition, most studies were conducted in Iran, making it difficult to generalize the data to other countries. Among the strengths of the present study was the search in databases by two independent authors and the use of manual in addition to electronic search, which resulted in the retrieval of more articles. Also, there was no limitation to the intervention form used in the selected articles, including oral, inhaled, topical, etc. In this research, all clinical trials used the FSFI, a valid and reliable tool; however, some studies did not clearly explain the randomization and blinding methods. It is suggested to conduct future clinical trials with a better design.
7.1. Conclusions
It seems that herbal medicines positively affect sexual function and satisfaction of women of reproductive age and can be an effective and safe treatment for FSD. However, as there are few clinical trials on each plant and its side effects in this population, more research is required with larger samples of women of reproductive age.