1. Background
Delivery before 37 weeks of gestation is considered preterm birth (PTB), accounting for 5 - 18% of pregnancies worldwide (1). PTB is associated with higher mortality and morbidity rates in neonates (2, 3). Nearly 4 million neonatal deaths occur annually, a quarter of which are due to premature birth (4) and in surviving preterm infants, chronic lung disease, growth delay, hearing impairment, respiratory distress syndrome, intraventricular hemorrhage, growth retardation, necrotizing enterocolitis, perforation, and retinopathy of prematurity are common (5). So, preventing preterm births is crucial and could be prevented with current, cost-effective interventions (6).
The evidence of the complex pathogenesis of preterm birth is still weak, which can explain the limitations of targeted and effective strategies to prevent it (1).
The causes of preterm birth are multifactorial (7). Infections and inflammation in the genital tract will increase PGE2 in amniotic fluid and trigger spontaneous preterm delivery (1, 7, 8).
Garlic has well-documented antimicrobial effects and contains enough dietary fiber (9). Garlic (Allium Sativum) has various compounds, including B vitamins, phosphorus, calcium, potassium, zinc, sulfur, and antioxidants. The sulfur compounds of garlic are the main reason for its pungent smell. Garlic has at least 33 sulfur compounds, such as allein, allicin, allyl propyl disulfide, aminoase enzymes, peroxidase, and 17 amino acids. One of the most important compounds of garlic is allicin (9, 10). Despite considerable effort, no one has detected allicin, alliin, or their metabolites in vivo or in human blood (11). Garlic stimulates selectively fermented compounds in the intestine, thereby balancing and activating the digestive microflora (10).
Previous studies have revealed the role of garlic as an antioxidant, hypotensive mediator, antimicrobial agent, and anti-diabetic drug (12-14).
2. Objectives
As there is little study on garlic's role in preventing preterm delivery, we designed this study to evaluate this garlic role.
3. Methods
The current study was a single-center, prospective, double-blind, randomized, placebo-controlled trial (RCT) conducted at Moheb Yas Hospital (an affiliated hospital of the Tehran University of Medical Sciences) between March 2015 and March 2016.
The Tehran University of Medical Sciences departmental ethics committee approved the research protocol with the number (IR.TUMS.REC.1395.2581). The IRCT registration number of this study is (IRCT 2017011824754N4).
The inclusion criteria were gestational age between 16 - 26 weeks, threatened preterm labor such as previous preterm delivery, surgery, cervical surgery, the history of abortion in the second trimester, bleeding during the first trimester, and multiparty.
Exclusion criteria were uterus anomalies, uterus myoma, mother age less than 18 or more than 40 years, anemia (HB less than 10), diabetes, hypertension, autoimmune diseases, fetal anomalies, preeclampsia, cerclage (cases with previous preterm labor underwent sonography and if they needed cerclage they were excluded).
All participants completed the informed consent form before entering the study. The study's method and the random use of garlic tablets or a placebo were explained to the participants. The authors declare that they have no conflicts of interest.
Randomization was done by an expert nurse via computer random number generation. Patients and physicians were blinded to the patient's group. A secretary gave tablets to the patients, who were blinded to the content of each tablet. Tablets were taken for 10 weeks (26 - 36 weeks). Enrolled cases followed up to delivery.
The enrolled pregnant women were randomly assigned to two groups:
Intervention group: Progesterone Amp (250 mg) + garlic tablet (500 mg)
Group: Progesterone Amp (250 mg) + placebo control
The garlic tablets contain powder (85.42%; equivalent to 8.9-mg allein) (Goldaroo Pharmaceutical Co., Isfahan, Iran). A 250 mg progesterone ampule (Proluton, Shafayab Gostar Company, Iran) was prescribed as an intramuscular injection. Garlic tablets were taken with a meal at the dose of one tablet every 24 hours for 10 weeks, and Progesterone ampule was taken once per week until 36 weeks.
The placebo tablets were produced in the same shape, color, and odor as the garlic tablets.
Patients were followed up regularly by phone calls to ensure adherence to the study protocol.
Also, participants were issued self-report forms to register daily complaints and record medicinal use to ensure the correct use of medication. Participants were reminded to attend the center or contact the researchers if they had problems. The occurrence of preterm birth was the primary outcome of the study (gestational age < 37 weeks).
The incidence of preterm premature rupture of membranes or obstetric complications (Chorio amnionitis, postpartum sepsis, and postpartum hemorrhage) was recorded. The side effects of the prescribed garlic tablets (such as dizziness, constipation, sleepiness, or vaginal dryness) were checked at least once in each of the second and third trimesters.
3.1. Statistical Analyses
Quantitative variables were expressed as frequency and percentage and compared using the chi-square or Fisher exact test with a small sample size. Numerical data were presented as mean and standard deviation. We used the Kolmogorov-Smirnov test to determine the data distribution normality. After that, the relationships of continuous variables with normal distribution were investigated using the independent t student test, and continuous variables without normal distribution were investigated with the non-parametric Mann-Whitney test. Multivariate logistic regression analysis was used to estimate different variables' interaction and confounding effects.
The distribution of variables in this study was normal except for Gravidity, Parity, live birth, and gestational age, which the Mann-Whitney test was used to assess instead of an independent t-test, and then the P-value was extracted. The significance level was considered 0.05 to interpret the relationships among the variables.
Multivariate-Binary regression analysis was used to investigate the true effect of some variables on the study outcome (occurrence of premature birth). It was used to estimate different variables' interaction and confounder effects on the outcome.
4. Results
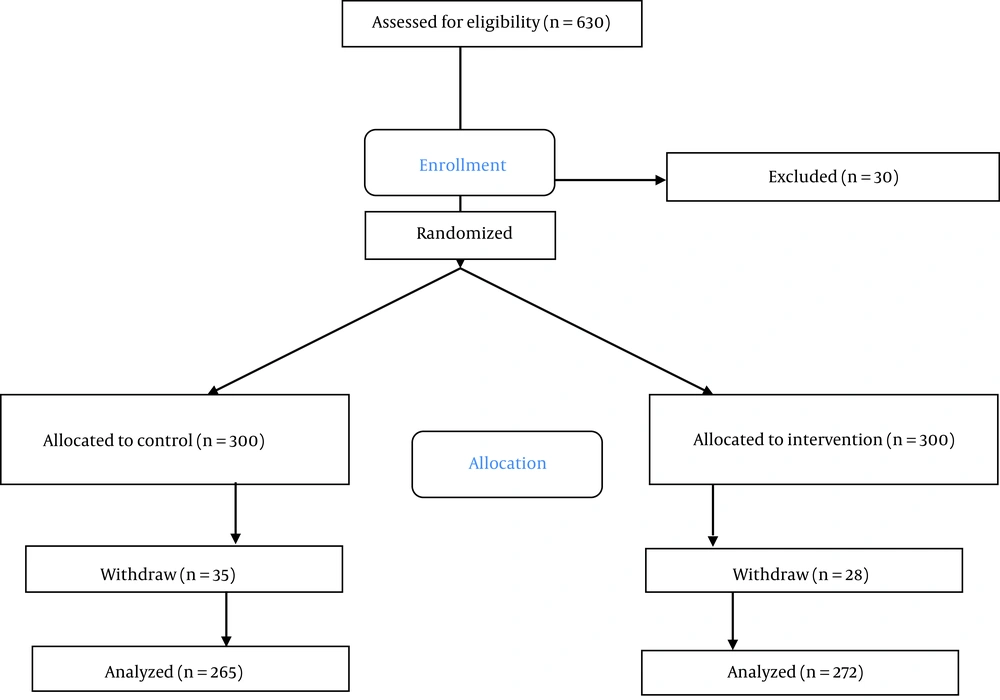
From 630 participants, 30 were excluded from the study due to the need for cerclage. Due to a lack of consent, 28 women from the intervention group and 35 from the control group withdrew from the study. Thus, 537 pregnant women were randomized and started the study (Figure 1).
They were 272 in the intervention group and 265 in the control group. The two matched well for baseline characteristics (Table 1).
| Variables | Intervention Group | Control Group | P-Value |
|---|---|---|---|
| Age (y) | 31.3 ± 5.2 | 31.4 ± 5.1 | 0.84* |
| Gestational age (week) | 23.25 ± 5.2 | 15.09 ± 6.2 | 0.0001+ |
| Gravidity | 2.4 ± 0.9 | 2.5 ± 1.7 | 0.10+ |
| Parity | 0.9 ± 0.7 | 1.2 ± 0.7 | 0.007+ |
| Live birth | 0.9 ± 0.7 | 1.1 ± 0.7 | 0.01+ |
| History of abortion | 0.3 ± 0.7 | 0.5 ± 0.8s | 0.10+ |
| NVD | 80 (29.4) | 49 (19.4) | 0.008** |
| C/S | 192 (70.6) | 204 (80.6) | |
| Age less than 18 years | 1 (0.4) | 0 (0.0) | 0.3** |
| Age more than 40 years | 11 (4) | 12 (5.3) | 0.41** |
| Family history of preterm delivery | 4 (1.5) | 2 (0.9) | 0.52# |
| Previous abdominal surgery | 3 (1.1) | 0 (0.0) | 0.114# |
| High-risk occupation | 3 (1.1) | 2 (0.9) | 0.812# |
| History of bleeding | 130 (47.8) | 48 (21.3) | 0.001** |
| Multiparity | 187 (68.8) | 194 (86.2) | 0.001** |
| Uterus anomaly | 2 (0.7) | 1 (0.4) | 0.667# |
| Myoma | 4 (1.5) | 0 (0.0) | 0.068# |
| History of abortion in the second trimester | 0 (0.0) | 8 (3.6) | 0.002# |
| History of cervical surgery | 1 (0.4) | 2 (0.9) | 0.455# |
| History of anemia | 0 (0.0) | 5 (2.2) | 0.013# |
| History of diabetes | 1 (0.4) | 1 (0.4) | 0.893# |
| History of preterm delivery | 6 (2.2) | 15 (6.7) | 0.014# |
Abbreviations: NVD, normal vaginal delivery; C/s, cesarean section.
a Values are reported as Mean ± standard deviation or number (%).
b P-value refers to student t-test and chi-squared when appropriate.
c Level of significance P < 0.0001+, P < 0.001**, P < 0.01# with respect to control.
d **Chi-square test, #Fisher exact, * independent t student test, + Mann-Whitney test.
The participants were between 25 and 37 years old. Descriptive statistics in Table 1 show that the general characteristics of both groups were similar (P > 0.05).
The rates of C/S and history of preterm labor were statistically higher in the control group (Table 1).
No women developed diabetes or preeclampsia during pregnancy in both groups. The mean number of parity, live birth, and abortion significantly differed between the intervention and control groups (Table 1).
All participants were followed up until the labor time. Seventeen participants in the intervention group (6.3%) and 75 (28.3%) in the control group had preterm delivery (P < 0.001) (Table 2).
| Variables | Intervention Group (N = 265) | Control Group (N = 272) | P-Value |
|---|---|---|---|
| Preterm delivery | 17 (6.3) | 75 (28.3) | 0.001** |
| Cerclage | 1 (0.4) | 1 (0.4) | 0.893# |
| Gestational age (week) | 36.25 ± 21.60 | 39.57 ± 21.64 | 0.036+ |
| Type of delivery | 0.329** | ||
| C/S | 182 (69.5) | 111 (74) | |
| NVD | 80 (35.5) | 39 (26) | |
| Newborn | 0.212** | ||
| Female | 111 (46) | 56 (39) | |
| Male | 132 (54) | 87 (61) | |
| Weight of neonate (gr) | 2702.77 ± 607.59 | 3273 ± 455.87 | 0.0001* |
Abbreviations: NVD, normal vaginal delivery; C/s, cesarean section.
a Values are reported as Mean ± standard deviation or number (%).
b P-value refers to student t‑test and chi‑squared when appropriate.
c Level of significance P < 0.0001**, P < 0.001+, P < 0.0001*, with respect to control
d **Chi-square test, #Fisher exact, * independent t student test, + Mann-Whitney test.
Multivariate-Binary regression analysis was used to estimate the interaction of different variables on outcome. Considering preterm labor as dependent and other variables (Multiparty, bleeding, anemia, intervention, and type of delivery) as independent variables, the study group (intervention or control) was the only predictor of preterm labor (OR-3.6, 95 %CI: 1.98 - 6.5, P < 0.001)
That is, preterm birth was reported in a higher percentage of participants in the control group (Table 2, 3). The two groups did not report Chorio amnionitis, postpartum sepsis, or hemorrhage.
| Variables | B | P-Value | Adjusted OR | 95% CI for Adj. OR | |
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Multiparity | -0.006 | 0.989 | 0.994 | 0.415 | 2.383 |
| Bleeding | -0.327 | 0.417 | 0.721 | 0.327 | 1.589 |
| Anemia | -2.266 | 0.092 | 0.104 | 0.007 | 1.449 |
| Group | 1.305 | 0.0001 | 3.686 | 1.819 | 7.470 |
| Delivery | 0.773 | 0.081 | 2.166 | 0.910 | 5.155 |
| Constant | 0.163 | 0.956 | 1.177 | - | - |
Abbreviations: CI, confidence interval; Adjusted OR, adjusted odds ratio.
a Preterm labor = Outcome or dependent variable.
b Level of significance P < 0.0001.
c Variable (s) entered on step 1: Multiparity, bleeding, anemia, preterm. Delivery, group, delivery.
5. Discussion
The results of the current study revealed that garlic tablets could be beneficial in reducing preterm delivery. This study's total preterm delivery rate was 17%, consistent with the global estimate (preterm delivery between 5 - 18%) (15, 16).
Myhre et al. assessed the role of dried fruits and garlic pills on preterm labor and found that they are protective agents for preterm delivery [OR: 0.74 (95% CI: 0.65, 0.95)] (16). They argued that fruits containing antimicrobial or anti-inflammatory properties could reduce the risk of preterm labor.
According to regression analysis of the current study, the study group (intervention or control) was the only predictor of preterm labor (OR-3.6, CI95%: 1.98 - 6.5, P < 0.000), which could indicate the beneficial effect of consuming garlic peels for preterm labor prevention. Also, Myhre et al. found that probiotic consumption will reduce the risk of preterm delivery (17). Garlic with allicin has antibacterial properties against E. coli, S. aureus, E. faecalis, K. pneumonia, Candida spp., and T. vaginalis (18-22). Also, clinical evidence has revealed that oral garlic tablets can be as effective at treating Trichomonas vaginalis (23). This wide range of antimicrobial activity will decrease vaginal infection and reduce preterm labor (17). Garlic has antifungal activity against C. albicans, Candida, and Streptococcus mutants, which are responsible for preterm labor (18, 24).
Previous studies showed that women with bacterial vaginosis during pregnancy are at higher risk of preterm labor than those with normal vaginal flora (25). Administration of antibiotics such as garlic peels would help normalize vaginal flora and reduce preterm births. Preterm birth is one of the most common causes of neonatal death, and nearly 35% of neonatal deaths occur due to preterm labor (26-28). Therefore, according to the results of this study, it may be possible to point out the role of garlic tablets in preventing premature births.
The best strategy to study the role of garlic in preventing preterm birth is to target patients with recurrent spontaneous preterm labor. This was followed in the current study. Our findings can only be interpreted in high-risk women for preterm labor, and a high rate of our patients did continue their follow-up. The main power of this study is the large sample size and the prospective design. The limitations of this study; Failure to measure vaginal microbes and their changes with the use of garlic pills. Therefore, it is suggested to investigate these changes in future clinical trials. Also, studies are needed to improve methods of preterm birth prevention and facilitate effective health promotion strategies that include nutritional interventions during pregnancy or early pregnancy.
5.1. Conclusions
The study's results showed that the combined treatment significantly prolonged the pregnancy or improved its outcomes. Garlic tablets seem to be effective in preventing preterm birth.