1. Background
Coronavirus disease 2019 (COVID-19) was declared a pandemic by the World Health Organization (WHO) in March 2020, following confirmed cases in 114 countries (1, 2). By November 24, 2022, the global crisis affected 633 million people, costing over 6.5 million lives (3). In Morocco, the Ministry of Health announced the first confirmed case on Monday, March 2, 2020 (4). Since then, 1.2 million confirmed COVID-19 cases have been reported to the WHO, resulting in 16.283 deaths in all regions of the country, with different distribution. As of 15 November 2022, 55 million vaccine doses have been administered (2).
Since the beginning of this health crisis, the notion of perceived drug risk and adverse effects has changed. Fear of becoming infected with this novel virus, unknown to the general population, prevailed over safety, giving people the impression that their only option is self-care and self-medication (1). Such a feeling of fear has increased, particularly with the high mortality rate in the absence of a specific therapy or vaccine for this disease (1, 5). The literature review indicated that anxiety and depression symptoms (16 - 28%) and self-reported stress (8%) were common reactions to the COVID-19 pandemic problems, including poor sleep quality (6). The psychological distress and fear generated by a new disease can also lead to changes in behavior. Consequently, many individuals, particularly those who feel ill, have turned to consuming various drugs, including traditional medicines, to treat or prevent a perceived COVID-19 infection without consideration for safety and effectiveness on the human body (1, 5).
Several countries, including Morocco, imposed lockdowns to control the infection and limit its spread among the population (7). Many small clinics and treatment facilities have also been closed during the COVID-19 pandemic, leaving people without common advice or urgent medical help (7). All of these factors had been conducive to self-medication.
According to the WHO, self-medication has been defined as the selection and use of drugs by individuals for the treatment of self-identified symptoms or diseases (8). Inappropriate drug use may impact human health due to multiple toxicological and pharmacological risks (1). It may also be associated with increased morbidity and mortality due to misdiagnosis and delayed search for appropriate medical advice and treatment, as well as an increased risk of drug interactions, medical expenses, medication errors, and antimicrobial resistance (9).
Most drugs consumed without clinical evidence for treating COVID-19 include azithromycin, hydroxychloroquine, some antiretrovirals, and calcium supplements (8). Meanwhile, zinc and vitamin D have been recommended for their intervention to strengthen the immune system and prevent the cytotoxicity of chloroquine (10). Introducing vitamin C to the treatment of COVID-19 patients was also proposed (10). The use of traditional herbs should also be considered. In Africa, they are used as alternative drugs and play a crucial role in treating diseases (8). Several studies have reported various motivations for self-medication, including previous experience with the disease, high costs of medical services, the existing bureaucracy in healthcare facilities, and low regulatory activity (11, 12). Self-medication is a serious public health problem, so we need to understand this practice and the triggers within the population.
Due to the limited studies conducted in Morocco and in order to strengthen researchers’ efforts to provide more results regarding the prevalence and risk factors of self-medication during the COVID-19, we conducted the current research to study the prevalence and associated factors of self-medication practices in the Moroccan population.
2. Objectives
The findings of our study and the results of studies around the world will provide the information needed to develop awareness programs and policies to address self-medication.
3. Methods
3.1. Study Design and Sampling
The present cross-sectional survey using a self-administered questionnaire (printed copies) was conducted in the city of Meknes (North Central of Morocco) from March 2022 to June 2022 to investigate the level of self-medication practice before and during the COVID-19 pandemic. The minimum sample size of 384 was calculated using the Cochran formula for cross-sectional studies for the 95% confidence level and 5% margin of error for a general population estimated at 835695 (13). A total of 400 respondents took part in the study after the deletion of incomplete responses. A pilot test was conducted with 40 participants to check the acceptability and validity of the questionnaire. Some changes were made after the pilot testing. It should be noted that these 40 people interviewed during the pilot test were excluded from the study.
3.2. Questionnaire Design
The survey contained 20 questions in three languages, including French, Arabic, and Amazigh, as languages used in Morocco, and covered four sections. It was prepared and validated by multidisciplinary authors consisting of medical epidemiologists, pharmacologists, and microbiologists. All questionnaire sections were developed based on the data reported in the literature and contained different sections. The first and second sections included socio-demographic information and clinical features of participants, respectively. The other two sections focused on the prevalence of self-medication before and during COVID-19, the reasons behind self-medication, and adverse drug reactions. In the case of uneducated participants, the questions were read and construed. Generally, each participant took 10 - 15 minutes to respond to all questions.
3.3. Inclusion and Exclusion Criteria
The inclusion criteria included being an adult (aged ≥18 years), being consent to participate in the study, and residing in the city of Meknes. Furthermore, pregnant women and children were not included in the study.
3.4. Ethical Considerations
The present study was conducted anonymously to ensure confidentiality and reliability. The study aimed to communicate with all participants. Those who accepted to participate in our study were asked to sign a consent form. The participants were not involved in any stages of the study.
3.5. Data Analysis
The dependent variable was self-medication for COVID-19, coded as binary responses: No = 0 and Yes = 1. Independent variables consisted of socio-demographic characteristics and self-medication practices.
Data were analyzed using Stata 14 software (Corp. 2015. Stata Statistical Software: Release 14. College Station, TX: Stata Corp LP). The data of all returned questionnaires (N = 400) were entered into Excel (Windows 11, Microsoft Corporation), cleaned, coded, and exported to Stata 14. Descriptive statistics were used to characterize the sample and study variables (frequencies, percentages, means, and standard deviations [SDs]). The comparison between self-medication before and during COVID-19 was tested using the chi-square test and odds ratio (OR). A multivariate logistic regression model was used to identify factors associated with self-medication. The significance level was determined at a P-value below 0.05 with a 95% confidence interval (CI).
4. Results
The survey involved 400 respondents from the general population (mean age = 34.97 ± 15.8 years). Among the sample, 185 (46.25%) were female, with a sex ratio of (M/F) 1.16 for the male sex. Most respondents (56.25%) were under the age of 30, while the 31 - 40 age group (9.75%) and the > 60 age group (10%) were proportionally similar. A total of 240 (60%) were university graduates, and all participants (100%) were citizens of Morocco. Only 18.25% reported prior comorbid conditions, while the majority (80.75%) had medical insurance and were in good health (based on self-report) (47%). All demographic characteristics are shown in Table 1.
| Characteristics | Frequency |
|---|---|
| Gender | |
| Female | 185 (46.25) |
| Male | 215 (53.75) |
| Age (y) | 34.97 ± 15.8 |
| Age group | |
| ≤ 30 | 225 (56.25) |
| 31 - 40 | 39 (09.75) |
| 41 - 50 | 44 (11) |
| 51 - 60 | 52 (13) |
| > 60 | 40 (10) |
| Level of education | |
| No formal education | 51 (12.75) |
| Elementary school | 24 (06) |
| Secondary school | 85 (21.25) |
| University education | 240 (60) |
| Sector of activity | |
| Students | 134 (33.50) |
| Healthcare | 53 (13.25) |
| Education | 26 (06.50) |
| Housekeeper | 105 (26.25) |
| Retired | 41 (10.25) |
| Other | 41 (10.25) |
| Medical insurance | |
| Yes | 323 (80.75) |
| No | 77 (19.25) |
| Comorbidities | |
| Present | 73 (18.25) |
| Absent | 327 (81.75) |
| Self-reported health | |
| Excellent | 69 (17.25) |
| Good | 188 (47) |
| Fair | 114 (28.50) |
| Poor | 23 (05.75) |
| Very poor | 6 (01.50) |
Socio-Demographic Characteristics of Respondents (N = 400) a
According to the survey, 291 (72.75%) out of 400 respondents practiced self-medication, while 109 (27.25%) did not. Moreover, the study revealed that before the pandemic, 314 (78.50%) participants had used self-medication, compared to 86 (21.50%) who had not. According to our findings, self-medication during the COVID-19 period decreased statistically significantly compared to the pre-pandemic period (P = 0.0001). In the population studied before the pandemic, self-medication risk appeared to be significantly higher than during the pandemic. The OR analysis (Table 2) revealed a greater than 1 risk ratio between the two periods of self-medication (OR= 5.23; 95% CI: 3.047 - 8.99). Therefore, self-medication was more prevalent before the COVID-19 outbreak than during the outbreak.
| Self-Medication Practice During the COVID-19 Pandemic | Odds Ratio (CI 95%) | P-Value | |||
|---|---|---|---|---|---|
| No | Yes | Total | |||
| Self-medication practice before the COVID-19 pandemic | 5.23 (3.047 - 8.99) | 0.0001 a | |||
| No | 48 | 38 | 86 (21.50) | ||
| Yes | 61 | 253 | 314 (78.50) | ||
| Total | 109 (27.25) | 291 (72.75) | 400 (100) | ||
The Self-medication Practice Before and During the Coronavirus Disease 2019 Pandemic (Odds Ratio) (N = 400)
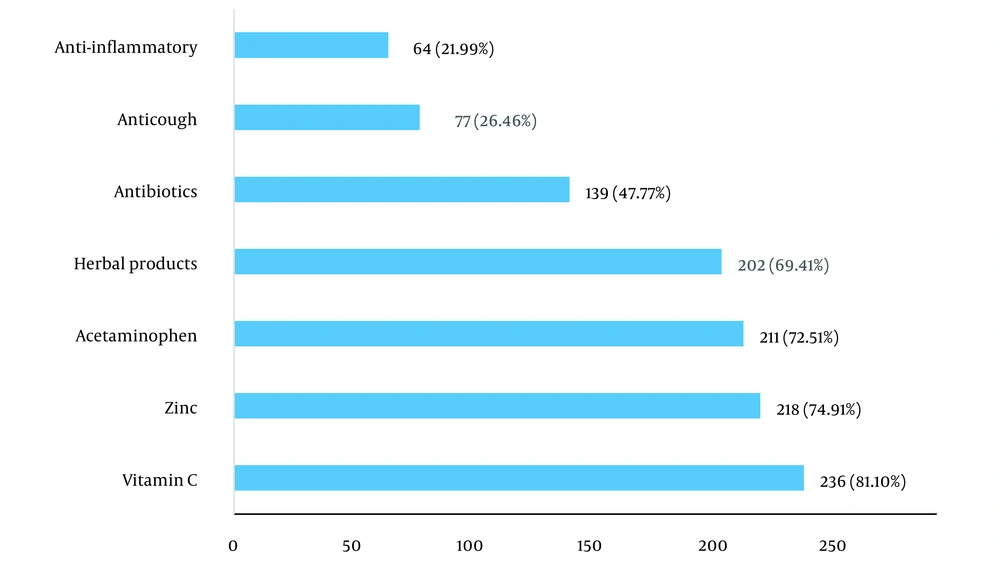
Figure 1 shows that most medications used for self-medication to prevent or treat COVID-19 were supplements such as vitamin C (81.10%) and zinc (74.91%), followed by acetaminophen (72.51%) and herbal products (69.41%). Anti-inflammatories were the least mentioned drug for self-medication in the COVID-19 pandemic (21.99%).
The participants reported using herbal products for therapeutic purposes. Various forms and uses are available for these products. Infusions constituted the majority (95.54%), followed by nasal sprays (42.08%), aerial sprays (23.27%), and massage balms (14.36%). These herbal products were predominantly composed of Eucalyptus globulus (92.57%), Mentha pulegium (75.74%), Zingiber officinale (72.28%), Citrus limon (61.39%), Thymus vulgaris (44.06%), and Rosmarius officinalis (33.06%).
Among the respondents practicing self-medication, 208 (71.48%) self-medicated when symptoms of COVID-19 developed, 43 (14.78%) practiced self-medication to prevent the apparition of symptoms, and 40 (13.74%) were confirmed positive for the COVID-19 test (polymerase chain reaction (PCR) test) (Table 3). Fatigue or asthenia (95.16%), headache (92.34%), myalgia (79.84%), cough (41.53%), fever (35.48%), and loss of smell and taste (9.27%) were common symptoms during the pandemic for which respondents used drugs. The analysis of the results also showed that the most common source of self-medication information came from websites and the media (38.83%), followed by friends and family advice (33.1%). Only 15.81% of respondents identified the pharmaceutical worker as a source of information.
Self-medication for COVID-19 was mainly due to fear of being tested positive for COVID-19 (22.68%), media impact (20.27%), and financial issues (17.87%). Other reasons reported were the distance from the healthcare institution (14.09%), fear of being quarantined (13.75%), fear of discrimination (6.19%), and fear of going to the hospital (5.15%) (Table 3).
| Characteristics | Variables |
|---|---|
| Gender | |
| Male | 135 (46.39) |
| Female | 156 (53.61) |
| When did self-medication start? | |
| For prevention without symptoms | 43 (14.78) |
| Confirmed positive test (PCR test) | 40 (13.74) |
| When symptoms of COVID-19 developed (without biological or clinical confirmation) | 208 (71.48) |
| Symptoms (one or more) (n = 248) b | |
| Fatigue or asthenia | 236 (95.16) |
| Myalgia | 198 (79.84) |
| Fever | 88 (35.48) |
| Cough | 103 (41.53) |
| Loss of smell and taste | 23 (9.27) |
| Breathing difficulty | 18 (7.26) |
| Headache/migraine | 229 (92.34) |
| Other symptoms | 36 (14.52) |
| Source of information | |
| Advice from friends or family | 78 (26.80) |
| Websites and the media | 113 (38.83) |
| Worker in pharmacy | 46 (15.81) |
| Yourself | 54 (18.56) |
| Reasons for self-medication | |
| Fear of going to the hospital | 15 (5.15) |
| Fear of being tested positive for COVID-19 | 66 (22.68) |
| Financial issues | 52 (17.87) |
| Fear of discrimination | 18 (6.19) |
| Fear of being quarantined | 40 (13.75) |
| Media impact | 59 (20.27) |
| Distance from the healthcare institution | 41 (14.09) |
| Improvement after taking drugs (n = 248) b | |
| Relief of all the symptoms | 54 (21.77) |
| Relief of almost all symptoms | 68 (27.42) |
| Relief of some symptoms | 65 (26.21) |
| Relief of one symptom | 30 (12.10) |
| Persistence of symptoms | 31 (12.50) |
Description of the Characteristics Associated with Self-medication During the Coronavirus Disease 2019 Pandemic (N = 291) a
In the bivariate logistic regression model, age, gender, education level, self-reported health, sector of activity, and medical insurance were analyzed. Multivariate analyses showed that the younger age group (≤ 30 years) (OR = 1.59; 95% CI: 0.96 - 2.78), university education (OR = 1.47; 95% CI: 0.87 - 2.99), and good self-reported health (OR=2.83; 95% CI: 1.43 - 3.71) were independently associated with self-medication (Table 4).
| Variables | Univariate | Multivariate | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | P-Value | AOR | 95% CI | P-Value | |
| Age (y) | ||||||
| ≤ 30 | 2.59 | (0.75 - 5.38) | 0.001 | 1.59 | (0.96 - 2.78) | 0.001 |
| > 30 | 1.00 | Reference | ||||
| Gender | ||||||
| Male | 0.96 | (0.66 - 1.52) | 0.84 | |||
| Female | 0.75 | (0.24 - 2.22) | 0.60 | |||
| Level of education | ||||||
| No formal education | 1.36 | (1.04 - 1.75) | 0.38 | |||
| Elementary school education | 1.19 | (0.92 - 1.44) | 0.40 | |||
| Secondary school education | 1.06 | (1.04 - 1.75) | 0.66 | |||
| University education | 1.73 | (0.69 - 3.27) | 0.000 | 1.47 | (0.87 - 2.99) | 0,000 |
| Self-reported health | ||||||
| Excellent | 2,35 | (1.36 - 4.09) | 0.52 | |||
| Good | 3,56 | (1.85 - 6.88) | 0.002 | 2.83 | (1.43 - 3.71) | 0.032 |
| Fair | 0.89 | (0.31 - 2.65) | 0.22 | |||
| Poor | 2.23 | (0.89 - 4.89) | 0.13 | |||
| Very poor | 1.51 | (0.80 - 2.97) | 0.19 | |||
| Sector of activity | ||||||
| Students | 2,33 | (0.29 - 4.18) | 0.050 | 1.94 | (0.82 - 3.56) | 0.17 |
| Healthcare | 0,19 | (0.12 - 0.33) | 0.36 | |||
| Education | 0.87 | (0.24 - 2.18) | 0.63 | |||
| Housekeeper | 3.08 | (2.00 - 5.14) | 0.87 | |||
| Retired | 1.25 | (0.87 - 3.13) | 0.18 | |||
| Other | 1.03 | (0.69 - 2.16) | 0.27 | |||
| Medical insurance | ||||||
| Yes | 1.00 | Reference | ||||
| No | 0.79 | (0.13 - 0.88) | 0.88 | |||
Multivariate Analysis of the Factors Associated with Self-medication During the Coronavirus Disease 2019 Pandemic
5. Discussion
To our knowledge, this study is the first research conducted in Morocco in the context of the COVID-19 pandemic. Self-medication is a global phenomenon that can present risks to human and community health (14, 15). Although it is approved by the WHO for minor diseases, it should be practiced cautiously (16). Our research found that self-medication for COVID-19 was prevalent at 72.75%. The prevalence of self-medication may be influenced by differences between countries regarding advertising, legislation, and the possibility of obtaining certain drugs without a prescription (17, 18). It may explain the large disparity in frequencies between countries. The Shrestha team’s systematic review of self-medication practices throughout the COVID-19 pandemic indicated that out of the 14 studies examined, the mean prevalence of self-medication during COVID-19 was estimated at 44.78% globally. In 11 studies in the general community, the prevalence ranged from 19.3% to 88.3% (7), putting our score in the upper limit of global frequencies next to Bangladesh and Jordan, which got 88.33% and 80% in their studies, respectively (7, 19). Our study also revealed a statistically significant decrease in the number of respondents who self-medicated during COVID-19 compared to the pre-pandemic period. Self-medication is 5.23 times more likely to happen during COVID-19. Dare et al.’s study showed a considerable decline in the number of Ugandans who self-medicated before the COVID-19 pandemic compared to the COVID-19 lockdown period (20). In Kenya, the same situation was observed where the prevalence of self-medication increased from 36.2% before the pandemic to 60.4% during the pandemic (21). The change in prevalence between the two periods (before and during the pandemic) could result from a change in people’s behavior to deal with this new and unknown disease. During the lockdown, people focused more on their health because they were encouraged to practice better personal hygiene. Consequently, under stress and anxiety, they tried to protect themselves by using several types of medications and even home herbal preparations. Matthieu Grégori’s study shows that the market share of self-medication increases during epidemics (22).
The analysis of the decrease in the number of arbitrary drug users compared to the pre-COVID-19 period could be explained, among other things, by the number of awareness and information campaigns run daily by health authorities to train the public about the dangers of arbitrary drug use. It should also be noted that strict measures on the part of the authorities not to sell medicines arbitrarily or without a prescription have been observed. Confinement may also make access to medicines more difficult.
Generally, buying a drug is often based on pharmaceutical advice, personal experience, or parental advice. However, in the context of COVID-19, another determinant motivating self-medication was drug advertising (23). During the COVID-19 epidemic, a number of substances were popular, primarily vitamins C and D, chloroquine, hydroxychloroquine, and food supplements. Some of those treatments actually have serious side effects, like antibiotic resistance caused by overuse of antibiotics, bleeding induced by aspirin, hydroxychloroquine arrhythmia, and suppression of the immune system, possibly due to corticosteroid use (24). To our knowledge, the used doses of zinc, vitamin C, etc., were not adapted to the COVID-19 period and severity. Undoubtedly, patients have based their dosage decisions on the package leaflet or on the experience of others who have contracted the disease.
In this study, vitamin C was the most commonly used drug, with 81.10%. This is consistent with the Algerian study, where 91.40% of pharmacists found increased consumption of vitamins and nutritional supplements (23). In Togo, vitamin C, and traditional medications were also the most common (25). Vitamin C seems to help boost the immune system (26). Several teams have therefore proposed vitamin C supplementation for preventing and treating COVID-19 (27, 28). However, excessive supplementation without medical monitoring can result in adverse reactions (use cautiously in patients with a history of renal lithiasis or renal failure) (29), particularly as studies regarding the use of vitamin C in the treatment and prevention of respiratory infections are inconclusive (30). In addition, self-medication with additional minerals such as zinc is also used because of its ability to enhance innate and adaptive immunity during viral infections (31).
Acetaminophen was the third most consumed drug, equal to 72.51%. It is also a drug that is preferentially auto-medicated in Peru (32), Pakistan (33), and Guinea (6). The massive consumption of this medication may result from its availability for sale without a physician’s prescription. Indeed, using vitamins as supplements or acetaminophen during pain is not considered arbitrary in many societies, such as Morocco. The misuse of acetaminophen has serious consequences (6). It is alarming that its consumption is considered nontoxic at any dose (34). The standard oral dose of acetaminophen is 0.5 - 1 g every 4 - 6 h, up to 4 g/day, but more importantly, it has dose-related toxicity (35). Acetaminophen may induce hepatotoxicity after significant overdose (36), and serious liver injury has been observed with long-term use, even at therapeutic doses in patients with alcoholic liver disease or viral infections (37). Therefore, acetaminophen is a medication to be used cautiously, particularly because its sales have increased significantly during the COVID-19 pandemic (38).
The results also showed self-medication with herbal products to treat or prevent COVID-19. The reason may be due to the fact that the use of traditional medicines is commonplace in African culture and relatively cheaper than modern medicines (25), even if their composition is usually unknown (25). In Morocco, social media broadcasts on the use of Syzygium aromaticum and Artemisia herba alba to protect against COVID-19. The WHO is working with research institutions to select traditional medicines for investigation into the clinical efficacy and safety of COVID-19 treatment (39).
We have no information regarding the biological effects of medicinal plants on COVID-19, but their diverse secondary metabolites provide innumerable advantages (40). There are many biological effects they are capable of producing, including anti-inflammatory (Eucalyptus globulus, Zingiber officinale, Citrus limon), antimicrobial (Eucalyptus globulus, Mentha pulegium, Zingiber officinale, Thymus vulgaris, Citrus limon), antioxidant (Eucalyptus globulus, Mentha pulegium, Zingiber officinale, Thymus vulgaris, Rosmarius officinalis), and analgesic properties (Eucalyptus globulus) (40).
Moroccans have grown increasingly interested in dietary supplements and herbal products in recent years, particularly since social networking sites have contributed to the popularity of these products, particularly during the recent pandemic.
Antimalarials (chloroquine and hydroxychloroquine) were excluded from our study because Moroccan health authorities had removed them from pharmacies. The use of these drugs has been limited to the hospital environment under medical supervision due to the adverse reactions they may cause in case of abuse. The choice of hydroxychloroquine and chloroquine was based on a non-randomized study conducted in France showing positive results in treating COVID-19 patients, particularly those treated with hydroxychloroquine 600 mg/day (41).
In line with other self-medication studies, our study showed that some participants also used antibiotics. They rank fifth, with 47.77% of people who used them. Several studies show that the antibiotics most consumed during the pandemic were amoxicillin, ciprofloxacin, azithromycin, and erythromycin (1, 6, 32, 42). According to a study conducted in Peru, one in five people took azithromycin as a preventive measure without respiratory symptoms (32). Another study showed a synergic effect of the association of azithromycin and hydroxychloroquine against the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (41). Reports also indicate potential anti-inflammatory properties of azithromycin that may reduce the progression of COVID-19 (42, 43). However, its administration in association with hydroxychloroquine was involved in elevating the QT interval (44). Consumption of hydroxychloroquine with or without azithromycin has increased cardiotoxic risks such as QT prolongation and sudden death (44).
Without any clinical or biological confirmation, self-medication was used in our context when symptoms including cough, weariness, and headaches (71.48%) that are comparable to COVID-19 symptoms first appeared. The preferred source of self-medication drugs was websites and the media. Several scientific articles were the subject of a systematic review by Shrestha et al. discovering that pharmacy accounted for 89.5% and 73.9% of the information sources in Kenya and Nigeria, respectively (7). In Pakistan, prescriptions from family or friends predominated (7). Our findings can be explained by the fact that our study has been carried out in a city where internet usage is common.
Our analysis discovered two risk factors: Those under 30 years of age and university education. This outcome is in line with what we discovered regarding the website that served as the information’s primary source. Since young college students are the biggest Internet users across all platforms, including websites, social networks, etc., numerous investigations, including Sadio et al.’s study in Togo, Janatolmakan et al.’s study in Iran, and Zhang et al.’s study in China, found the level of education to be a risk factor (25, 45, 46). Several publications also recognized gender, old age, health sector worker, insurance coverage, and rating anxiety scale as risk factors (1, 25, 32, 45, 46)
5.1. Conclusions
In Morocco, self-medication has been a serious health concern, particularly during the COVID-19 pandemic. For COVID-19-related symptoms, a number of medications were taken without the necessary scientific support. The most common supplement was vitamin C, but acetaminophen, herbal products, and antibiotics like azithromycin were also widely used. Self-medication practiced improperly can lead to a false diagnosis, serious side effects, drug interactions, drug addiction, and bacterial resistance. Our findings should be viewed cautiously because they are not applicable to the entire Moroccan population. However, we hope that these findings will enlighten healthcare policymakers about ways to improve pharmaceutical care as they aim to save lives.