1. Background
Episiotomy is a commonly performed obstetric procedure, and postoperative perineal pain is a troublesome complication for women (1). This pain can negatively impact physical, psychological, and social aspects of a person’s life, including limited movement, difficulties with urination and defecation, baby care, and breastfeeding. It can also disrupt family and marital relationships by causing dyspareunia (2). Furthermore, perineal pain is a significant factor contributing to women's fear of childbirth and their preference for cesarean delivery (1-3).
Various methods have been recommended to alleviate perineal pain following episiotomy, including pharmacological and non-pharmacological approaches. Pharmacological methods include medications such as aspirin-codeine, acetaminophen-codeine, non-steroidal anti-inflammatory drugs (NSAIDs), and anesthetics like lidocaine spray or gel. Non-pharmacological methods encompass the use of cold and heat therapy, acupressure, acupuncture, relaxation techniques, distraction, and music therapy (4-6). Among these approaches, lidocaine is one of the most commonly used medications for pain relief. Different forms of lidocaine, including spray, gel, and cream/ointment, are viable options for alleviating perineal pain. The advantages of topical products include localized effects with minimal systemic absorption, ease of preparation, and administration by the patient (7-12).
However, there is conflicting information regarding the effectiveness of lidocaine in relieving perineal pain. Corkill et al. reported the efficacy of lidocaine gel in relieving perineal pain during the first two days after delivery (13). Conversely, Minassian et al. concluded that the use of topical plant compounds was more effective and safer than lidocaine (14). Based on our understanding of pain relief mechanisms, effective topical analgesics should contain compounds that penetrate the skin and inhibit pain receptors such as cation receptor potential channels and cyclooxygenase-2 (11). Another advantage of local anesthesia is that inhibiting pain signals in the skin disrupts the pain cycle and prevents internal organs from being exposed to high levels of systemic analgesics (13).
The clove plant (Syzygium aromaticum) is a medicinal herb that has garnered attention in traditional medicine (14). Belonging to the Myrtaceae family, it contains volatile essential oils, tannins, caryophyllene, triterpenes, and esters. Clove glycosides consist of aliphatic alcohols, monoterpenoids, eugenol, isoeugenol, farnesol, sitosterol, nerolidol, and campestral (15). Clove oil, derived from clove buds, is widely used in the production of medicines, cosmetics, and hygiene products. It is beneficial in treating wounds and injuries, particularly on delicate skin. Clove oil is employed in the formulation of anti-acne compounds and as a remedy for insect bites and purulent pimples (16). The pain-relieving properties of clove are attributed to the presence of eugenol, which inhibits the production of prostaglandins (15).Clove oil and extracts have also been traditionally used as analgesics in dentistry (17).
2. Objectives
This study aimed to compare the potential effect of lidocaine alone versus lidocaine combined with clove oil on episiotomy site anesthesia.
3. Methods
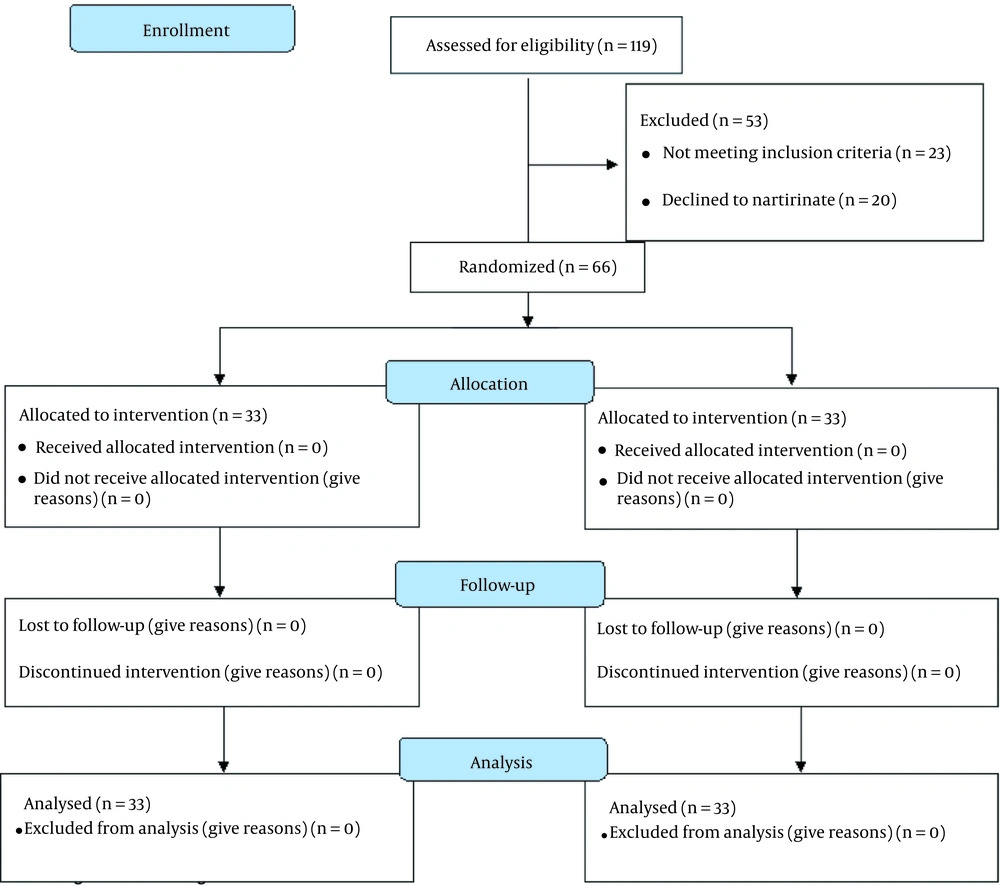
The present study was a randomized parallel clinical trial with a 1:1 allocation ratio, conducted at Baharloo Hospital in Tehran. A total of 66 nulliparous women who underwent episiotomy were included, with 33 assigned to the lidocaine group and 33 assigned to the lidocaine and clove oil group. The study received approval from the ethics committee and was registered in the Iranian Registry of Clinical Trials with identification numbers IR.TUMS.FNM.REC.1399.212 and IRCT20110621006854N4, respectively. Inclusion criteria were as follows: Singleton pregnancy, aged between 18 and 35 years, gestational age between 38 and 42 weeks, and vaginal non-instrumental delivery. Participants were excluded if they had undergone manual removal of the placenta, had a history of medical or obstetric complications before or after delivery, had specific food or medication allergies, experienced a third- or fourth-degree perineal tear, had a second stage of labor lasting more than 2 hours, were candidates for cesarean section, or did not require episiotomy (Figure 1).
3.1. Randomization and Blinding
The women were randomly assigned to either the control or intervention groups using the random block method. Four blocks were selected from six possible sequences (BAAB, BABA, BBAA, ABBA, ABAB, AABB). The letter "A" was assigned to the intervention group, and the letter "B" to the control group. These sequences were placed in sealed envelopes. An external observer performed the randomization process, repeating it with replacement until the desired sample size was reached. Allocation was concealed, meaning neither the participants nor the research team knew which group each person was assigned to. While blinding the participants and research team was not feasible due to the nature of the intervention, the data analysts were kept unaware of the treatment given to maintain blinding.
3.2. Intervention
At the beginning of the study, each participant completed consent and demographic information forms. The researcher measured the weight and height of the participants using a standard scale equipped with a height gauge in the hospital. In the control group, 5 cc of the routine injectable form of 2% lidocaine (manufactured by Caspian Tamin Pharmaceutical Company) was utilized. In the intervention group, 10 minutes before the scheduled time for the lidocaine injection, clove oil from Narin Gol Company with a concentration of 0.8% was applied. A total volume of 10 cc was utilized for each participant. The same dosage of injectable lidocaine was administered in this group as well. The perineum was massaged with clove oil, and then lidocaine was administered at the appropriate time, using the same dosage and amount as the control group. During the episiotomy repair, both groups received a 2% lidocaine injection. The researcher administered the clove oil and facilitated the entire process of vaginal delivery and episiotomy repair for the patients.
3.3. Instruments
The severity of pain was assessed using the Visual Analog Scale (VAS) and the McGill Pain Questionnaire at 1, 6, and 12 hours after episiotomy repair. Additionally, demographic characteristics were evaluated using a demographic questionnaire.
3.4. Statistical Analyses
To calculate the effect size, the study by Rajabzadeh et al.(18) was utilized, taking into account the mean and standard deviation. G*Power software was employed to determine the sample size, resulting in a calculated size of 30 women in each group, considering a 10% dropout rate. Thus, the final sample size consisted of 33 participants in each group. For statistical analysis, various inferential statistical tests were utilized, including independent t-tests, analysis of variance with repeated measures, descriptive frequency analysis, frequency percentages, means, and non-parametric tests such as the chi-square test. The research units were comparable in terms of the type of suture material used, degree of perineal tear, amount of anesthetic solution, and repair method. There were no participants lost to follow-up in this study, and data from all 66 participants were included in the analysis.
4. Results
Table 1 presents a comparison of demographic variables between the two groups. The results indicate that there were no significant differences observed between the groups.
| Variables | Lidocaine and Clove Oil (N = 33) | Lidocaine (N = 33) | P-Value b |
|---|---|---|---|
| Age (y) | 26 ± 6.2 | 29 ± 5.35 | 0.78 |
| BMI (kg/m2) | 23.6 ± 1.04 | 24.01 ± 1.1 | 0.06 |
| Gestational age (week) | 39.23 ± 0.76 | 38.62 ± 1.26 | 0.07 |
a Values are expressed as mean ± SD.
b Independent t-test.
The results indicate that there was no statistically significant difference between the two groups before and 12 hours after the intervention (P > 0.05). However, at 1 and 6 hours after the intervention, there was a statistically significant difference observed between the two groups (P < 0.05) (Table 2).
| Time Groups | Lidocaine and Clove Oil Mean ± SD | Lidocaine | P-Value b |
|---|---|---|---|
| Before the intervention | 3.78±1.23 | 3.18±1.57 | 0.68 |
| 1th hour | 5.03±2.13 | 6.88±1.08 | 0.000 |
| 6th hour | 3.39±2.03 | 3.73±1.12 | 0.000 |
| 12th hour | 1.42±1.09 | 1.55±1.23 | 0.068 |
a Values are expressed as mean ± SD.
b Independent t-test.
To examine the combined effect of group and time on the mean pain scores, a repeated measures ANOVA was conducted (Table 3). To assess the sphericity of the data, Mauchly's test was performed, and the Greenhouse-Geisser correction was applied to interpret the results
| Time Groups | Lidocaine and Clove Oil | Lidocaine | P-Value b |
|---|---|---|---|
| Before the intervention | 3.21 ± 1.14 | 3.06 ± 1.17 | 0.63 |
| 1th hour | 5.39 ± 2.19 | 5.74 ± 2.41 | 0.000 |
| 6th hour | 3.23 ± 1.19 | 3.81 ± 2.26 | 0.000 |
| 12th hour | 1.17 ± 1.45 | 1.31 ± 1.03 | 0.071 |
a Values are expressed as mean ± SD.
b Independent t-test.
The results of the repeated measures ANOVA indicated a statistically significant difference between the two groups in each of the two pain assessment scales (P < 0.05). This finding suggests that both the VAS and McGill scales showed significant differences in pain scores between the control and intervention groups across different time points.
The use of repeated measures ANOVA allows for the examination of within-subject changes over time and the comparison of these changes between different groups. By considering the sphericity of the data and applying appropriate corrections, the analysis provides reliable results for assessing the simultaneous effects of group and time on pain levels (Table 4).
| Group Scale | Lidocaine and Clove Oil | Lidocaine | P-Value b | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Before | 1th h | 6th h | 12th h | Before | 1th h | 6th h | 12th h | ||
| VAS Scale | 3.78 ± 1.23 | 5.03 ± 2.13 | 3.39 ± 2.03 | 1.42 ± 1.09 | 3.18 ± 1.57 | 6.88 ± 1.08 | 3.73 ± 1.12 | 1.55 ± 1.23 | 0.000 |
| McGil Scale | 3.21 ± 1.14 | 5.74 ± 2.41 | 3.81 ± 2.26 | 1.17 ± 1.45 | 3.06 ± 1.17 | 5.39 ± 2.19 | 3.23 ± 1.19 | 1.31 ± 1.03 | 0.000 |
a Values are expressed as mean ± SD.
b Repeated measure ANOVA.
5. Discussion
Episiotomy is a commonly performed surgery that can be quite painful. Pain plays a significant role in women's fear of childbirth and their preference for cesarean section. This study aimed to compare the potential effect of lidocaine alone versus lidocaine combined with clove oil on episiotomy site anesthesia. Pain relief measures can help alleviate discomfort and enable women to resume their normal activities more quickly.
The results of this study demonstrated a significant effect of the combination of lidocaine and clove oil in controlling pain during episiotomy among nulliparous women. No side effects were observed in any of the groups. Both the lidocaine group and the lidocaine and clove oil group experienced a decrease in average pain intensity, with a significant difference between the two groups observed at 1 hour and 6 hours after the intervention. The lidocaine and clove oil group exhibited slightly more satisfactory results. However, there was no significant difference in average pain intensity between the two groups at the 12-hour mark after the intervention.
In a study by Omidvar and Mir Mohammad Ali, which compared the effect of lidocaine with a placebo on episiotomy pain intensity in primiparous women, lidocaine was found to significantly reduce pain intensity at various time points after administration (19). However, their study differed from the present study in terms of the type of lidocaine used (gel form) and the shorter duration of examination (first 120 minutes after administration). Additionally, their study ethically deprived one group of participants from receiving pain relief, even though they were in pain.
Another study conducted in Turkey compared the effect of indomethacin vaginal suppositories with lidocaine ointment for pain treatment after episiotomy at different time points. The results showed a significant difference in pain intensity between the lidocaine group and the control group only during the first 15 minutes after drug administration (20). These studies support the effectiveness of lidocaine in reducing pain, although there are some differences in the specific interventions and study durations.
Regarding the clove oil group, there were no similar studies comparing the efficacy of clove oil with lidocaine. Due to ethical concerns regarding the use of pure clove oil for pain reduction, the study design was modified to the current intervention. Rajabzadeh et al. conducted a study on the effect of clove extract on pain intensity at the episiotomy site (18). They found that the intensity of labor pain was lower in the clove group compared to the placebo group on the fourth and tenth days after delivery. While their study focused on the postpartum period and differed in purpose from the present study, their findings support the effectiveness of cloves in reducing pain. This efficacy can be attributed to the presence of certain compounds in clove oil, such as aliphatic eugenol, monoterpenoid, farnesol, isoeugenol, campesterol, and nerolidol sitosterol, which inhibit prostaglandin production and exert analgesic effects. Other studies on animals and dental local anesthesia have also demonstrated the analgesic properties of cloves (19-24).
The present study is the first to compare the effect of clove oil with routine anesthesia using lidocaine. The findings suggest that lidocaine and clove oil may have similar pain-relieving effects. This is valuable considering the drawbacks of lidocaine, such as the risk of needle insertion into the fingers of healthcare providers and the potential impact on the baby's head. However, the study has some limitations, including its focus on primigravida women only and the inability to fully explore the pure effect of clove oil due to ethical considerations.
5.1. Conclusions
Considering the greater effectiveness of lidocaine combined with clove oil in reducing episiotomy site pain intensity and the absence of side effects, this combination can be recommended as an alternative approach for pain management at the episiotomy site.