1. Background
Urolithiasis is very common and is one of the common causes of emergency departments visits. The urolithiasis prevalence proportion in Iran is 5.7%, the incidence rate is 145/100,000 and its recurrence rate is 36% (1). Renal colic presents as complex symptoms characteristic for the presence of stone, which obstructs ureter. Ordinarily, the characteristic of pain is of sudden sensing in flanks and sometimes radiates to the system of genital. Moreover other symptoms include nausea, vomiting, and hematuria may be seen (2). Renal colic needs urgent and influential medication with pain killers such as narcotics, with or without spasmolytic drugs. The most frequently used agents are Pethidine and morphine (3).
The mechanism of action of opioids are through binding to specific proteins, named opioid receptors. Opioid receptors expressed in central and peripheral nervous systems. The opioid analgesic effects mediates via mu opioid receptor activation. Therefore, opioids, which are used as pain killers, are known as, “mu agonists” (4). In fact, several pathways enrolled in renal colic pain that include urinary obstruction with stone, urinary ducts` wall pressure, ureter smooth muscle spasm, stone area tissue edema and inflammation, as well as peristalsis aggravation (5, 6). The histamine-1 (H1) receptors have a wide distribution in body cells. Recently the studies showed that histamine receptors are also expressed in the ureter. Histamine can cause strong peristaltic contractions in the ureter (7).
Chlorpheniramine, propylamine H1-receptor antagonist (antihistamine), is used for allergy treatment. It is usually prescribe for flu and allergies. The half-lives of the drug elimination is varying 18 - 43 hours (8). We hypothesize that Chlorpheniramine can relieve renal colic pain by decreasing peristaltic contractions in the ureter. Therefore, the aim of this study was considered as a comparison of analgesic effect of morphine with and without Chlorpheniramine in patients with acute renal colic.
2. Methods
2.1. Study Design
In this randomized clinical trial, the patients suspected to renal colic who were admitted to the emergency departments of our university hospitals were recruited to the study. The inclusion criteria included individuals the age of 18 to 65 years, symptoms associated with acute renal colic, and the stone that was confirmed by kidney-bladder-urinary tract ultrasound or computed tomography scan. While patients under the age of 18 or above 65 years old, patients with signs related to a fever (temperature greater than 38 celsius degrees), absence of stone in radiologic evaluations, and abnormality in urinary tract were excluded from the study. Furthermore, patients with C criteria were excluded; angle-closure glaucoma, benign prostatic hypertrophy, peptic ulcer disease, bladder neck obstruction, gastric outlet obstruction, chronic obstructive pulmonary disease, asthma, urinary retention, hyperthyroidism, and cardiovascular diseases. This study was approved by Ahvaz Jundishapur University of Medical Sciences ethic committee. The study protocol was explained for all the patients. They were included after signed informed consent.
2.2. Therapeutic Intervention
The patients were randomly divided into 2 groups by block randomization method. Patients in group A received 1cc of intravenous chlorpheniramine containing 10 mg along with 5 mg of morphine sulfate. While group B patients received 1 cc Isotonic normal saline along with 5 mg morphine. Before treatment of pain, the score was measured by visual analog scale (VAS). The VAS scale, an adult unidimensional measure of pain intensity have 10 level points of representation of pain severity.
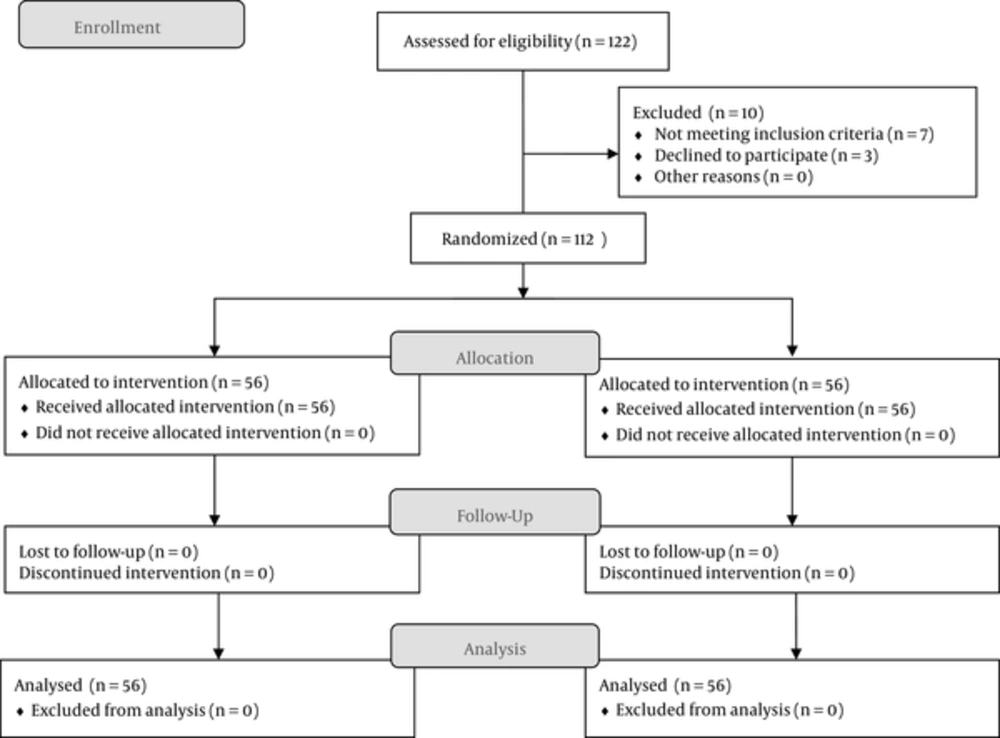
After the intervention, in time point including immediately before drug administration and 15, 30, 45, and 60 minutes after treatment the amount of pain was measured. All of the patients were followed up for 4 hours after treatment. The incidence of drug related adverse effects such as nausea, vomiting, vertigo, and constipation were evaluated. The patients whom did not response to trial analgesics after 60 minute of intervention, received another morphine rescue dose of 5 mg (Figure 1).
2.3. Statistical Analysis
The sample size was calculated 110/ group in respect of power of 90% of study, 0.05 type I error and correlation of 0.25. At first, the data obtained were examined in terms of descriptive indicators and then, to compare quantities between the 2 groups, according to normality of data, t-test and Mann-Whitney test were used. Normality of data was evaluated by Kolmogorov-Simonov normality. Statistical analysis was performed using the SPSS version 20. A P value < 0.05 assumed as significant.
3. Results
A total of 122 patients were included in the study, where 10 patients were dropped off due to the fact that they didn't meet the exclusion criteria or decline to participate in the study (Figure 1). Patients’ demographic characteristics have been shown in Table 1. Based on these results, age and sex distribution has no significant differences between the 2 groups. The mean age of patients was 40.20 ± 7.21 years. Furthermore, the participants have no impaired level of consciousness, drug allergy, and opiate addiction (Table 1).
| Variables | Morphine + Chlorpheniramine (n = 56) | Morphine (n = 56) | P Value |
|---|---|---|---|
| Age, y | 41 ± 6.1 | 4.23 ± 7.2 | 0.23 |
| Sex | 0.45 | ||
| Male | 73 | 69 | |
| Female | 27 | 31 | |
| Vital signs | |||
| Systolic pressure | 135.75 ± 20 | 132 ± 18 | 0.56 |
| Diastolic pressure | 76.23 ± 7.2 | 78.31 ± 6.3 | 0.59 |
| Respiratory rate | 17.32 ± 4.21 | 16.71 ± 3.11 | 0.47 |
aValues are expressed as mean ± SD or %.
The amount of pain before starting an intervention has no statistical significant differences between 2 groups. After treatment in group A, VAS score decreased from 8.5 to 2.1 and in group B it decreased from 9.1 to 2.7. Point to point analyzing showed that pain amount has no significant differences in the minutes 15 and 60 after intervention, however, statistically, there were significant differences in the pain score of time point of minutes 30 and 45 after intervention (Table 2). Moreover vital signs including blood pressure and breath rate have no differences between the groups.
| Variables | Time | Morphine (n = 56) | Morphine + Chlorpheniramine (n = 56) | P Value |
|---|---|---|---|---|
| Pain score | Before intervention | 8.5 | 9.1 | 0.70 |
| 15 min after intervention | 6.4 | 7 | 0.33 | |
| 30 min after intervention | 5.2 | 6.5 | 0.01 | |
| 45 min after intervention | 3.2 | 4.1 | 0.02 | |
| 60 min after intervention | 2.1 | 2.7 | 0.12 | |
| Nausea and vomiting, % | 57 | 90 | 0.001 |
The most common drugs adverse effects including nausea and vomiting were evaluated and compared between the groups. The patients receiving morphine along with chlorpheniramine showed less incidence of nausea and vomiting against those receiving morphine alone (Table 2). The patients who received morphine rescue dose after minute 60 after initial intervention in trial group A were more than group B, which was statistically significant (P = 0.04).
4. Discussion
Cholelithiasis is a common disease and a prevalent etiology of emergency department referrals with a prevalence proportion of 5.7% in Iran (1). The incidence of renal colic was increased in the past decades, it may be due to changes in the general population life style (9). Urgent and influential medications consist of spasmolytic drug and opioids.
The current most frequently used agents for pain relieving of patients with renal colic are pethidine and morphine (3). Prescribing opioids make some challenges in emergency departments for their interferes with evaluating the level of consciousness, and possible need for continuous monitoring (10). Therefore, this investigation focused on the ways that limits use of such drugs. This was the reason for designation of the current trial.
Our findings indicated that the patients in group A and B showed a significantly decrease in the pain score. However, the pain score in the time points of 30 and 45 in group A was significantly less than group B. This results suggest that using Chlorpheniramine along with Morphine can be more effective that morhpine alone in managing patients with acute renal colic. After determination of histamine receptors in ureter by Bertaccini et al. it has been suggested that they can make peristalsis effect during renal colic (7). After that, use of histamine 1 receptor antagonists in management of patients with renal colic were evaluated. Yilmaz et al. in a double blind randomized study, evaluated the pain reliving efficacy of histamine 1 receptor antagonist in patients with renal colic. They divided 86 patients with urinary system stones into 2 groups; group 1 received 50 mg intramuscular (IM) dimenhydrinate and group 2 received placebo consist of only 2 cc intramuscular isotonic saline. They conclude that dimenhydrinate is effective in relieving renal colic pain, nausea, as well as vomiting (11). One of the most causes of renal colic pain is usually associated to the ureter soft muscle contraction due to the presence of stones (12). Ugaily-Thulesius et al. showed that extra histamine is related to high frequency of contractions in utterer. Furthermore, they showed that under pathological conditions such as renal colic mast cells of ureters releases histamine, which lead to contraction and consequent pain (13). In another study they showed that urothelial damage in ureteral stone can penetrate subepithelially and make degranulation of mast cells mediators that includes histamines (14).
Collectively, these results indicated that Chlorpheniramine may block histamine receptors on ureter cells and subsequently decreases the peristaltic contractions in the ureter. Moreover the results showed that use of Chlorpheniramine are in relation with lowering incidence of nausea and vomiting and also decreases the morphine needed dose. We conclude that additional chlorpheniramine can lower the needed dose for opioids and can probably diminish the opioids adverse effects.