1. Background
Injury and mortality resulting from snakebites pose significant public health challenges, particularly in tropical regions, although these incidents occur globally. Annually, there are approximately 5.4 million reported cases of snakebites, with 1.8 to 2.7 million envenomings, leading to around 81,000 to 138,000 fatalities worldwide. Most snakebites are observed during the summer months, correlating with heightened human and snake activities (1). Based on a report in tropical regions, the number of snakebite victims who die unregistered in the community is threefold higher than hospital-recorded deaths. This finding suggests that hospital visits do not cover all snakebite patients, and the statistics of snakebites are higher than those reported in official records (2).
The World Health Organization (WHO) has acknowledged snakebite envenoming as a critical health issue and classified it as a high-priority neglected disease that necessitates prompt medical intervention in facilities equipped with effective antivenoms, sufficient bed capacity, and appropriately trained medical staff (3, 4). Snakebite envenoming can lead to severe consequences, including fatalities, long-term physical disabilities (such as amputations, blindness, and renal failure), as well as psychological effects like post-traumatic stress disorder (PTSD) (5). The financial burden of these outcomes is profound, entailing both direct treatment costs and indirect losses due to diminished income (6).
Despite the high incidence of snakebites, access to effective, affordable treatment remains a persistent medical challenge, particularly in developing regions (7). Even though snakebite occurrences are frequent, snake antivenoms are still not readily and sufficiently available, especially in the developing regions of the world (8). In light of the urgency for effective management, the application of fresh frozen plasma (FFP) as a clotting factor replacement therapy has been suggested to minimize catastrophic hemorrhagic risks. However, apprehensions exist that the infusion of clotting factors might exacerbate coagulopathy by providing additional substrates for procoagulant toxins in the venom (9, 10). Additionally, the use of blood products carries inherent risks such as transfusion reactions or viral transmission, with increasing awareness of adverse effects linked to FFP (9).
On the other hand, there are several conflicting recommendations on the use of antibiotics in snakebite victims (11-13). The application of antibiotics in managing snakebite cases generates conflicting guidelines; some recommend routine prophylactic treatment post-envenomation (11, 13), while others argue that antibiotics should only be administered in the presence of clinical infection signs, such as local tissue necrosis, gangrene, abscess formation, or bullae (13). The literature suggests that broad-spectrum antibiotics, including ciprofloxacin, amoxicillin/clavulanate, piperacillin (13), penicillin (13, 14), and ceftriaxone (15), are suitable options for empirical or definitive treatment, with consideration for surgical intervention in cases of invasive soft tissue infections.
Iran is home to a diverse array of venomous snake species, with the most medically significant belonging to the Viperidae family, such as Vipera lebetina, Echis carinatus, Pseudocerastes persicus, and Vipera albicornuta, as well as the Elapidae family, particularly Naja oxiana. Each of the 31 provinces of Iran hosts at least one venomous snake species, and several provinces harbor multiple species, rendering snakebites a substantial health risk, especially in the rural southern and southwestern regions (16). The presence of notable species such as Ophiophagus hannah, P. persicus, E. carinatus, and M. lebetina in the Khuzestan province highlights the need for ongoing research and public education on the significance and risks associated with these creatures. By fostering a better understanding of venomous snakes, we can promote coexistence and ensure the conservation of these fascinating animals within their natural habitats. The ecological environment of Khuzestan supports the survival of these species and also plays a crucial role in their behavioral adaptations and interactions within their habitats (16-19).
2. Objectives
Based on this information, the present study aims to examine the statistics of snakebites during the summer of 2019 at Razi and Abouzar Hospitals in Ahvaz. Additionally, we analyzed the demographic and clinical characteristics, treatments received, necessity of hospitalization and surgery, as well as the recovery and mortality rates of snakebite patients.
3. Methods
3.1. Patients
This descriptive-analytical epidemiological study was conducted under the supervision of the Ethics Committee of Jundishapur University of Medical Sciences in Ahvaz (IR.AJUMS.REC.1400.330). Informed consent was obtained from all participants. This hospital-based cross-sectional study targeted the statistical population, including all adults (≥ 13 years) suffering from envenomation snakebites who visited Razi Hospital in Ahvaz, as well as all children (≤ 12 years) with envenomation snakebites who attended Abouzar Hospital in Ahvaz during the summer of 2019.
Patient data, including age, gender, place of residence, initial symptoms, the time between the bite and hospital admission, the number of antibiotics administered, the necessity for ICU admission and its duration, surgical interventions, dressings, and mortality rates, were collected through interviews with patients and by reviewing archived records. These data were documented in designed questionnaires. The criteria for ICU admission included severe laboratory abnormalities such as coagulation disorders and thrombocytopenia, underlying diseases like heart attacks, strokes, and cancer diagnoses, as well as bed availability.
Two Iranian antivenom brands, Polyvalent and Snafb, were randomly administered to patients, and the dosage of each was carefully recorded. Polyvalent antivenom, produced by the Razi Institute, has been the primary treatment option for many years, effectively targeting the venom of six common Iranian snake species. Snafb antivenom, manufactured by Padra Serum, gained recognition when the company was listed among the serum manufacturers of the WHO in 2021. Its development, production, and approval were a collaborative effort between the Poisoning Department of Jundishapur University and Razi Hospital of Ahvaz.
Informed consent forms were signed by the patients or the parents of affected children. The sole criterion for inclusion in the study was a venomous snakebite, while the only exclusion criterion was incomplete medical records.
3.2. Statistical Analysis
Data analysis was performed using SPSS version 26 statistical software (SPSS Inc., Chicago, IL, USA). The mean and standard deviation were calculated for quantitative variables, while absolute and relative frequencies were determined for qualitative variables. Appropriate parametric or non-parametric tests were selected based on the data type and distribution analysis, utilizing the Kolmogorov-Smirnov and Shapiro-Wilk tests. The findings were examined using the Mann-Whitney U test, Fisher’s exact test, and Spearman correlation analysis. A significance level was set at a P-value cutoff of 0.05. The results were published with overall and acceptable accuracy, maintaining the confidentiality of patient information.
4. Results
Based on the results of the Shapiro-Wilk and Kolmogorov-Smirnov tests, the distribution of data related to quantitative variables was not normal (P < 0.05). Consequently, the tests used in subsequent stages of statistical evaluations were selected according to this type of dispersion. Of the total 90 snakebite cases during the three months of summer 2019, 68 individuals (75.6%) were adults, and 22 individuals (24.4%) were children (Table 1 and Figure 1A). The ages of the subjects ranged from 2 to 48 years, with a mean age of 26.93 years and a standard deviation of 16.42 years. The mean age for adults and children was estimated at 33.92 ± 12.54 years and 7.40 ± 3.67 years, respectively.
| Variables | Statistics | P-Value |
|---|---|---|
| Categories | - | |
| Child | 22 (24.4) | |
| Adult | 68 (75.6) | |
| Age (y) | ||
| All participants | 26.92 ± 16.417 (2 - 84) | |
| Child | 7.40 ± 3.67 | |
| Adult | 33.92 ± 12.54 | |
| Gender | 0.056 | |
| All participants | ||
| Male | 67 (74.4) | |
| Female | 23 (25.6) | |
| Child | ||
| Male | 13 (59.1) | |
| Female | 9 (40.9) | |
| Adult | ||
| Male | 54 (79.5) | |
| Female | 14 (20.6) | |
| Location | 0.025 b | |
| All Participants | ||
| Rural | 66 (73.3) | |
| Urban | 24 (26.7) | |
| Child | ||
| Rural | 20 (90.9) | |
| Urban | 2 (9.1) | |
| Adult | ||
| Rural | 46 (67.6) | |
| Urban | 22 (32.4) | |
| Snake type | 0.756 | |
| All Participants | ||
| Unknown | 89 (98.9) | |
| Known | 1 (1.1) | |
| Child | ||
| Unknown | 22 (100) | |
| Known | 0 (0.00) | |
| Adult | ||
| Unknown | 67 (98.53) | |
| Known | 1 (1.47) | |
| First manifestation | - | |
| Swelling | 32 (35.6) | |
| Pain | 36 (40.0) | |
| Bleeding | 4 (4.4) | |
| Warmth | 1 (1.1) | |
| Erythema | 4 (4.4) | |
| Nausea/vomiting | 3 (3.3) | |
| Burning | 14 (15.6) | |
| Bruising | 1 (1.1) | |
| Fever/chills | 4 (4.4) | |
| Time interval to treatment (h) | 0.820 | |
| All participants | 10.98 ± 11.73 (0.3 - 48) | |
| Child | 7.84 ± 7.55 | |
| Adult | 11.99 ± 12.67 | |
| Hospitalization duration (d) | 0.001 b | |
| All participants | 2.82 ± 1.88 (1 - 10) | |
| Child | 3.86 ± 2.25 | |
| Adult | 2.47 ± 1.61 | |
| ICU necessity | 0.003 b | |
| All participants | ||
| Yes | 19 (21.1) | |
| No | 71 (78.9) | |
| Child | ||
| Yes | 0 (0.00) | |
| No | 22 (100) | |
| Adult | ||
| Yes | 19 (27.9) | |
| No | 49 (72.1) | |
| ICU hospitalization (d) | - | |
| 1 | 3 (3.3) | |
| 2 | 11 (12.2) | |
| 3 | 4 (4.4) | |
| 4 | 1 (1.1) | |
| Antivenom vials used number | 0.206 | |
| All participants | 7.99 ± 5.21 (1 - 24) | |
| Child | 6.59 ± 2.89 | |
| Adult | 8.58 ± 5.85 | |
| Antibiotics used amount | 0.00 b | |
| All participants | ||
| Ceftriaxone | 53 (58.9) | |
| Gentamycin | 1 (1.1) | |
| Gentamycin/penicillin 17 | (18.9) | |
| Gentamycin/penicillin/ceftriaxone | 1 (1.1) | |
| Child (19 of 22) | ||
| Ceftriaxone | 0 (0.00) | |
| Gentamycin | 1 (5.3) | |
| Gentamycin/penicillin | 17 (89.5) | |
| Gentamycin/penicillin/ceftriaxone | 1 (5.3) | |
| Adult (53 of 68) | ||
| Ceftriaxone | 53 (100) | |
| Gentamycin | 0 (0.00) | |
| Gentamycin/penicillin | 0 (0.00) | |
| Gentamycin/penicillin/ceftriaxone | 0 (0.00) | |
| Therapeutic/surgical procedures | 0.00 b | |
| All participants | ||
| No procedure | 79 (87.8) | |
| FFP | 8 (8.9) | |
| Dressing | 3 (3.3) | |
| Child | ||
| No procedure | 12 (54.6) | |
| FFP | 7 (31.8) | |
| Dressing | 3 (13.6) | |
| Adult | ||
| No procedure | 67 (98.5) | |
| FFP | 1 (1.5) | |
| Dressing | 0 (0.00) | |
| Mortality rate | ||
| Alive | 90 (100) | |
| Died | 0 (0.00) |
Abbreviation: FFP, fresh frozen plasma.
a Values are expressed as No. (%), mean ± SD or mean ± SD (range).
b A P-value of < 0.05 is considered statistically significant.
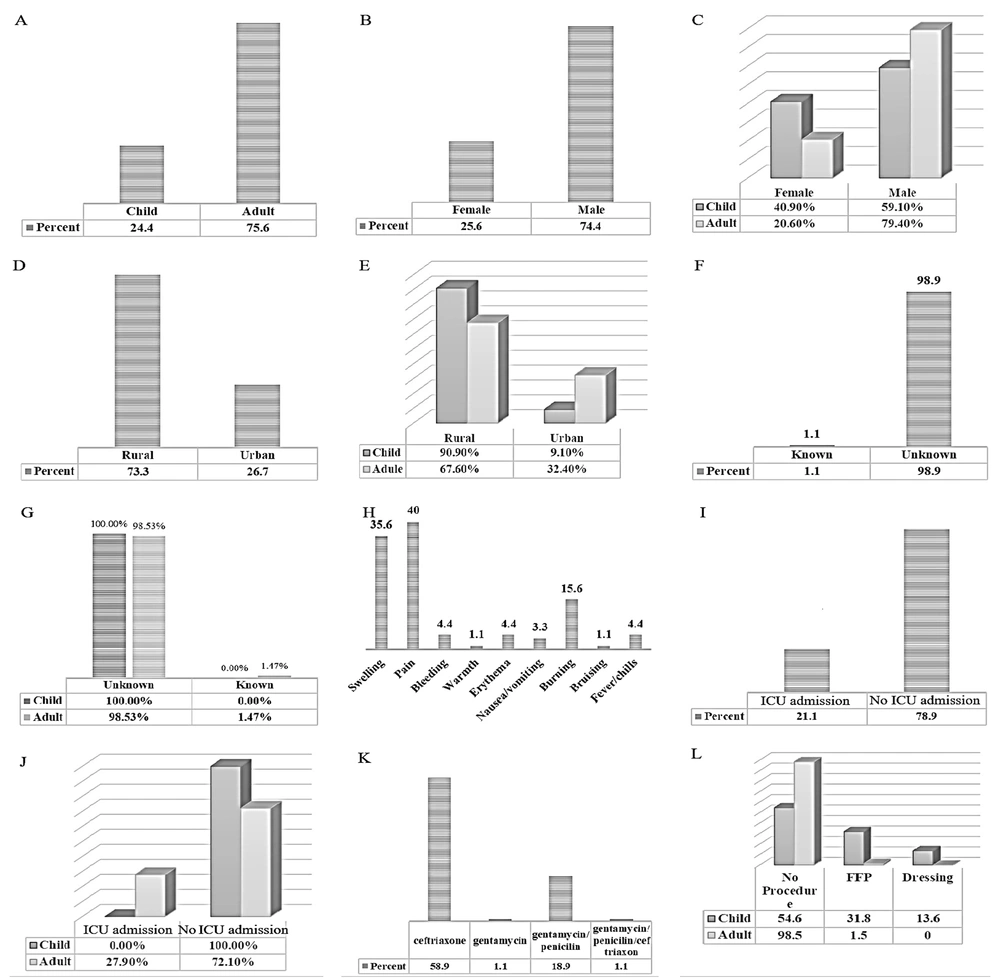
Demographic and clinical features of patients. A, frequency of patients in child and adult age categories; B, frequency of patients in male and female sex categories; C, frequency of child and adult patients in male and female sex categories; D, frequency of patients in rural and urban location categories; E, frequency of child and adults patients in rural and urban location categories; F, frequency of snakes in known and unknown categories; G, frequency of child and adults patients in known and unknown snake categories; H, frequency of first clinical manifestations; I, frequency of ICU admission; J, frequency of child and adults patients in ICU admissions; K, frequency of used antibiotics; L, frequency of treatment procedures.
Most of the victims were men, totaling 67 (74.4%), while women numbered 23 (25.6%). The gender distribution of the injured did not show a significant difference based on age group (P = 0.056) (Table 1 and Figure 1B and C). Most of the injured resided in rural areas of the province (66 individuals, 73.3%). By age group, the majority of adult victims were 46 (67.6%), while child victims numbered 20 (90.9%) residing in rural areas. However, the frequency of rural child victims was significantly higher than that of urban victims (P = 0.025) (Table 1 and Figure 1D and E).
In most cases of snakebite in the studied population, the species of the biting snake was not identified, accounting for 89 individuals (98.9%) of the total 90 victims. There was only one reported case of snakebite by E. carinatus among adults, as the victim brought the snake’s corpse (Table 1 and Figure 1F). The difference between children and adults regarding the identification of snake species was not significant (P = 0.756) (Table 1 and Figure 1G).
In terms of initial manifestations of the disease, pain was reported in 36 individuals (40%), swelling in 32 individuals (35.6%), and burning in 14 individuals (15.6%) among the examined patients (Table 1 and Figure 1H). The time interval from the bite to hospital admission ranged from 0.3 to 48 hours, with a mean of 10.98 hours and a standard deviation of 11.73 hours. The average time interval for adults was higher than that for children, but this difference was not significant (P = 0.820) (Table 1).
The mean duration of hospitalization for patients ranged from 1 to 10 days, with a mean of 2.82 days and a standard deviation of 1.88 days. The average length of stay for adults was significantly less than that for children (P = 0.001) (Table 1). The need for ICU admission was observed in 19 individuals (21.1%). It was also found that the need for ICU admission in adults was significantly higher than in children (P = 0.003) (Table 1 and Figure 1I and J). The number of ICU hospitalization days for patients requiring this type of admission is presented in Table 1.
The number of antivenom vials ranged from 1 to 24, with a mean of 7.99 and a standard deviation of 5.21. There was no significant difference in the mean number of antivenom vials consumed between adults and children (P = 0.206) (Table 1). In 18 individuals (20%) of the total cases, antibiotics were not used. Out of 22 children, 19 received antibiotics, while out of 68 adults, 53 received antibiotics. Ceftriaxone was the most commonly administered antibiotic among the studied samples, with a frequency of 53 individuals (58.9%). In children, gentamycin/penicillin was used in 17 individuals (89.5%), which was the most frequently administered treatment, while in adults, ceftriaxone was used in 53 individuals (100%) (P = 0.00) (Table 1 and Figure 1K).
The frequency of FFP and dressings was reported in 8 individuals (8.9%) and 3 individuals (3.3%), respectively, showing a significant difference between adults and children; the frequency of FFP and dressing in children was 31.8% and 13.6%, respectively. In adults, these rates were reported at 1.5% and 0%, respectively (P = 0.00) (Table 1 and Figure 1L). No fatalities were reported in the studied population (Table 1).
According to the results of the Spearman correlation test, no significant correlation was observed between the age of individuals and the number of antivenom vials consumed (P = 0.853). The Mann-Whitney test did not report a significant correlation between the mean number of antivenom vials consumed and the gender of the patients (P = 0.691). The findings obtained from the Kruskal-Wallis test indicated no significant relationship between the number of antivenom vials consumed and the type of the causal snake (P = 0.147). Findings from the Kruskal-Wallis test also showed no significant correlation between the type of snake involved in the bite and the age of the individuals affected by snakebites (P = 0.908). The chi-square test did not report a significant relationship between the type of snake involved in the bite and the type of antibiotic administered (P = 0.985). These demographic trends align with global patterns observed in tropical regions.
5. Discussion
Bites and stings are among the most significant health-related problems, imposing substantial costs on the healthcare system each year. Snakebites, as a considerable public health challenge, are often overlooked, especially in rural communities across tropical and subtropical regions of the world. Despite the high prevalence of these incidents, precise epidemiological data on snakebites have not been provided (20). Recent findings indicate that global warming is leading to an increase in the number of venomous snakebites (21). A recent study shows that for every degree Celsius increase in daily temperature, the incidence of snakebites rises by nearly six percent. Researchers have stated that climate change contributes to increased activity among cold-blooded animals, such as snakes (22). Considering the climatic conditions of Ahvaz city and the high temperatures during the hot seasons that increase the activity of venomous cold-blooded animals (23, 24), this study investigates the epidemiology of snakebites among adult patients visiting Razi Hospital and pediatric patients visiting Abouzar Hospital in Ahvaz during the summer of 2019.
As presented in the results section, the majority of snakebite cases in our study were among adults (75.6%). The victims were aged between 2 and 84 years, with a mean age of 26.92 years. The mean ages for adults and children were reported to be 33.92 ± 12.54 years and 7.40 ± 3.67 years, respectively. In the study by Levine et al., out of a total of 420 snakebite cases that occurred between 2013 and 2017, only 22.4% of the patients were children. This finding is consistent with the present study, which reported that adults were the age group most likely to be bitten by snakes (25).
In a comprehensive study carried out by our research team from 2018 to 2020, we investigated the cases of children suffering from snakebites who were referred to Abouzar Hospital in Ahvaz. The findings revealed that the average age of the victims was 10.73 years, with a standard deviation of 3.41 years (26). In the descriptive study by Mohammadi Kojidi et al., the mean age of the victims was 43.14 years (27). This figure is higher than the mean age obtained in our study, possibly because only patients from Rasht city were included in their study. In our study, the lower mean age may be attributed to the high incidence of snakebites among rural children.
In alignment with the current study, the research by Esmaeil et al. noted that the majority (34.3%) of snakebite victims were in the age group of 20 - 29 years (28). In the study by Tekin et al., 42.4% of snakebite victims were children (3), whereas this figure was 24.4% in the present study. In the study by Zamani-Alavijeh et al., the mean age of patients was reported as 28.26 ± 0.36 years, with the highest frequency of bites occurring in the 21 - 30 year age group (27%) and the lowest in individuals over 80 years old (less than 1%) (29).
In Brazil, Feitosa’s study identified that the majority of snakebite victims fell within the age group of 16 to 45 years (30). Conversely, a study by Mohapatra et al. in India found that the peak incidence of snakebites occurred among individuals aged 15 to 29 years (31). Meanwhile, Tekin and his team in Turkey categorized most of their patients as adults (3). These observations align with the results of the current study.
In our study, males constituted 74.4% of victims, consistent with prior studies, which reported 71% in Mohammadi Kojidi et al. (27) and 60.5% in Kshirsagar et al. (32). However, Zamani-Alavijeh et al. (29) reported a lower proportion of 45%, potentially reflecting regional demographic differences. The study by Feitosa et al. indicated that 79% of snakebite victims were male (30). Mohapatra et al.’s study observed a lower figure of 59%, although men still experienced a higher prevalence of snakebites compared to women (31). Similarly, Tekin et al.’s study reported that 64% of the patients were male (3). The results obtained in our study align with the general findings regarding the higher incidence of snakebites among males. However, the observed differences in the age and gender distribution of victims may be attributed to various factors, including climatic, cultural, and employment variations between men and women in the studied community.
In the present study, most of the victims resided in rural areas of the province. The total number of rural residents was 66 individuals (73.3%), including 46 adults (69.7%) and 20 children (30.3%). In the study by Esmaeil et al., all cases occurred in rural areas, which aligns with the higher incidence of snakebites among rural residents found in the current study (28). In contrast, Zamani-Alavijeh et al. reported that 93.3% of snakebite cases occurred in urban areas, with most (99.7%) occurring at home (29). Furthermore, both Feitosa et al. (30) and Mohapatra et al. (31) noted that the highest rates of snakebites occurred in rural areas, with the latter study highlighting that rural areas accounted for 97% of snakebite-related fatalities.
Factors contributing to the high incidence of snakebites among rural children in this study include increased activity levels in this age group and their curiosity and risk-taking behaviors, such as moving rocks and playing near snake habitats. Moreover, in rural areas, safety measures such as wearing gloves and checking shoes before putting them on are often overlooked. It is more likely for children to walk barefoot or not wear appropriate footwear (33). Additionally, contributing factors to snakebites in rural settings include the aging of houses, lack of proper infrastructure, sleeping and resting in open environments, and the absence of beds for sleeping.
In the current study, pain was observed in 36 individuals (40%), swelling in 32 individuals (35.6%), and burning in 14 individuals (15.6%) as the most common initial symptoms among the patients examined. In the study by Soleimani et al. (34), the main symptoms reported among victims included pain, swelling, hematuria, and abnormalities in liver enzymes, with a prevalence of 57.3% [Soleimani et al. (34)]. The study by Mohammadi Kojidi et al. noted that the most frequent complications included subcutaneous bleeding (100%) and pain (81%) (27). In the research by Esmaeil et al., all patients exhibited symptoms of pain, swelling, erythema, and ecchymosis, with 40.3% experiencing severe fatigue (28). Additionally, research conducted by Adukauskiene et al. revealed that 70% of snakebite patients reported symptoms of pain and swelling (35).
These discrepancies in findings may stem from factors such as the type of venom from various snake species, the physical resilience of the victims, or the speed of medical response and treatment received. Based on our findings, 98.9% of snakebite cases involved unidentified snake species. This figure was reported as 52.9% in the study by Chew et al. (36). This finding in our study may be due to the high diversity of snakes in Iran, with many individuals lacking prior encounters or familiarity with snakes. Consequently, identifying the snake species requires an understanding of the ecosystem and prior knowledge of snakes. On the other hand, snakebites often induce significant fear and panic, which can impair the focus of the affected individual, making it challenging to identify the type of snake or even recognize its distinguishing features.
In our study, the time interval from snakebite to hospital visit ranged from 0.3 to 48 hours, with a mean of 10.98 hours. The average time interval for adults seeking medical attention was higher than that for children; however, this difference was not statistically significant (P = 0.820). Given the serious complications arising from delays in receiving snakebite treatment, which may include tissue loss due to debridement or surgical removal of necrotic areas (15), limb amputation (37), chronic wounds, infection, osteomyelitis, arthritis, severe physical disability (38-40), and, depending on the type of snake, renal disorders (41), cerebral cortex disturbances (42), chronic neurological deficits (43), psychiatric disorders such as depression (44) and seizures (45), PTSD (45, 46), and chronic musculoskeletal disabilities such as swelling, muscle atrophy, joint stiffness, decreased muscle strength, balance disorders, and permanent deformities (47, 48), it is essential to minimize the time interval between the bite and hospital visit (40).
To this end, implementing educational programs to inform the public about the importance of obtaining prompt treatment following a snakebite is crucial in reducing delays and their consequences. Considering that the majority of cases in this study were from rural areas, the reasons for delays in seeking help may include the remoteness of villages from county centers, inadequate rural roads, lack of available transportation, unawareness of the importance of receiving timely treatment, and financial difficulties faced by rural residents.
The average duration of hospitalization for patients ranged from 1 to 10 days, with a mean of 2.82 days. The mean length of hospitalization for adults was significantly lower than that for children. In our team's prior investigation, we found that the average duration of hospitalization for children who suffered snakebites was 4.05 days, with a standard deviation of 2.13 days (26). The need for ICU admission was observed in 19 individuals (21.1%). Additionally, it was established that the requirement for ICU admission was significantly higher in adults compared to children. In the study by Lang et al., the median length of stay in the intensive care unit (IQR) was reported as 3 days (49), comparable to the figures obtained in the present study.
Since snakebites have been a threat for as long as humans have existed, treatments for them have evolved alongside human civilization (50). In traditional Iranian medicine, initial treatments involved making an incision, scraping, or creating a puncture at the bite site, followed by attempts to suction the venom (51). However, this method posed a risk to the person administering treatment due to potential poisoning from the venom entering their mouth. Another method involved applying a tourniquet to the affected limb (52). This practice is both painful and dangerous, as it can lead to ischemia or the development of necrotic wounds. The use of topical chemical substances or herbs was also a common treatment in ancient remedies (53). However, validating the therapeutic effects of plant materials requires extensive research grounded in modern healthcare practices and global standards.
Cryotherapy, which involves cooling the bite area with ice packs, is another method that carries the risk of exacerbating tissue damage (54). These traditional methods are often long-term treatments and may not be effective within the critical initial period after a bite. Moreover, some can worsen the damage. While controlled cooling may reduce inflammation (55), and certain plants contain active compounds that could alleviate snakebite symptoms, these approaches need proper guidelines and validation. Physical venom extraction, if performed before the venom spreads, is a logical approach but requires tools compliant with global standards (51).
Therefore, regular training and reminders for at-risk populations and clinical staff in Ahvaz are essential to mitigate complications from outdated treatments. Currently, antivenom serum remains the most effective, safe, and reliable treatment.
Based on the current study, the average number of antivenom vials administered ranged from 1 to 24, with a mean of 7.99. The amount of antivenom used in adults did not show a significant difference compared to children. In the study by LoVecchio and DeBus, 50 children who experienced snakebites (87.72%) received antivenom, among whom 19 cases exhibited immediate hypersensitivity reactions (56). In Lang’s study, antivenom was administered to 12.6% of patients hospitalized in the intensive care unit due to snakebites (49).
Antivenom is a crucial treatment for snakebites, as it contains specific antibodies that neutralize the toxic effects of snake venom. The timely administration of antivenom can significantly reduce morbidity and mortality associated with envenomation. Without proper treatment, snakebites can lead to severe complications such as tissue damage, organ failure, and even death. Antivenom helps to alleviate symptoms, prevent the progression of venom-related injuries, and improve overall patient outcomes. Additionally, it plays a vital role in public health, particularly in regions where snakebites are prevalent, ensuring that affected individuals receive essential medical care and reducing the long-term impacts of snakebite injuries.
In our study, 72 individuals (80%) of all patients received antibiotics. The most commonly prescribed antibiotic was ceftriaxone, which was administered to 53 individuals (58.9%), all of whom were adults. For children, gentamicin/penicillin was used for 10 individuals (52.6%), making it the most prevalent treatment in this age group. Although there are guidelines for managing snakebite envenomation, the use of antibiotics in this context remains controversial. Various studies reported different types of antibiotics utilized in snakebite cases, ranging from beta-lactams to lincosamides and nitroimidazoles, and from monotherapy to combination antimicrobial therapies. Antibiotics should be prescribed cautiously and carefully. Prophylactic use of antibiotics has been reported as prohibited in most studies (57).
Scientifically, the administration of antibiotics in snakebite cases should be based on the susceptibility of microorganisms isolated from the affected tissue or identified in the snake’s oral cavity (57, 58). However, this was not feasible in the present study due to the lack of precise identification of snake species and the limited opportunity for identifying microbial species at the wound site. Therefore, the high rate of antibiotic consumption observed in this study was due to precautionary measures taken and the consideration of the potential risk of infection.
The frequency of FFP and dressing was reported in 8 individuals (8.9%) and 3 individuals (3.3%), respectively, with a significant difference between the adult and pediatric groups. Specifically, the frequency of FFP and dressing in children was 31.8% and 13.6%, respectively. In adults, these figures were 1.5% and 0%, respectively. In snakebite incidents without timely intervention, the healing of certain wounds can be challenging and even life-threatening. The WHO has provided official guidelines for managing snakebite wounds with severe complications, such as large blisters and skin necrosis. However, there is no standardized protocol for the emergency management of common snakebite wounds. Moreover, the types of snakes and venom characteristics vary by country and region, leading to diverse wound treatment methods (598).
Dressings with various active ingredients (60-62) and FFP treatment (63) have been reported in different studies. Fresh frozen plasma is the liquid component of a unit of whole blood frozen within a specified time frame, typically 8 hours. The FFP contains all coagulation factors except platelets, and it does not include red blood cells or leukocytes. Fresh frozen plasma corrects coagulation by replacing or supplementing plasma proteins in patients with deficient or dysfunctional plasma proteins. The standard dosage is 10 to 20 milliliters per kilogram, which increases factor levels by approximately 20% (64).
In the present study, FFP was not utilized, except for patients who were in emergency conditions and received FFP before being referred to our center. In a study by Holla et al., all 62 patients examined were administered an average of 5 units of FFP, with 6 of these patients experiencing adverse reactions to this treatment. These reactions included chills and pain at the infusion site (63).
In the present study, the mortality rate was zero. In the study conducted by Kshirsagar et al., a mortality rate of 1.85% was reported among patients who presented late to the hospital (32). The mortality rate of 8% in the Lang et al. study may be attributed to the fact that their cases were selected from ICU patients (49).
The findings from our study indicated that most snakebite victims are adults, predominantly males, and individuals residing in rural areas. In many cases, the species of the snake responsible for the bite was unknown. More than one-fifth of the victims required admission to the ICU. Swelling, pain, and a burning sensation were the most common initial symptoms observed in patients. The average duration of hospitalization for adults was significantly shorter than that for children. In one-fifth of the cases, antibiotics were not utilized. Among children, gentamicin/penicillin was the most frequently used treatment, while ceftriaxone was more commonly administered to adults. The frequency of FFP and dressing interventions in children was higher than in adults. No fatalities were reported.
Therefore, it seems that even in areas with limited healthcare systems, prompt hospital visits could allow for patient recovery and minimize complications. Public media campaigns for personal protective education, especially in rural areas, could effectively reduce cases of bites and venomous stings. Moreover, training and retraining healthcare personnel can strengthen prevention and optimal treatment strategies.
Similar studies to the present one have rarely been conducted in Iran, which limits the ability to make accurate comparisons and conclusions. Due to the high rate of unknown snake species, further investigations into the relationship between the treatment used and the species of snake responsible for the bite are necessary. It is essential to plan and implement additional studies with a larger time scale and the consideration of more independent and intervening variables to confirm or refute the present results.
5.1. Strengths and Limitations
This study provides valuable insights into snakebite statistics in Ahvaz, Iran. Concentrating on Ahvaz allows for a detailed examination of snakebite patterns within a particular ecological and healthcare context. This localized approach can yield valuable insights for targeted interventions. The study contributes to the understanding of clinical manifestations and treatment outcomes in a region where snakebites are a significant health concern. Documenting these aspects can aid in developing local clinical guidelines and improving patient care. Despite its limitations, the study adds to the limited body of knowledge on snakebite epidemiology in Iran. The data can be used to inform national-level policies and resource allocation for snakebite prevention and management. Evaluating the types of treatments used and their outcomes, even with incomplete follow-up, can offer preliminary insights into their effectiveness. This information can guide further research and improvements in clinical practice.
Despite these potential strengths, the present study’s conclusions are tempered by certain limitations. The restriction to cases referred to the referral centers introduces a potential selection bias, as it excludes cases managed elsewhere or those that did not seek formal medical care. Additionally, the inability to accurately follow up with patients hinders the determination of long-term complications and the effectiveness of administered treatments. Retrospective data collection on snakebite incidents can be subject to recall bias, affecting the accuracy of reported clinical symptoms and treatment details. Reliance on patient history and records may not fully capture the nuances of each case. The study may not fully detail the range and severity of clinical manifestations due to limitations in data granularity. Variations in venom toxicity among different snake species in the region could lead to a wide array of clinical presentations that may not be fully captured. Complete mortality data may be challenging to obtain, especially for cases that do not present to the study centers.