1. Background
Epilepsy is one of the major neurological disorders in humans, and it involves about 0.5 - 1.0% of the population in the world (1). Inflammatory reactions occur in the brain in various central nervous system (CNS) disorders, including neurodegenerative, autoimmune, and epileptic diseases. Anti-inflammatory and pro-inflammatory cytokines and related molecules have been shown in the plasma and CNS of clinical epileptic cases and experimental models of seizures (2). Evidence shows that the roles of inflammation in the initiation of seizures and epileptogenesis are as follows: a) seizures and status epilepticus induce the production of pro-inflammatory cytokines and inflammatory mediators, b) systemic inflammation can affect the integrity of the blood–brain barrier (BBB), enhance the excitability of neurons, and decrease the seizure threshold, c) disruption of the BBB by inflammatory processes may induce epileptogenesis through the disturbance of brain homeostasis, and d) several anti-inflammatory drugs have been reported to exert antiepileptic actions (2-7). Cyclooxygenases (COXs), the key enzymes that convert arachidonic acid to prostaglandins (PGs), have been implicated in physiological and pathophysiological functions in the CNS. Non-steroidal anti-inflammatory drugs (NSAIDs) known as COX inhibitors are commonly used for treating fever and pain state and for the prevention of and therapeutics of many diseases. However, the role of PGs and NSAIDs in the seizure activity is controversial (8). Cyclooxygenase-2 (COX-2) activity produces oxidative stress and results in the production of PGs, which have many destructive effects. The transcription of COX-2 has been reported to be induced by synaptic activity and that COX-2 could play a significant role in the pathogenesis of epilepsy (9). Meloxicam is a U.S. food and drug administration-approved drug for rheumatoid arthritis and osteoarthritis (10). Meloxicam is derived from enolic acid and is a potent inhibitor of PG biosynthesis under inflammatory conditions with preferential COX2 inhibitory activity. Prostanoid release in the brain was shown to have been reduced by 20% - 30% by meloxicam (11, 12). The drug has shown to cause improved gastric and renal tolerability and higher therapeutic index both experimentally and clinically than conventional NSAIDs (10). Moreover, the potential antioxidant activity of meloxicam was found (13, 14). Meloxicam attenuated oxidative stress probably by alleviating lipid peroxidation and improving the antioxidant defense system (15). However, this study aimed to investigate the effects of meloxicam on PTZ and MES-induced seizures in mice.
2. Methods
2.1. Experimental Animals
Male C57 albino mice born and reared in the research center and experimental animal house at the Ahvaz Jundishapur University of Medical Sciences were used in the present study. Young healthy male mice weighing between 24 g and 28 g were housed and maintained at a temperature (23 ± 2 °C)- and humidity (50 ± 10%)- controlled environment under a 12 hours light/dark cycle with alternating food and water, except for a short time when they were removed from their cages for testing. To minimize circadian changes and inter-group variations, all the experiments were conducted between 08:00 a.m. and 14:00 p.m.. Animal testing was carried out in accordance with the institutional guidelines for animal care and use, and all possible measures were taken to minimize the number of animals used. Animals were acclimatized to the new conditions for at least 1 hour before testing.
2.2. Drugs, Chemicals, and Solutions
The following drugs were used in the present study: meloxicam (Iran-Hormun, Iran), PTZ (Sigma-Aldrich, USA), phenytoin (HIDANTIC, Caspian Tamin, Iran), and diazepam (ZEPADIC, Caspian Tamin, Iran). All chemicals were dissolved in 0.9% saline except meloxicam, which was suspended in normal saline containing 0.025% Tween-80. Drug solutions were prepared fresh, and the selected doses were administered in 10 ml/kg animal body weight. The doses of meloxicam were selected on the basis of previous studies on mice and our preliminary observations (16).
2.3. Pentylenetetrazole-Induced Seizures Test
Mice were divided into six groups each containing eight animals: vehicle (group I), diazepam (group II) at a dose of 1 mg/kg, i.p., and groups III-VI meloxicam (2.5, 5, 10, and 20 mg/kg, i.p.), respectively. Thirty minutes later, seizures were induced by the PTZ (85 mg/kg, i.p.). The animals were observed during the first 30 min to evaluate latency for convulsion, Straub’s tail, onset of myoclonic seizures, and protection against mortality.
2.4. Maximal Electroshock (MES)-Induced Seizure Test
Mice were divided into six groups each containing eight animals and treated with vehicle, phenytoin (25 mg/kg, i.p.), and meloxicam (2.5, 5, 10 or 20 mg/kg, i.p.), respectively. Thirty minutes later, seizures were induced by a current stimulus (50 mA, 80 Hz for 0.2 seconds) delivered using ear electrodes by an electroconvulsometer (Borjsanat Company, Iran). To improve electrode contact, the electrodes were moistened with normal saline before they were attached to the ears of mice (17, 18). The current used was predetermined before experimentation. The current that caused hindlimb tonic extension (HLTE) and death did not occur in all mice in the control trials. The duration of HLTE (i.e., the hindlimbs of animals outstretched at 180° to the plane of the body axis) was recorded. Protection was defined as the complete absence of HLTE.
2.5. Rotarod Test
The ataxic behavior of mice was evaluated in the accelerating rotarod test. Mice were placed with the four paws on a 6 cm diameter rod revolving at 12 rpm exactly 25 cm above the floor. Mice were trained to remain on the rod for three consecutive trials of 1 minute each. On the next day, all animals in a group received either vehicle, diazepam (1 mg/kg), phenytoin (25 mg/kg, i.p.), or meloxicam. After 30 minutes, each animal was placed on the rod for 1 minute to confirm the absence of any motor coordination disorder.
2.6. Statistical Analysis
All the results were presented as mean ± SEM. Latency to induce convulsive behavior by the PTZ and MES was analyzed by one-way analysis of variance (ANOVA) followed by post hoc Tukey’s test for comparison. P values less than 0.05 were considered significant.
3. Results
3.1. Effect of Meloxicam on PTZ-Induced Seizures
In PTZ-induced seizures, the administration of meloxicam at doses of 5 and 10 mg/kg increased the latency for convulsion, Straub’s tail, and myoclonic seizure compared with the vehicle (P < 0.05). Meloxicam and diazepam showed significant protection against mortality induced by seizures. Diazepam (1 mg/kg, i.p.)-treated animals did not show any signs of convulsions and protected all the mice from PTZ-induced convulsions (Table 1).
| Treatment | Dose, mg/kg | No. | Latency for Convulsion, s | Latency for Straub’s Tail, s | Latency for Myoclonic, s | Protection of Mortality, % |
|---|---|---|---|---|---|---|
| Vehicle | 10 mL/kg | 8 | 45.25 ± 2.54 | 53.25 ± 2.20 | 65.5 ± 2.75 | 0 |
| Diazepam | 1 | 8 | 228.3 ± 10.4*** | 1200 ± 0.0 | 1200 ± 0.0 | 100% |
| Meloxicam | 2.5 | 8 | 52.625 ± 1.90 | 61.25 ± 2.49 | 70.875 ± 3.60 | 50% |
| Meloxicam | 5 | 8 | 60.625 ± 2.64* | 68.75 ± 1.64* | 79.5 ± 3.73* | 62.5% |
| Meloxicam | 10 | 8 | 75.5 ± 3.32* | 84.625 ± 2.87* | 107.375 ± 4.11* | 75% |
| Meloxicam | 20 | 8 | 51.625 ± 2.02 | 56.5 ± 1.34 | 63.75 ± 1.82 | 12.5% |
aValues are expressed as mean ± SEM.
bData were analyzed by one-way ANOVA followed by Tukey’s HSD multiple comparison test, *P < 0.05, ***P < 0.001 compared with the vehicle group.
3.2. Effect of Meloxicam on MES-Induced Seizures
In the MES model, phenytoin prevented the occurrence of HLTE in mice, and meloxicam at any dose did not change the duration of HLTE compared with the untreated control group. Furthermore, meloxicam at all applied doses worsened the condition of mice and caused their mortality (Table 2).
| Treatment | Dose, mg/kg | No. | Hindlimb Tonic Extensions, s | Mortality, % |
|---|---|---|---|---|
| Vehicle | 10, mL/kg | 8 | 14.62 ± 0.59 | 0 |
| Phenytoin | 25 | 8 | 0.0 ± 0.0 | 0 |
| Meloxicam | 2.5 | 8 | 16.5 ± 0.45 | 25% |
| Meloxicam | 5 | 8 | 14 ± 0.53 | 12.5% |
| Meloxicam | 10 | 8 | 16.5 ± 0.56 | 25% |
| Meloxicam | 20 | 8 | 16 ± 0.59 | 12.5% |
3.3. Rotarod Test
Treatment with meloxicam, diazepam (1 mg/kg), and phenytoin (25 mg/kg, i.p.) did not influence mice performance in the rotarod test. The effects of these treatments did not alter motor coordination.
4. Discussion
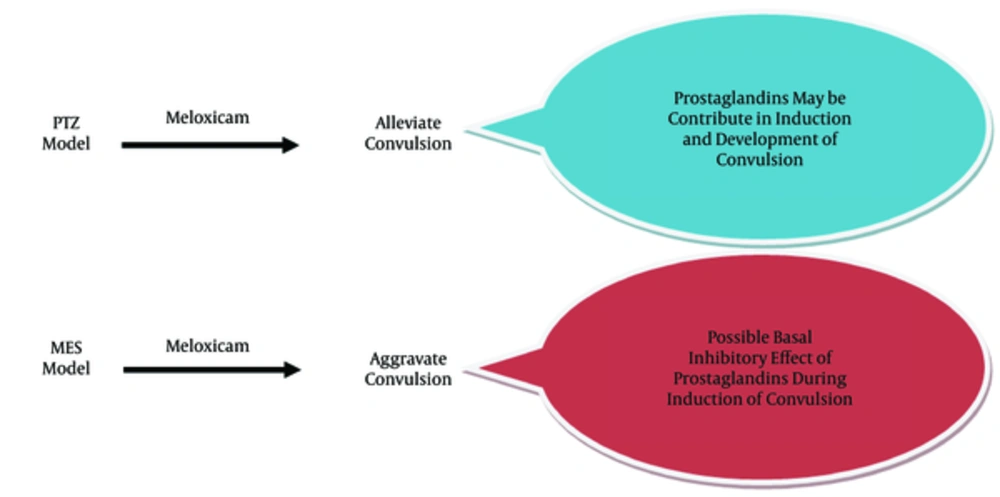
In this study, we applied the differential effects of meloxicam on PTZ- and MES-induced convulsions in mice. Meloxicam can be effective in the type of seizure in the PTZ model. The lowest mortality and reduction in duration of myoclonic seizures was obtained at 10 mg/kg. Thus, this dose is considered the most neuroprotective dose in PTZ-induced seizures in mice. Meloxicam at a high dose (20 mg/kg) decreased latency to convulsive behavior and increased mortality rate (decrease in mortality protection). Thus, the meloxicam effects at a dose of 20 mg/kg were reversed. Clinically effective drugs against PTZ-induced seizure can be used in the treatment of myoclonic and absence epilepsy (19-21). Accordingly, meloxicam can be effective in absence epilepsy. As a convulsive agent, PTZ inhibits GABAA receptors. Therefore, drugs that are agonists at the GABAA site can prevent PTZ-induced seizures. Free radicals aggravate epilepsy by increasing the activity of glutamine synthase (22). One of the most common causes of seizures in humans and animals is decreased GABAergic activity and increased glutaminergic system activity. GABAA receptors are ligand-gated chloride channels that mediate the inhibitory transmission in the synapses. The GABAA receptor function not only prevents the development of epilepsy but also inhibits the development of convulsive activity throughout the cerebral cortex tissues (23). In many reports, COX-2 is involved in some neurological disorders, such as Alzheimer’s disease (24), traumatic brain injury (25), cerebral ischemia (26), and epilepsy (2). Evidence shows that the effect of COX inhibition on seizure activity is highly dependent on many factors, including the nature of the COX inhibitor used (i.e., selective or nonselective) and the experimental model (27). The contribution of COX isoenzymes in the progression and severity of convulsions remains controversial (27). The up-regulation of COX enzyme was shown to occur exclusively in COX-2 isoform following seizure activity (28). COX induction leads to the increase in PGs levels, particularly PGE2, which may facilitate glutamate release from the nerve terminal. This result clarifies the modulator effects of COX inhibitors on glutamate and GABAergic transmission (29). The role of PGs in seizures is known as the PGE2 and PGD2 levels become elevated following PTZ administration (30). Thus, COX inhibitors can be concluded to reduce seizures by inhibiting PG synthesis. Another study showed that meloxicam significantly reduced the increase in brain myeloperoxidase and malondialdehyde levels and restored the glutathione content of the brain (31). COX activation also leads to increased free radical production, which causes oxidative stress, continued apoptosis of GABAergic neurons, and consequently increased glutamate-mediated epileptic discharges (1). COX-2 inhibition up-regulates the expression of GABAA receptors, the main fast inhibitory neurotransmitters in the brain; thus, COX-2 inhibitors decrease neuronal excitability and prevent epileptic seizure (9). However, some results of previous studies on the role of COX-2 in convulsions are controversial. Pre-treatment with COX-2 inhibitors, such as nimesulide, celecoxib, and indomethacin, is known to aggravate kainic acid-induced seizure activity (32). In the current study, meloxicam did not change the duration time of HLTE and surprisingly caused mortality in animals receiving meloxicam. Consistent with our finding, one study indicated that COX inhibitors were ineffective against MES-induced convulsions (33). By contrast, another study on celecoxib, a selective COX-2 inhibitor, showed that celecoxib had beneficial effects when given in combination with phenytoin against electroshock-induced convulsions (34). According to the results of the current study (Figure 1), meloxicam did not have a neuroprotective effect on the MES model of convulsion. As the administration of meloxicam leads to the decreased basal brain level of PGs, the occurrence of death in the MES model of convulsion in animals receiving meloxicam can represent the basal inhibitory effect of PGs during induction and development of convulsion in mice. However, meloxicam in the PTZ model showed a significant anticonvulsive activity. This result indicates that PGs contribute to the induction of convulsions in the PTZ model. However, future studies are required to clarify the effect of NSAIDs on and the role of PGs in the induction and development of convulsion in different models of seizures.