1. Background
The genus Eremostachys is present as the one of the main genera of the Lamiaceae family, which was represented by nearly 60 species that occur mostly in Central Asian countries such as Armenia, Turkmenistan, and USSR. Traditional knowledge showed anti-inflammatory and analgesic effects of rhizomes of various species of Eremostachys (1). Previous investigations reported the other biological properties such as antioxidant, antimalarial, anti-bacterial, antidepressant, and antinociceptive activities (1-6). Phytochemical studies on the extracts of some species of this genus have indicated the presence of different natural compounds. The rhizomes of E. laciniata were an important source of iridoid glycosides, flavonoids, and phytosterols (2, 5, 6). Ferulic acid derivatives, furanolabdane diterpene glycoside, iridoid glycosides, and phenylethanoid glycosides have been identified from the rhizomes of E. glabra (7-9). Loasin A and B and Loasifolin with flavonoid structure and Eremoside A to C with iridoids skeleton have also been isolated from E. loasifolia (10-12). Other studies showed the presence of iridoid glycosides from E. moluccelloides and an isoflavone structure from E. vicaryi (13, 14). Phytochemical studies on the essential oil composition of species of this genus have illuminated the presence of terpenoid structures, linear hydrocarbons, and their derivatives (15-21).
E. azerbaijanica Rech. f. is one of the indigenous plants of the East Azerbaijan province of Iran. Phytochemical investigations demonstrated the presence of phenylethanoids and iridoid glycosides from the root and a phenylethanoid as well as a flavonoid from aeria parts of E. azerbaijanica (22-24).
2. Objectives
The objectives of this study are to evaluate general toxicity, cytotoxicity, and anti-bacterial effects of the aerial parts of E. azerbaijanica extracts. Additionally, all the extracts were tested for the presence of various phytoconstituents by different reagents.
3. Methods
3.1. Plant Material
The aerial parts of E. azerbaijanica Rech.f. were gathered during the flowering stage from Bostan Abad, Eastern Azerbaijan (37° 51’ N, 46° 51’ E), Iran, in July 2012. A voucher specimen (TBZ-fph-738) of the plant has been placed in the Herbarium of the Pharmacognosy Department, Faculty of Pharmacy, University of Medical Sciences, Tabriz.
3.2. Extraction
Air-dried and ground E. azerbaijanica aerial parts (50 g) were Soxhlet extracted continually with n-Hexane, DCM and MeOH (500 mL each, all from Caledon, Canada). All these 3 extracts were discretely dried using a rotary evaporator (Heidolph, Germany) at a maximum temperature of 45°C.
3.3. Brine Shrimp Lethality Test (BSLT)
The general toxicity of different extracts from aerial parts of E. azerbaijanica was monitored by the BSLT method (5). The Artemia salina eggs (Sera brand, Turkey) were placed and hatched in flask with 300 mL of artificial seawater (Aqua Marine brand, Thailand). The flask was well ventilated with an air pump and preserved in a water bath at 29 - 30°C. A light source was left on top of the flask. The nauplius appeared after 48 hours. Three extracts were dissolved in dimethyl sulfoxide (DMSO, Merck, Germany) to get a 1 mg/mL concentration and then the stock solutions were diluted with artificial sea water. Different concentrations of extracts were prepared by serial dilution. Almost 10 nauplius were counted and transferred into each tube. Surviving nauplius were counted 24 hours later and the mortality ratio was calculated at each extract doses via the best-fit line plotted concentration versus percentage lethality. The controls were DMSO, normal saline and podophyllotoxin (Sigma-Aldrich, Germany). The LC50 value was estimated using linear regression analysis by Excel software.
3.4. MTT Assay
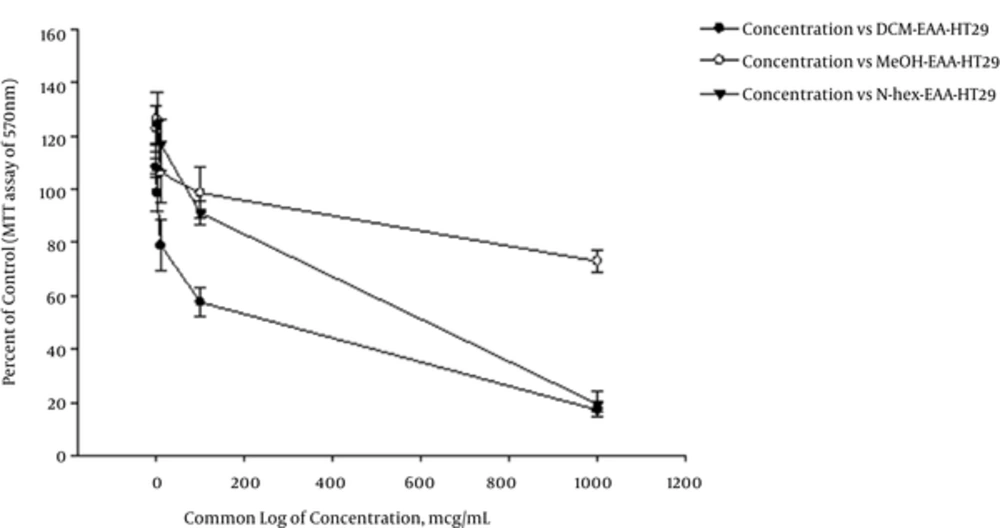
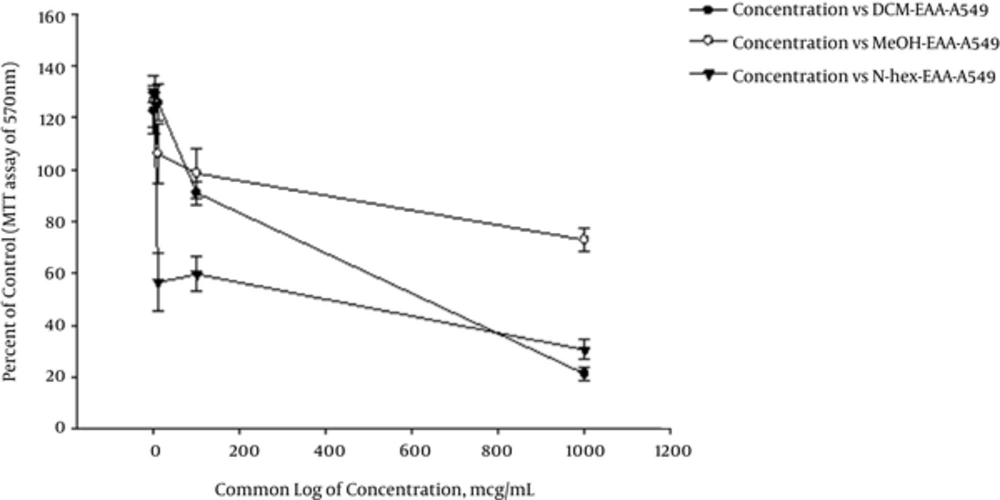
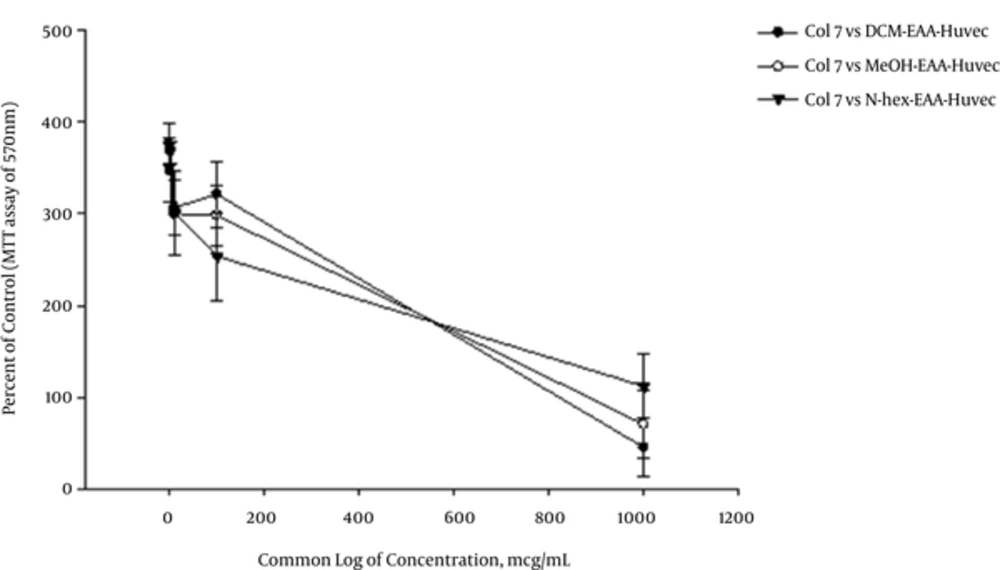
A549 (human lung carcinoma), HT29 (human colorectal adenocarcinoma), and HUVEC (human umbilical vein endothelial) cell lines were cultured in RPMI 1640 (Roswell Park Memorial Institute) medium with essential additives including 100 µg/mL streptomycin and 100 IU/mL penicillin augmented with 10% fetal bovine serum (FBS). The cells were kept in a moistened atmosphere of a 5% CO2 (37°C). (3-(4, 5-dimethylthiazol- 2-yl)-2, 5-diphenyltetrazolium bromide (MTT, Sigma-Aldrich, USA) colorimetric assay was employed to determine the anti-proliferative activity of medicinal plants (25). MTT was dissolved in phosphate buffered serum (5 mg/mL PBS). In MTT assay, 1 × 104 cells/well were seeded into 96-well plates and hatched in 24 hours. Then, the cells were treated with various concentrations of extracts and incubated for 3 days in a moistened atmosphere at 37°C in the presence of 5% CO2. Different dilutions of n-Hexane, DCM, and MeOH extracts (including: 1, 10, 100, 1000 µg/mL), which were dissolved in dimethyl sulfoxide and diluted with cell culture medium, were added to cells and transferred to incubator. After 72 hours of incubation 20 µL of MTT reagent was added to each well. The plates were kept at 37°C for 4 hours. After that, the medium was removed and pure DMSO (100 µL) was added to each well. Finally, the metabolized MTT product was measured by reading the absorbance at 570 nm on a microplate reader (ELISA plate reader, Bio teck, Bad Friedrichshall, Germany). For comparing the anti-proliferative activity of plants, Paclitaxol and DMSO were considered as positive and negative controls. The cell survival was calculated by the following formula: Relative viability (%) = (A test/A control) × 100
Where A control is the absorbance of control reaction (all reagents excluding the plant extracts) and A test is the sample absorbance. The results obtained from 3 independent experiments. The IC50 (the concentration that 50% cell growth is inhibited) was calculated from a dose response curve plotted in the Sigma Plot 10 software (26-28).
3.5. Antimicrobial Assay
3.5.1. Microbial Strains
Examined organisms included 2 species of gram negative bacteria, Pseudomonas aeroghinosa (ATCC 9027), and Escherichia coli (ATCC 8739), 2 strains of gram positive species, Staphylococcus epidermidis (ATCC 12228) and Staphylococcus aureus (ATCC 6538) and a fungus, Candida albicans (ATCC 10231), which were purchased in lyophilized culture from Persian type culture collection (Iran).
3.5.2. Disc Diffusion Test
Activated microorganisms were transferred to Muller Hinton Broth medium (Merck, Germany) and incubated overnight at 37°C. Saline solution was twice applied to provide the turbidity for the centrifuged pallets at 3000 rpm for 15 minutes (equal to 0.5 Mc Farland, 108 CFU/mL as a standard optical density). The final concentration of inoculums was adjusted to about 106 CFU/mL with sterile saline solution. To get a uniform microbial growth, 10 mL of prepared inoculums suspensions were spread over the autoclaved Muller Hinton Agar Medium and then the sterile discs of Whatman paper with 6 millimeters diameter that were impregnated with 50 µL of different concentrations of extracts in 50% aqueous DMSO (1:1, 1:5, 1:10), located on the surface of media. The plates were incubated for 30 minutes in a refrigerator to let the diffusion of extract, and then, they were incubated at 37°C for 24 hours. Lastly, the inhibition zones obtained nearby sterile discs were measured.
In order to compare the potency of the antimicrobial activity of the extracts, 2 control groups were considered including aqueous DMSO as a negative control and a standard disc of Amikacin as the positive control. All tests were performed 3 times and the mean value was calculated (5, 29).
3.6. Phytochemical Screening
3.6.1. Test for Alkaloids
3.6.1.1. Dragendorff Test
The precipitate with reddish brown color by Dragendorff’s reagent (Potassium bismuth iodide solution) indicates presence of alkaloids (30).
3.6.1.2. Hager Test
Alkaloids with Hager’s reagent (saturated solution of Picric acid, Sigma-Aldrich, Germany) give yellow color precipitate (30).
3.6.2. Test for Reducing Sugars
Appearance of reddish orange color precipitate indicates the presence of reducing sugar of extract with Benedicts reagent (alkaline solution containing cupric citrate complex, Sigma-Aldrich, Germany) (30).
3.6.3. Test for Triterpenoids and Sterols (Libermann- Buchard Test)
At first, the samples are treated with a few amount of acetic anhydride (Merck, Germany) and then boiled and cooled. Color change of mixture is started after the addition of concentrated sulfuric acid (Merck, Germany) from the side of the test tube. A ring with a brown color at the connection of 2 layers and the green color upper the layer shows the existence of steroids. Moreover, the creation of deep red color point to the existence of triterpenoids (30, 31).
<b>3.6.4. Test for Amino Acids and Proteins (Ninhydrin Test</b>)
The reaction between amino acids or proteins, with 0.2% solution of Ninhydrin (Indane 1, 2, 3 trione hydrate, Merck, Germany) produces a violet color (30, 31).
3.6.5. Test for Cardiac Glycosides
3.6.5.1. Kedde Test
A purple color is produced with the addition of 1 drop of 90% alcohol and 2 drops of 2% 3, 5-dinitro benzoic acid (Merck, Germany) in 90% alcohol with extract. The medium is made alkaline with 20% NaOH solution. The color reaction with 3, 5-dinitro benzoic acids be influenced by the existence of a beta- unsaturated-o lactones in the aglycone (30).
3.6.5.2. Keller Killiani Test (Test for Deoxy Sugars)
5 mL of extract solution is mixed to 2 mL glacial acetic acid (Merck, Germany) in a test tube and a drop of ferric chloride (Merck, Germany) solution is added. Then 1 mL concentrated H2SO4 is added carefully by the side of the sample tube. A brown ring at the border indicated the existence of deoxysugar characteristic of cardenolides (30, 32).
3.6.6. Test for Tannins and Phenolic Compounds (Ferric Chloride Test)
The sample gives a blue green color with a few drops of ferric chloride (30).
3.6.7. Test for Iridoids
1 mL of Trim-Hill reagent was added to the concentrated extract and then heated for a few minutes. A blue-green or red color indicated the presence of iridoids (33).
4. Results
In the present study, general toxicity, anti-proliferative, and antimicrobial activities of 3 extracts with different polarity from aerial parts of E. azerbaijanica were determined and the results are shown in Table 1. Moreover, 3 extracts were tested for the presence of various structural groups of natural compounds by different reagents and results are indicated in Table 2.
| Extracts | General Toxicityb | Antiprolifrative Activity, µg/mL | ||
|---|---|---|---|---|
| LC50, µg/mL | HT29 | A549 | HUVEC | |
| n-Hexane | 30 ± 2 | 427 ± 107 | 161 ± 95 | > 1000 |
| DCM | 73 ± 4 | 124 ± 37 | 451 ± 73 | > 1000 |
| MeOH | > 1000 | > 1000 | > 1000 | > 1000 |
BSLT and Cytotoxicity of n-Hexane, Dichloromethan and Methanol Extracts of E. Azerbaijanica Aerial Partsa
| Phytochemicals | n-Hexane Extract | DCM Extract | Methanol Extract |
|---|---|---|---|
| Alkaloids | |||
| Dragendroff’s test | - | - | - |
| Hager’s test | - | - | - |
| Reducing sugars | |||
| Benedict’s test | - | - | - |
| Sterol and triterpenoid | |||
| Libermann- Buchard test | +++ | +++ | - |
| Proteins and amino acids | |||
| Ninhydrrin test | |||
| Cardiac glycosides | |||
| Kedd test | +++ | +++ | - |
| Keller- Killiani test | - | - | - |
| Tannins and phenolic compounds | |||
| Ferric Chloride test | - | - | - |
| Flavonoids | |||
| Shinoda test | - | - | + |
| Iridoids | |||
| Trim-Hill test | - | - | +++ |
Phytochemical Tests for Various Extracts of E. Azerbaijanica Aerial Parta
Antimicrobial effect of the extracts was subjected to screen by agar disc diffusion technique and no antimicrobial effect was observed against examined microorganisms.
5. Discussion
Brine shrimp lethality test (BSLT) is known as a low-priced test revealing of anti-bacterial, cytotoxic, pesticidal, and insecticidal activities and could be used as a simple technique with small amounts of test materials (34). The BSLT of the extracts obtained from E. azerbaijanica aerial parts were evaluated at different polarities. Table 1 shows that both n-Hexane and DCM extracts were efficient in BSLT as impure fractions and MeOH extract showed no significant level of toxicity (LC50 > 1.0 mg/mL) in comparing with podophyllotoxin (a cytotoxic lignan) as a well-known standard. According to our previous studies regarding BSLT of pure iridoid glycosides of E. laciniata and ferulic acid derivatives of E. glabra roots, these compounds had no significant level of toxicity at LC50 > 1.0 mg/mL (4, 5).
The cytotoxicity (IC50) of the extracts of E. azerbaijanica aerial parts were evaluated for 2 cancer cell lines and 1 normal cell line and the results were shown in Table 1. The DCM and n-Hexane extracts showed potent cytotoxic effects for the HT29 and A549 cell lines, whereas MeOH extract didn’t show any significant cytotoxicity for these cell lines. Furthermore, the 3 extracts of E. azerbaijanica didn’t demonstrate any substantial activity against HUVEC as a normal cell line. Therefore, based on the remarkable effects of DCM extract on HT29 cell line and n-Hexane extract on A549 cell line, this plant can be considered as a potential natural resource of antitumor agents for future studies.
As shown in Table 2, preliminary phytochemical screening indicated that the DCM and n-Hexane extracts contained sterols, triterpenoids, and cardiac glycosides. These findings are consistent with data obtained in previous research for the cytotoxic effects of steroids, triterpenoides (35, 36), and cardiac glycosides (37, 38) on different cell lines. Additionally, our currently published paper showed the presence of hexa hydrofarnesyl acetone (27.1%), 2- methyl- 6-propyl- dodecane (16.4%), and tricosane (9.3%) as the major components of volatile oil of this plant (24), which might cause the observed anti-proliferative activities (39).
Pursuant to some previous reports, there is a direct relationship between the toxic activity in the BSLT and anti-proliferative effects; hence, it might be suggested that the BSLT is an inexpensive, easily mastered, and suitable preliminary assay for predicting cytotoxic activity (40). Moreover, these findings will guide us to purification and identification of responsible compounds and to find the synergistic or antagonist effects of them.
5.1. Conclusion
Our studies demonstrated for the first time the anti-proliferative activity of n-Hexane, DCM, and MeOH extracts of E. azerbaijanica aerial parts on 3 cell lines. Both n-Hexane and DCM extracts possessed potent general and cytotoxic effects on against A. salina, HT29 and A549 cell lines, respectively. Therefore, in the future, more studies should be focused on isolation of active and pure ingredients and clarification of anti-neoplastic mechanism of them.