1. Introduction
Extrapulmonary tuberculosis (TB) constitutes 15 - 20% of the total TB load in immunocompetent patients (1). Cutaneous involvement represents 1 - 2% of these cases (2, 3). The prevalence of cutaneous TB in India is 0.1 - 0.9%, according to various sources (3-5). Scrofuloderma is a type of secondary cutaneous TB arising from an endogenous source that spreads by contiguity from underlying lymph nodes, bones, or joints to the skin. It usually occurs on the neck in children, with cervical lymph nodes being the most common focus (6). The involvement of the skeletal system is unusual, which is observed in 6 - 10% of extrapulmonary TB cases (7). Approximately 60 - 80% of skeletal TB cases show the involvement of spine or weight-bearing joints, with sternal osteomyelitis being extremely rare in 1% of cases, even in endemic countries (7). We hereby report an immunocompetent adolescent female presenting with chronic non-healing sinus-like lesions and bridging scars mimicking infected presternal keloids. She was diagnosed with scrofuloderma with multifocal TB on a thorough evaluation.
2. Case Presentation
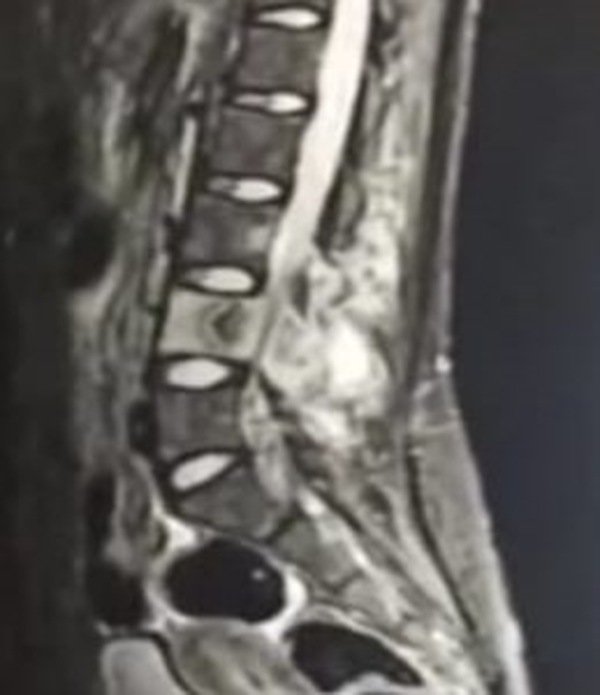
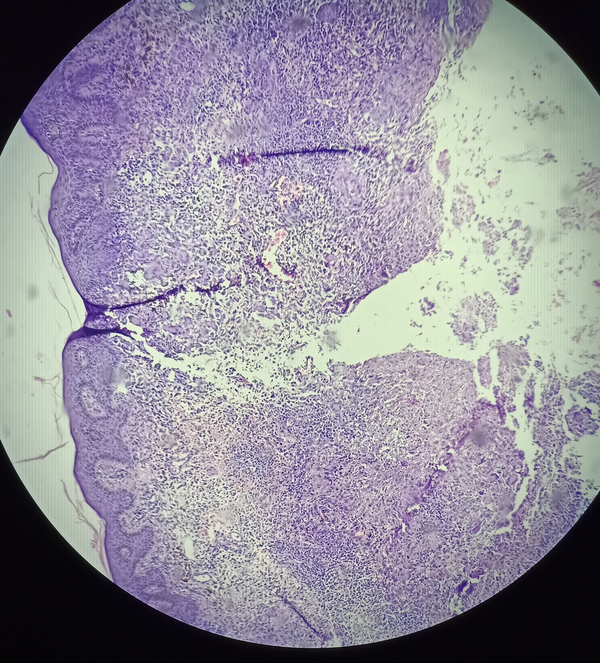
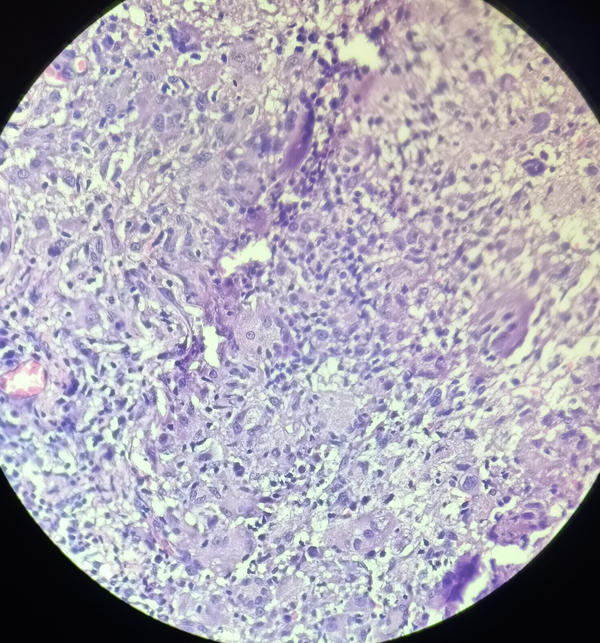
A 16-year-old unmarried female, hailing from an urban shantytown, came to our hospital with complaints of a chronic, non-healing, gradually progressive lesion on the upper part of the chest since one year ago. It had started as a pea-sized reddish swelling on the upper chest, which later increased in size and ruptured, forming a pus discharging tract. Before presenting to us, the lesion had been diagnosed and treated as keloid with secondary infection with no improvement. On inquiry, she had a history of significant weight loss, evening rise of fever, and chronic low backache. She denied a history of cough, neck or axillary swellings, antecedent trauma at the site of lesion, abdominal pain, or diarrhea. There was no past or family history of TB. On examination, the patient was cachexic (weight: 35 kg) with pallor, non-tender discrete axillary lymphadenopathy, and spinal tenderness in the lumbar area. Dermatological examination revealed dusky reddish to hyperpigmented, firm, rubbery discrete plaques (keloid-like) on manubrium sterni with bridging scars and an intervening sinus discharging sero-purulent fluid on manipulation (Figure 1). The lesions were tender and adherent to the underlying bone. Based on these findings, clinical differentials of scrofuloderma, atypical mycobacterial infection, actinomycetoma, chronic osteomyelitis, and lobomycosis were considered. The suspicion of tubercular etiology prompted us to explore other foci of tuberculosis. Hematological investigations revealed anemia and an elevated erythrocyte sedimentation rate (ESR) (40 mm at the end of 1 hour). Human immunodeficiency virus (HIV) - enzyme-linked immunosorbent assay (ELISA) was non- reactive. Hepatitis B and C serostatus was negative. Gram stain, Ziehl Neelsen (ZN) stain, and fungal stains were negative. Tuberculin skin test result was positive with induration of > 10 mm. Sputum ZN stain and nucleic acid amplification tests failed to demonstrate acid-fast bacilli. Chest X-ray (anteroposterior and lateral views) showed manubrial erosive lesion (Figure 2), confirmed on computed tomography (CT) scan of thorax with additional findings of mediastinal lymphadenopathy. Ultrasound of abdomen and pelvis revealed hypoechoic psoas collections. Magnetic resonance imaging (MRI) of the lumbar spine revealed prevertebral and paravertebral necrotic collections in the third to the fifth lumbar region with right psoas peri-muscular collection suggestive of psoas abscess (coronal section) and fourth lumbar vertebral sclerosis in sagittal section (Figure 3). These changes were reported as Pott’s spine. Acid-fast bacilli culture of seropurulent sinus discharge on Lowenstein-Jensen (LJ) medium was positive. Skin biopsy depicted the presence of epithelioid cell granulomas with Langhan’s giant cells and foci of caseous necrosis, suggestive of tuberculosis (Figures 4 and 5). Clinicopathological and radiological correlation led to the final diagnosis of scrofuloderma with multifocal TB. The patient received antitubercular treatment (ATT) with fixed-dose combination (FDC) of isoniazid (75 mg), rifampicin (150 mg), pyrazinamide (400 mg), and ethambutol (275 mg) given as two tablets daily, with topical antibiotics over the oozing sinuses. An orthopedics consultation was done, wherein she was advised conservative management. Dietary advice and haematinics with pyridoxine were also offered to improve her nutritional status. Currently, she is under regular follow-up.
3. Discussion
Tuberculosis is a chronic granulomatous infectious disease caused by Mycobacterium tuberculosis. Extrapulmonary forms significantly contribute to the morbidity and mortality of TB because of delayed or missed diagnosis, variable presentations, and multifocal involvement, especially in co-infection with HIV as a “cursed duet” (8). It can involve lymphoreticular, gastrointestinal, musculoskeletal, cutaneous, and nervous systems, as well. Cutaneous tuberculosis can be categorized on the basis of route of infection as exogenous and endogenous, which is further classified as hematogenous, lymphatic, and contiguous and also on the basis of bacillary load as multibacillary and paucibacillary (6). Scrofuloderma is the most common form of cutaneous TB among children, whereas lupus vulgaris is the most frequent variant in adults (6). The proportion of scrofuloderma was found to be 53.3% by Kumar et al. and 36.9% by Vashisht et al. [cited in Kumar and Kumar (6)]. It is a multibacillary form of secondary skin tuberculosis that spreads via a contiguous route. It more commonly arises in the neck from underlying cervical TB lymphadenitis, also known as scrofula (Latin word: scrofa - a brood sow). Nasopharyngeal TB or the practice of consuming unpasteurized milk in rural areas can be causative factors for the involvement of cervical nodes (6). Other lymph node groups affected include inguinal, axillary, submandibular, epitrochlear, and supratrochlear. Around 66% of cutaneous TB cases show systemic foci (6). Other than lymph nodes, the bones, joints, testes, breast, and lacrimal glands are the other underlying foci of scrofuloderma (6). Rarely, hepatic and intestinal TB can also be a focus of skin infection (6). Clinical presentation in childhood is characterised by the presence of multiple, chronic asymptomatic, subcutaneous cervical swellings, which later undergo softening, and ulceration forming discharging sinuses. These ulcers have bluish, undermined edges. Healing occurs with bridging, cribriform, or puckered scars. Adult scrofuloderma is a more localized entity. Skeletal TB accounts for 6 - 10% of extrapulmonary TB cases (7). It most frequently involves spine or weight-bearing joints. Sternal affliction is seldom seen, representing only 1% of skeletal TB cases (1, 7), while sternal osteomyelitis constitutes 0.3% of osteomyelitis cases (1, 7). It may be primary or usually found as an extension from hilar lymph nodes or hematogenous or lymphatic dissemination from other sites. Sternal TB has also been reported in the pediatric age group after Bacille Calmette Guerin (BCG) vaccination (9). Gallouj et al. have reported a similar case of scrofuloderma leading to the discovery of sternal TB (10). However, the finding of multifocal systemic TB (defined as the presence of two or more lesions in extrapulmonary sites with or without pulmonary involvement) (8) renders our case unique. Multifocal TB accounts for less than 10% of TB cases, and its association with skin involvement is rare, with only a few reported cases (8). Risk factors for extrapulmonary dissemination are female gender, malnutrition, low socio-economic status (all present in our case), HIV infection, and other immunocompromised states (11).
Diagnosis of multifocal TB is challenging, owing to delayed presentation, clinical polymorphism, and the diversity of organs affected. Skin involvement is dominated by scrofuloderma and gummas (8). Skin is also a site easily accessible for clinicopathological examination. Two pathomechanisms can give rise to multifocal TB: (1) hematogenous dissemination, and (2) initial hemolymphatic seeding of multiple organs with subsequent reactivation (8). Numerous investigations, including screening (Mantoux test induration > 10 mm), imaging studies (X-ray, computed axial tomography, MRI, ultrasonography), cytopathological studies (fine needle aspiration cytology and histopathology), IS-6110 polymerase chain reaction (high sensitivity), and culture (gold standard) are necessary for the establishment of the diagnosis of multifocal TB. Our case had the clinical presentation of bridging scars with sinuses over the upper chest (manubrium sterni), which is an extremely unusual site for scrofuloderma (7). Lesional morphology resembled an infected keloid (for which the patient had been earlier unsuccessfully treated) further compounding the diagnostic conundrum and suggesting multiple differentials like deep fungal (lobomycosis) or atypical mycobacterial infection, actinomycetoma, and nocardiosis. Furthermore, such lesions occurring over intertriginous regions may simulate hidradenitis suppurativa. It was only on the basis of strong clinical suspicion and thorough radiological and histopathological investigations that a final diagnosis of multifocal TB (sternal, mediastinal, cutaneous, and lumbar vertebral) was reached. A multidisciplinary consultation was sought wherein conservative management was recommended for skeletal TB in addition to the antitubercular treatment (ATT). Indian’s new revised national tuberculosis control program (RNTCP) guidelines for extrapulmonary TB, recommend the use of FDC of ATT (Table 1) (12). Multifocal TB should always raise the suspicion of underlying HIV infection and immunosuppression (8). The presence of multidrug-resistant (MDR) or extensively drug-resistant (XDR) TB poses great therapeutic difficulty with prolonged treatment courses and poorer prognosis. Although our patient was immunocompetent, the diagnosis was delayed due to atypical site of cutaneous presentation (upper chest instead of neck or axilla), rare focus (sternal TB), and more importantly, morphological resemblance to keloid with the presence of non-specific subtle symptoms and signs.
| Weight Category (kg) | Number of Combination Combination (FDC) | |
|---|---|---|
| Intensive Phase (2 months); HRZE (75, 150, 400, and 275 mg) | Continuation Phase (4 months); HRE (75, 150, and 275 mg) | |
| 25 - 39 | 2 | 2 |
| 40 - 54 | 3 | 3 |
| 55 - 69 | 4 | 4 |
| ≥ 70 | 5 | 5 |
The Doses of the Fixed-Dose Combination of Antitubercular Treatment According to the Weight Bands (New Revised RNTCP Guidelines for Pulmonary and Extrapulmonary New/Untreated Cases) (12)
3.1. Conclusion
Involvement of skin and sternum in multifocal TB is rare. Accurate recognition of the myriad faces of cutaneous TB is essential, particularly in high burden countries, as skin provides a window of opportunity for diagnostic interventions. Scrofuloderma might just be the tip of the iceberg, warranting a meticulous evaluation to unveil hitherto undetected multifocal systemic tuberculosis.