1. Background
Melasma is a common disease amongst skin pigmentation system disorders. It is most prevalent in people aged 30 to 55 and generally occurs in regions where the skin is exposed to the sun, such as malars, temple, upper lip and chin (1, 2). Pregnancy, contraceptives, and UV exposure account for this disorder. It is a common cause of women referral to dermatologists. Typical long-term treatments of this disorder, such as the use of the Kligman’s formula, have failed (3, 4). Therefore, new therapies have been suggested in a number of studies. The use of different lasers in the treatment of dermal melasma is still under discussion.
2. Objectives
This study was designed based on previous studies and adopted combined therapies. It aimed to assess and compare the remedial effect of hydroquinone plus neodymium-doped yttrium aluminium garnet (Nd: YAG) laser with and without CO2 fractional laser.
3. Patients and Methods
This study was a split-face randomized clinical trial done at Rasoul Akram hospital during years 2013 and 2014. All patients who were diagnosed with melisma and resistance to other treatments were included and those that had post-inflammatory hyperpigmentation due to laser or sensitivity to hydroquinone were excluded.
Patients with dermatologist-diagnosed melasma were checked by the research physician. After explaining the purpose and method of the study, the subjects signed an informed consent and received the initial explanations. The melasma lesions were divided to two zones with respect to the face symmetry line. Hydroquinone cream was locally applied on both zones, and one zone was treated by Q-switched (QS)-Nd: YAG laser + CO2 fractional laser, while the other only recieved QS-Nd: YAG laser. Next, Melasma area and severity index (MASI) checklist was filled by the researchers with respect to the cases’ status. This questionnaire divides the human face to four zones in order to score every zone; the four zones include forehead, right malar, left malar and chin. The first three zones occupy 30% of the total area of the face, while the latter one (chin) occupies only 10% of the face area. Melasma area and severity index measures the degree of melasma and scores its severity. The area of melasma lesion was scored from zero to six depending on the stricken area, where zero was allocated to non-stricken zones and six was allocated to zones occupying 90% - 100% of the face area. The darkness of melasma was scored from zero to four. Total score of MASI was obtained from the equation 1:

To avoid allergies, the cases were asked to rub the cream on the inner side of their forearm skin and let it remain for 48 hours without washing or cleaning. In the event of no allergy, the cases were asked to use the cream for 10 days before laser treatment and continue using for 12 weeks after treatment on butterfly-shaped melasma lesions of their face once a day at nights.
The cases were advised to apply a sunscreen to their face with minimum SPF of 25, every three hours. They were instructed to use the cream both outdoors and indoors. The second visit was two weeks after the first use of hydroquinone on melasma lesions. This was a split-face study in nature, which compared the effects of two treatment methods in any given case with different backgrounds.
At the beginning of the study, hidden codes were allocated to the cases inside closed envelopes. After determining the MASI scores, the envelopes were opened and they included detailed data about the treatment methods to be applied on the left and right side of the face.
The AMANA device (Unixel, USA) was used in this study to produce QS-Nd: YAG laser with a wave length of 1064 nm, probe size of 12 mm, one pass, and power of 700 J/cm2, as well as CO2 fractional laser with level of 12, power of 400, spot size of 0.8 and one pass; laser therapy sessions were held once every six weeks at the same time. Prior to every session, the under-treatment regions of the skin were checked by a dermatologist in order to assess probable color change suspected to be induced by side effects of laser therapy. Energy power of all sessions was the same. After laser treatment, patients were asked to use anti-solar, zinc oxide ointment and hydroquinone for 14 weeks. The cases were rechecked once every six weeks and received the next laser-therapy. Generally, this treatment was completed within 12 weeks. During this period, hydroquinone cream was applied once a day and laser-therapy sessions were held once every six weeks. The MASI questionnaire was filled after every laser-therapy session and the trend of treatment was evaluated; i.e. a dermatologist diagnosed the melasma cases and assessed the trend of treatment from the beginning to the end of the study. The cooperating physician received no information about the therapy method and recorded the probable side effects and their severities only by observing and checking melasma lesions on the face and comparing before, during and after treatment pictures.
Neither the cases nor the physician who recorded the MASI scores were informed of the therapy method on both sides of the face. Before every session, the cases status in terms of responding to therapy and probable side effects was recorded. Side effects included any sign of itching, erythema or skin rashes, hypopigmentation, depigmentation or lightening of the hairs of the therapy zone, and fainting or having such problems at home, suspected to be induced by laser therapy.
The SPSS statistical software 16.0.0 (SPSS Inc. Chicago, IL, USA) was used for all data analyses. P-values of less than 0.05 were considered statistically significant. All tests were two-sided. Categorical data were expressed as numbers (percentages). Continuous variables were reported as means (SD) or medians (range). The normality assumption of the continuous variables was examined using the Shapiro-Wilk’s W-test. Matched statistical analysis of data was made using the paired t-test. The generalized estimating equation method was applied to the data. To control the effect of the MASI score at baseline, this variable was considered as a covariate in the model. All tests were two sided and a significance level of 0.05 was considered significant. All statistical analysis was performed with the SPSS 16.0.0 software (SPSS Inc. Chicago, IL, USA).
In this study, the researcher was obliged to observe the ethics statement measures. However, the cases entered this study after signing an informed consent.
4. Results
Seventeen patients with resistant dermal melasma (14 females and three males) with mean (± SD) age of 38.47 (± 6.29) years (range 29 - 53) were recruited in this study. The median duration of melasma was three years (range between one and ten years). The only side effect was erythema observed only in two cases (11.8%). The mean MASI scores for the sides treated with Nd: YAG laser and Nd: YAG + CO2 fractional lasers are presented in Table 1.
a The values are expressed as mean ± standard deviation (SD).
b Abbreviation: Nd: YAG; neodymium-doped yttrium asluminium garnet.
c P < 0.05 for statistical difference from baseline to week six within the group.
d P < 0.05 for statistical difference from week six to week 12 within the group.
e P < 0.05 for statistical difference from baseline to week 12 within the group.
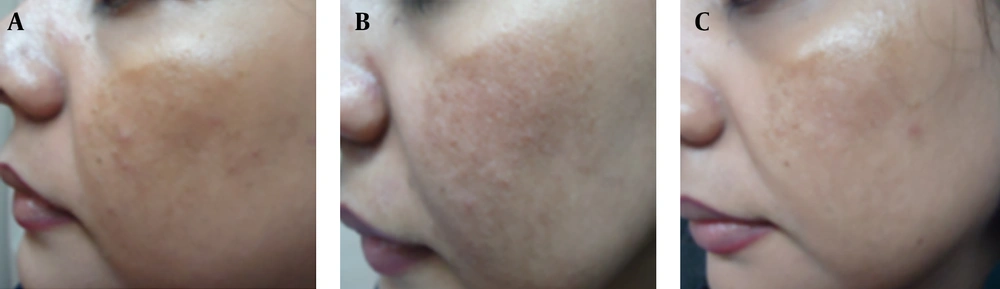
The mean MASI scores reduced significantly after six weeks for both therapies (Table 1) (Figure 1 A, B and C). Also, the mean MASI scores decreased significantly from week six till the end of the study (Table 1). After six weeks of therapy, the mean percentage reduction of MASI scores from baseline was 39.4% for Nd: YAG laser therapy and 58.45% for Nd: YAG + CO2 fractional laser (Figure 2 A, B and C).
On the side treated with Nd:YAG laser, the mean percentage reduction of MASI score from baseline at the end of the study was 67.51% and on the side treated with Nd:YAG + CO2 fractional laser this was 80.78%. Using the generalized estimating equations (GEE) method for testing the effect of the therapies, after controlling for MASI score at baseline, a difference was observed between mean MASI scores of the two therapies (P = 0.001). Controlling for the effect of “MASI score at baseline”, a significant reduction was observed in the MASI score of the side treated with Nd:YAG + CO2 fractional lasers in comparison with the side treated with Nd:YAG laser.
5. Discussion
This study compared the effects of topical hydroquinone cream plus Nd:YAG laser with and without CO2 fractional laser in the treatment of dermal melasma. According to the results, treatment of this disorder with Nd:YAG laser + CO2 fractional laser was more effective than the use of Nd:YAG laser alone (a reduction of 80.78% versus 67.51%). Previous studies have assessed the long-pulse effect of Nd:YAG laser in melisma (5-7). Our study agrees with the study of Wattanakrai et al. (6) and Jalaly et al. (7). Although the methodology of these studies was not similar to that of the present study, they confirmed that the inclusion of CO2 fractional laser in the treatment plan could improve the outcomes (8-10).
This study showed that a triple component treatment, i.e. hydroquinone cream plus Nd:YAG and CO2 fractional laser was more effective than a dual component treatment, i.e. hydroquinone cream plus Nd:YAG laser. In this study, only two cases (11.8%) showed side effects.
To investigate the mechanisms behind our observations, previous studies and articles were reviewed (11-17). Treatment of melasma by laser is based on the theory that laser spectrum is absorbable in specific tissues of the body (18-21). Certain wave-lengths are absorbed by pigments present in tissues (22-26). At wavelengths of 400 nm to 600 nm, pigments compete with oxyhemoglobin on absorbing photons, which increase vascular damage (1, 15, 18, 27-29). Among Q-switched lasers, post-treatment recurrence is prevalent in ruby laser. It is important to consider that all cases of this study were therapy-resistant with median duration of three years ranging from one to ten years. Manaloto et al. (27) advise laser for the treatment of severe or dermal melasma. In line with this report, our study confirmed the effectiveness of laser therapy for the treatment of melasma. This study, however, showed that during the three weeks of therapy with an interval period of four weeks (total = 12 weeks), the mean percentage reduction of MASI score from baseline was 80.78% in the Nd:YAG plus CO2 fractional group.
The study of Jalaly et al. (7) agrees with this study and shows the effects of CO2 fractional laser on decreased MASI score compared with Nd:YAG laser alone. Regarding the research methodology, hydroquinone therapy was started two weeks before the laser therapy in this study.
As a hydroxyphenol, hydroquinone competes with tyrosine for tyrosinase enzyme, which plays a role in melanin synthesis, resulting in reduced tyrosinase activity and melanin synthesis (1, 25, 26). Different studies have reported on the improved status of melasma at different degrees after treatment with hydroquinone (22-24, 30). Based on our observations, it seems that a combination of hydroquinone, Nd:YAG laser and CO2 fractional laser reduces melanin synthesis and increases melanocytes destruction.
A significant decrease in MASI was achieved by destructing pigments through laser on the one hand and reducing the formation of melanosome in keratinocytes and inhibiting its re-synthesis by hydroquinone, on the other hand. The addition of CO2 fractional laser to Nd:YAG laser and hydroquinone can create a different condition for destructing melanosomes. According to our observations, this combination has more effective results for the treatment of melasma. The 1064 nm QS-Nd:YAG is well absorbed by melanin and causes minimal damage to the epidermis and is not absorbed by hemoglobin. The deeper skin penetration is also helpful to target dermal melanin. Low-dose QS Nd:YAG laser induces sublethal injury to melanosomes causing fragmentation and rupture of melanin granules into the cytoplasm (31). There is also subcellular damage to the upper dermal vascular plexus, which is one of the pathogenetic factors in melisma. QS-Nd:YAG is the most widely used laser for the treatment of melasma (11, 32-34). Fractional lasers are a new method for melisma treatment, by which multiple microscopic zones of thermal damage are created leaving the majority of the skin intact. These multiple columns of thermal damage are called microthermal treatment zones (MTZ) and lead to extrusion of epidermal necrotic debris that includes pigment in the basal layer. The depth and diameter of MTZ are determined by the used energy levels. The density used and the number of passes determine the proportion of surface area treated. Fractional laser therapy has many advantages. It does not create an open wound, the recovery is faster and complications of open wounds such as hyper or hypopigmentation are avoided.
This study was a split-face randomized trial, which makes the results more reliable. On the other hand, simultaneous use of hydroquinone and laser therapy differentiates this study from others.
Hydroquinone treatment was initiated two weeks before laser therapy. Therefore, our results include the outcomes of the use of hydroquinone for 14 weeks. No study has ever reported on the effects of simultaneous use of hydroquinone and Nd:YAG + CO2 fractional laser. In the treatment of dermal melasma, there was a significant difference between Nd:YAG laser and the combination of Nd:YAG laser and CO2 fractional laser, and thus the latter method is recommended. Conducting more studies and comparing them with other therapies and studies with large population sizes are suggested for future research. Our study’s limitations include small sample size, short time of follow up and poor control of patients compliance in using anti-solar creams, thus further studies with large sample sizes are recommended.