1. Introduction
Epidermolysis bullosa (EB) refers to a group of inherited disorders that involve the formation of blisters following trauma (1). Epidermolysis bullosa pruriginosa is a recently described variant, caused by Type VII collagen gene mutation, with distinctive clinicopathological features (2). Most cases are sporadic (3), however, a few show autosomal dominant or autosomal recessive pattern of inheritance (2). Microscopic studies of EB pruriginosa show typical findings of dystrophic EB (4); in addition, it has been postulated that itching lesions of EB pruriginosa could represent an abnormal dermal response of some subjects to their inherited bullous disorder. The study of the molecular basis of dominant dystrophic EB (classical) and EB pruriginosa shows that both diseases are caused by a missense glycine substitution mutation by different amino acids in the same codon of COL 7A (G2028R and G2028A) (5).
2. Case Presentation
A 19-year-old Iranian girl, presented with blisters since the age of one year, on the distal of both lower extremities as well as on the elbows and knees. With age, nail involvement as nail dystrophy, pruritus, especially in the toenails, were added to her features. From three years ago, pretibial aspects of both legs were predominantly involved. Over time, pruritus gradually worsened with extension of lesions to her neck and lower back. No triggers were reported.
She was born of non-consanguineous marriage and was the first child of her family. There was similar skin involvement in her father and brother. Her fathers’ disease was more severe than hers with more involvement of the skin and absence of all nails from an early adolescent. Her brother also developed pruritic lesions and blister formation from childhood, however, he was much less affected.
On examination, multiple prurigo like papulonodules coalescing into a confluent plaque, milia formation, and excoriation were seen on the shins and dorsal aspect of both feet (Figure 1). Thin erythematous plaques with atrophic scars on the surfaces and milia on the rim, were seen on the knees and elbows. All toenails and some of the finger nails were dystrophic (Figure 2).
Apart from the skin and nail changes, she was in good general condition with no significant problems in swallowing, bowel functions, eyes, or teeth and was otherwise healthy and without a history of atopy.
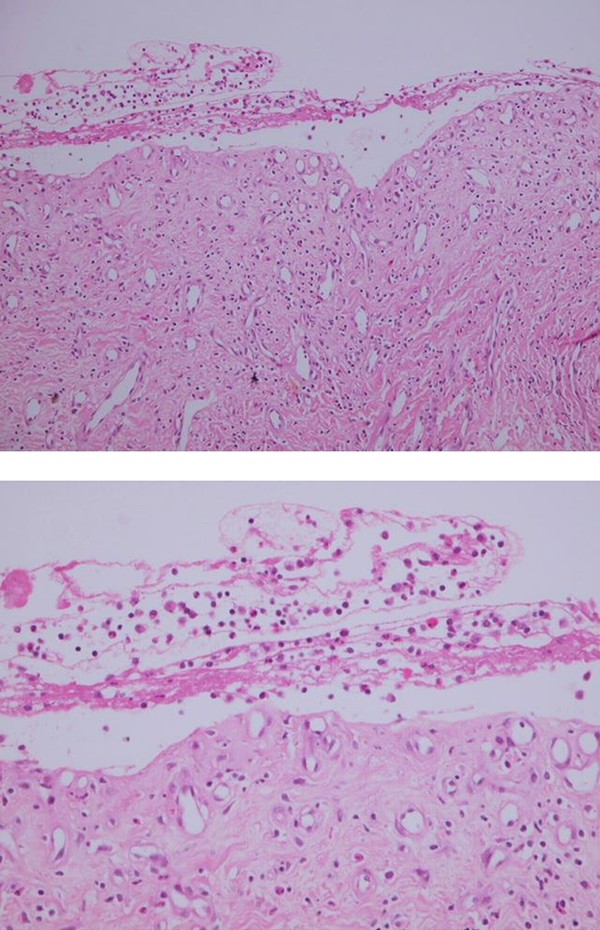
On the histopathology, a subepidermal blister has been showed. Dermis shows fibrosis with vertically oriented capillary sized vessels. There is mild infiltration of lymphocytes, eosinophils, and neutrophils in the upper dermis and in the blister cavity (Figure 3).
She had received a topical steroid and systemic antihistamines with no response after one year. In our center, patient treatment was initiated with systemic cyclosporine (2 - 3 mg/kg) with monitoring of blood pressure and serum biochemistry. After one week, the pruritus of lesions and development of new blisters decreased.
After three months, the patient had virtually complete resolution of pruritus. The papulonodular lesions of the shins were flattened and blister formation was stopped, however, there was no improvement in the nail involvement (Figure 4). After a three-month period, on oral cyclosporine, atrophic scars and post inflammatory hyperpigmentation were predominant features of the lesions.
3. Discussion
EB pruriginosa is a type of dystrophic EB termed by McGrath in 1994 (2). In the one original series of eight cases reported by McGrath, three had family history of similar skin disease, two showing an autosomal dominant, and the other an autosomal recessive pattern of inheritance. The pathogenesis is unknown; therefore, therapeutic agents are not successful. Treatment is necessary to control pruritus and the progression of cutaneous lesions. Potent topical steroids and intralesional triamcinolone were successful in some cases. Systemic therapy, such as antihistamines, corticosteroids, or etidronate, had no good effect (2). Our patient had no response to topical steroids and long-term use had compounded the skin fragility by inducing significant cutaneous atrophy.
Tacrolimus is a macrolide immunosuppressant produced by the soil fungus Streptomyces tsukubaensis that has been used in different dermatologic diseases to reduce pruritus such as atopic dermatitis. In a case report they reported successful treatment with topical tacrolimus (6). Since systemic cyclosporine has been used in EB pruriginosa with some success (4) and other immunosuppress agents such as colchicine and thalidomide has been used in treatment (7-9), there is just a few case reports to treat this disease. Although the pathogenesis of the pruritus in EB is not clear, increased serum levels of IgE can cause pruritus. Cyclosporin can eradicate Pruritus by decreasing serum IGE level. Cyclosporine can be a good choice.