1. Background
Acute coronary syndrome (ACS) includes patients with NSTEMI, STEMI and unstable angina (1). Despite progression in the prevention and treatment of cardiovascular diseases, it still continues to be recognized as the leading cause of death in the world. Finding the risk factors associated with cardiovascular disease (CVD) helps better prevention of the disease. Different risk stratification models have been designed for CVD. CVD associated risk factors are mainly categorized into two large groups; acquired and hereditary. The epidemiological studies suggested inappropriate diet, obesity and weight gain, low physical activity, smoking, hypertension, increased cholesterol and impaired lipid profiles, family history of CVD, age, sex, alcohol consumption, environmental factors, air pollution, and stress as the most important CVD related risk factors (2-4).
The ratio of NSTEMI to STEMI is increasing so that today only less than 30% of myocardial infarctions (MIs) are due to STEMI (5-7). Currently, we can detect even small sized myocardial necrosis with highly sensitive tests. Analyzing serial high-sensitivity cardiac troponin T (hs-cTnT) is the most common tool for myocardial injury screening, resulting in a higher diagnostic rate of NSTEMI patients (7). Previous studies have shown that STEMI patients have more hospital mortality than NSTEMI patients, but long-term outcomes after a percutaneous coronary intervention (PCI) is independent of MI types (8). In STEMI patients, the incidence of cardiac failure and cardiogenic shock in the anterior MI is higher than those with inferior and lateral MI (9). Unlike STEMI patients, the electrocardiogram (ECG) is not a suitable tool to identify the involved vessel in NSTEMI patients. Several studies have used brain natriuretic peptide (BNP) and ECG to identify the culprit vessel responsible for NSTEMI. However, the ECG's ability to locate an occluded vessel and the predictive value of BNP have usually been influenced by left ventricular failure (10).
One of the major mechanisms in NSTEMI is activation of platelets at the site of ruptured plaque. Platelets secrete and express significant amounts of substances, which cause inflammation, thrombosis, and finally atherosclerosis. The high platelet volume is associated with platelet activity and increased platelet adhesion (11). The association of mean platelet volume with thrombosis and inflammation has been studied before. There is a lot of evidence suggesting MPV is associated with the pathophysiology of ACS (12). MPV is available test in emergency room, and therefore, it can be used as an appropriate marker to assess the risk in these patients.
2. Objectives
In this study, we are going to determine whether MPV can help to predict the culprit vessel in NSTEMI patients or not.
3. Methods
3.1. Study Design
In this cross sectional study 349 patients with NSTEMI were evaluated between 2015 and 2017 in a tertiary center. Confirmed diagnosis of NSTEMI was defined according to fourth universal definition of MI (13). Patients with cTnI above the 99th percentile, T inversion > 1 mm, typical chest pain and new Q wave on ECG and also ST segment depression > 1 mm in the absence of ST elevation and new left bundle branch block were included. Patients with previous history of revascularization including percutaneous coronary intervention (PCI) and coronary artery bypass grafting (CABG) were included. On the other hand, patients with a history of receiving blood transfusion in the last three months, history of cancer and chemotherapy, use of drugs that affect hematological factors, history of platelet disease and patients with acute and severe bleeding were excluded. In all patients, 2 mL venous blood sample was taken from median cubital vein collected in tubes with EDTA. The sample was analyzed by an automated blood cell analyzer (ADVIA 2120; Siemens, Forchheim, Germany), estimating MPV during half an hour of sample collection (14).
3.2. Assessments
Major cardiac risk factors (cigarette, diabetes mellitus (DM), hypertension (HTN), hyperlipidemia (HLP)) and angiographic findings and drug history of patients were extracted from patients’ medical files. Then the MPV in complete blood count results and angiography findings were analyzed for any association. According to culprit lesions, patients were divided into LAD and non-LAD groups. Coronary artery disease was defined as any stenosis > 70% relevant to patients symptoms and ECG findings.
3.3. Statistical Analysis
All data were analyzed by descriptive statistics including mean, standard deviation, and frequency. Means were compared by independent t-test. Proportions were compared by chi-square test. Multiple logistic regression analysis was used to compare the variables of patients in the two groups. The P Value less than 0.05 is considered statistically significant.
4. Results
In this study, 349 patients were evaluated. Majority of these patients (79.3%) were male. The mean age of patients was 62.8 ± 10.7 (40 to 89 years old). The most common underlying disease was HTN. About half of the patients were smokers. Angiographic evaluation revealed single vessel disease (SVD) involvement in 44.8% of cases. The most involved culprit vessel was LAD (58.6%), followed by left circumflex (LCX) (24.1%) and right coronary artery (RCA) (17.2%). TIMI flow grade 3 was seen in majority of patients (79.3%) (Table 1).
| Characteristics | Mean (Range) ± SD or Frequency (%) |
|---|---|
| Age | 62.8 ± 10.7 |
| Gender (male) | 79.3% |
| Risk factors | |
| Diabetes mellitus | 24.1% |
| Hypertension | 65.5% |
| Hyperlipidemia | 17.2% |
| Smoking | 48.3% |
| Number of vessels | |
| SVD | 44.8% |
| 2 VD | 34.5% |
| 3 VD | 20.7% |
| Culprit vessel | |
| LAD | 58.6% |
| Lcx | 24.1% |
| RCA | 17.2% |
| Thrombus TIMI | |
| Grade 1 - 4 | 86.2% |
| Grade 5 | 13.8% |
| TIMI flow grade | |
| Grade 0 | 6.9% |
| Grade 1 | 10.3% |
| Grade 2 | 3.4% |
| Grade 3 | 79.3% |
| White blood cells | 10.13 (5.8 - 18.3) ± 2.94 |
| Hemoglobin | 14.49 (11.3 - 17.9) ± 1.89 |
| Platelets | 217 (99 - 312) ± 55 |
| MPV | 10.04 (8.4 - 12.2) ± 0.8 |
| Peak troponin | 3.35 (0.3 - 9.4) ± 2.6 |
| LVEF | 48.1 (35 - 60) ± 6.5 |
Descriptive Analysis
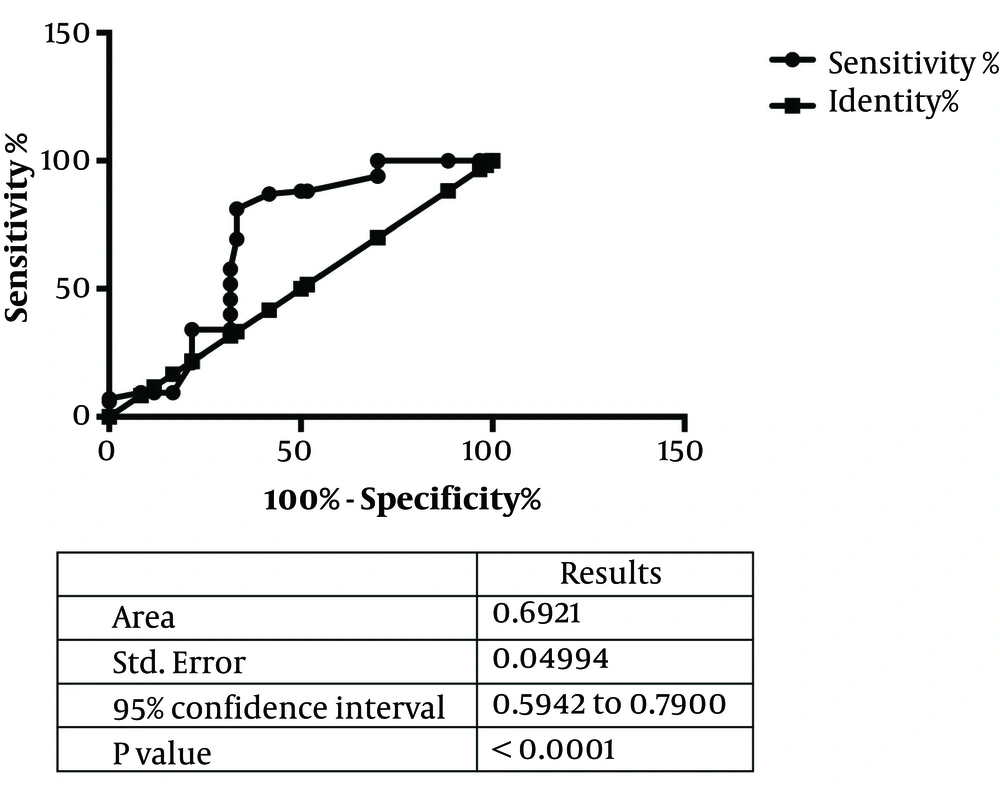
There were significant differences between the two groups (LAD and non-LAD) according to platelet count (P = 0.014), MPV (P = 0.001), HLP (0.024) and DM (0.048) (Table 2). Multivariate regression analysis showed that MPV (OR = 0.46, 95% CI = 0.27 - 0.78) and DM (OR = 0.18, 95% CI = 0.06 - 0.54) were independent predictors of LAD culprit vessel (Table 3). The significant positive correlation was also seen between MPV and LVEF (r = 0.22, P = 0.006) (Table 4). Area under curve (AUC) showed that with a cutoff point of 9.15, MPV had sensitivity of 100% and specificity of 30%, for predicting LAD as culprit vessel (Figure 1).
| Variables | LAD | Non-LAD | P Value |
|---|---|---|---|
| Age | 62.5 ± 8.4 | 62.8 ± 13.37 | 0.86 |
| Gender: Male | 70.6% | 47.8% | 0.002 |
| White blood cell | 10.44 ± 3.2 | 9.6 ± 2.4 | 0.128 |
| Hemoglobin | 14.3 ± 1.66 | 14.7 ± 2.1 | 0.65 |
| Platelets | 227 ± 47 | 204 ± 62 | 0.014 |
| MPV | 10.22 ± 0.72 | 9.78 ± 0.85 | 0.001 |
| Peak CTnI | 3.2 ± 2.7 | 3.4 ± 2.5 | 0.6 |
| LVEF | 47.9 ± 6.2 | 48.3 ± 6.9 | 0.77 |
| Smoking | 47.1% | 50% | 0.73 |
| Hypertension | 70.6% | 58.3% | 0.156 |
| Diabetes mellitus | 17.6% | 33.3% | 0.048 |
| Hyperlipidemia | 23.5% | 8.3% | 0.024 |
Comparison Variables in Patients with LAD and Non-LAD as a Culprit Vessel
| Variables | OR | 95% Confidence interval | |
|---|---|---|---|
| Lower | Upper | ||
| Gender | 0.448 | 0.136 | 1.474 |
| Platelets | 0.991 | 0.983 | 0.999 |
| MPV | 0.468 | 0.278 | 0.788 |
| DM | 0.182 | 0.061 | 0.544 |
| HLP | 3.517 | 0.908 | 13.619 |
Multivariate Analysis
| Variables | Pearson Correlation | P Value |
|---|---|---|
| Age | -0.104 | 0.211 |
| WBC | .170* | 0.041 |
| Hb | 0.098 | 0.240 |
| Plt | -0.151 | 0.070 |
| Peak CTnI | -0.110 | 0.188 |
| LVEF | .225** | 0.006 |
| Number of vessel | 0.079 | 0.343 |
Correlation of MPV with Other Variables
5. Discussion
Our findings showed that in patients with NSTEMI due to LAD lesion compared with non-LAD lesion group; MPV and HLP were significantly higher. According to high sensitivity of MPV, as a simple available inexpensive test, it could be suggested as a valuable screening test in NSTEMI patients.
Vizioli et al. examined the relationship between MPV and the risk and prognosis of cardiovascular diseases; they showed that increased MPV could be associated with cardiovascular risk (15). In another study by Bergoli et al., MPV was a predictor of coronary blood flow after percutaneous coronary intervention (PCI) (16). Gasparyan et al. also investigated the association between MPV, thrombosis and inflammation in their study, and concluded that increased MPV has a considerable association with thrombosis and inflammation and could be used as prognostic factors (12). In another study in 2010, Chu et al., investigated the MPV as a predictor of cardiovascular risk, and showed that increased MPV in acute MI had correlation with death (11). Similar to our findings in a study conducted by Liu et al. in 2014, by studying 190 patients with NSTEMI they found that MPV was a reliable efficient tool in predicting LAD obstruction in NSTEMI patients. On the other hand, B-type natriuretic peptide and ECG were not good tools in predicting LAD infarct location (17). In contrary with our findings Misumida et al. by studying 763 patients with NSTEMI found that MPV had no significant association with the incidence of LAD and non-LAD involvement, and did not have a significant role in predicting infarct site in NSTEMI patients (18). In a study by Misumida et al., MPV in LAD culprit group was higher than non-LAD culprit groups (8.6 vs. 8.4 respectively) (P value = 0.72). Contrary to this study, Liu et al. showed that MPV of LAD culprit group was smaller than those with left circumflex or right coronary arteries (9.0 ± 1.5 versus 9.8 ± 1.6, P < 0.001). Our study showed a significantly higher MPV in LAD culprit group, so the results of current studies are controversial and more studies are needed for a better understanding about the role of MPV and culprit lesion and prognosis of patients with ischemic heart disease. Yazici et al. showed the correlation between left ventricular ejection fraction (LVEF) and MPV. They defined depressed LVEF as LVEF ≤ 50%. Lower MPV was associated with depressed LVEF (P = 0.02) (19). MPV is associated with inflammation (20). Hence, some factors associated with LAD lesions such as lower LVEF in some cases and higher inflammation because of more extensive necrosis might be triggers of higher MPV in NSTEMI with LAD culprit lesion.
5.1. Limitations of Study
Our study was a cross sectional study. A cohort study following the outcome of peoples with higher MPV according to future occurrence of ischemic heart disease is needed for better results. In all patients, determining the culprit lesion was done by patients’ corresponding interventional cardiologist and it is possible that some difficulties in determining exact culprit lesion during procedure affect our results.
5.2. Conclusion
In conclusion, our findings indicated that MPV might have a predictive value in identifying culprit lesions in NSTEMI patients.