1. Introduction
Cardiac hemangioma was an extremely rare cardiac tumor. Previous research found hemangioma in only 2.8% of all primary heart tumors, with women being somewhat more affected than males (1); in around one-third of instances, it is found in the right ventricle. One-third of the instances were documented in the left ventricle, 23% in the right atrium chamber, and 7% in the left atrium chamber (2).
According to vascular classification in pathology, hemangiomas are categorized as follows: (1) Cavernous tumor; (2) arteriovascular tumor; (3) capillary; and (4) mixed type (2, 3).
Hemangioma symptoms include outflow tract obstruction, arterial compression, cardiac dysrhythmias, embolization, syncope, and sometimes rapid death in the first presentation, among others. Depending on the anatomical location and size of the tumor (3-6) due to the vascular nature and hemodynamic consequences of hemangioma surgery, the course is very unpredictable and surgery is only recommended for symptomatic cases (7).
2. Case Presentation
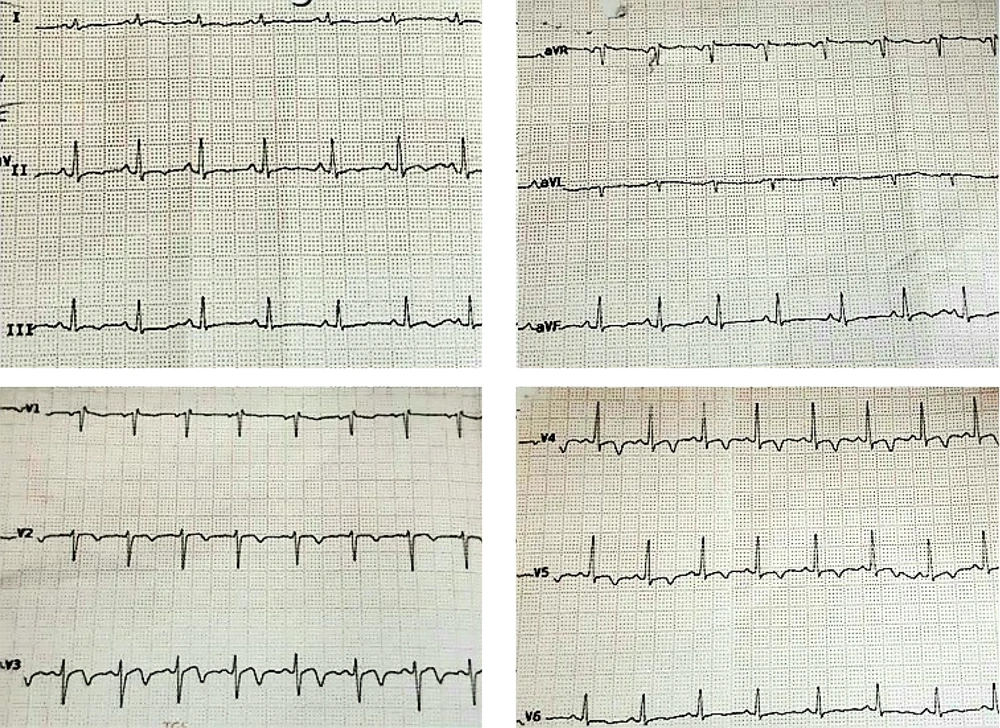
A 26-year-old woman, who was a candidate for in vitro fertilization (IVF) due to infertility, referred to the cardiology clinic for permission to perform the procedure. According to the changes in the electrocardiogram (ECG), the patient was referred for echocardiography. The patient was clinically asymptomatic and the physical examination was normal (Figure 1).
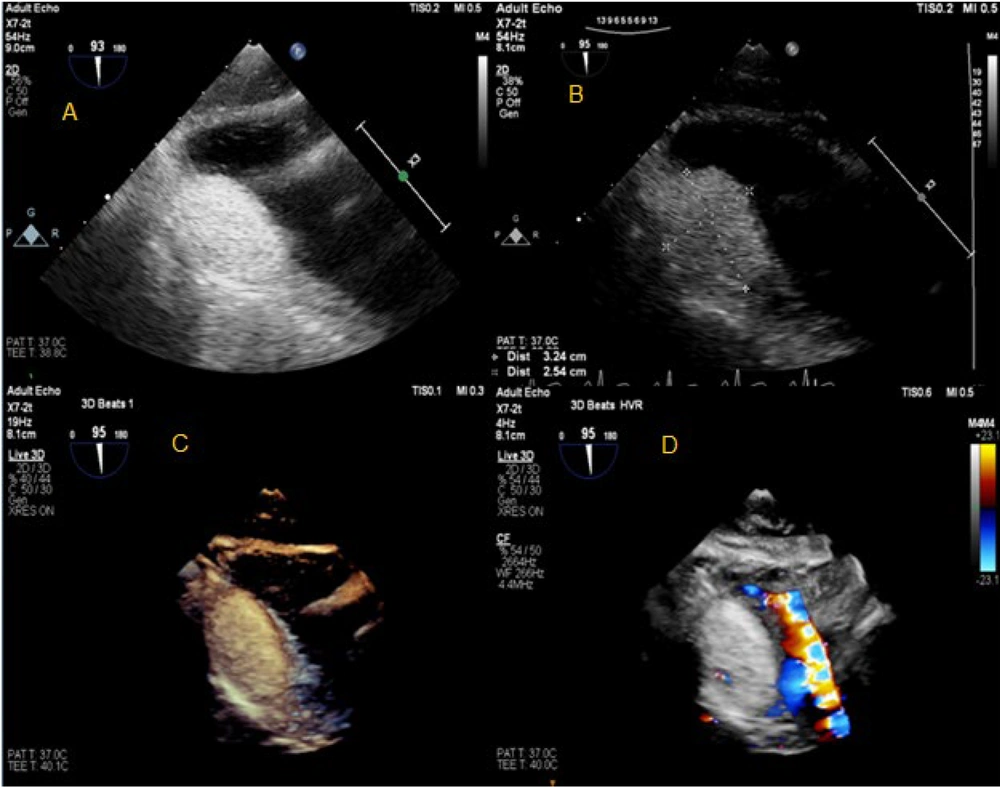
Transthoracic and transesophageal echocardiography revealed normal LV size with minor LV systolic dysfunction (EF = 50%), adequate contractility of the LV base and mid, but mildly impaired contractility of the LV at the site of LV mass. A large hyperechoic and encapsulated vascular mass (3.5 × 2.4 cm) without mobility was seen in the left ventricle in the apicoanterior segment. The mass had resulted in left ventricular apical hypokinesia (Figures 2 and 3).
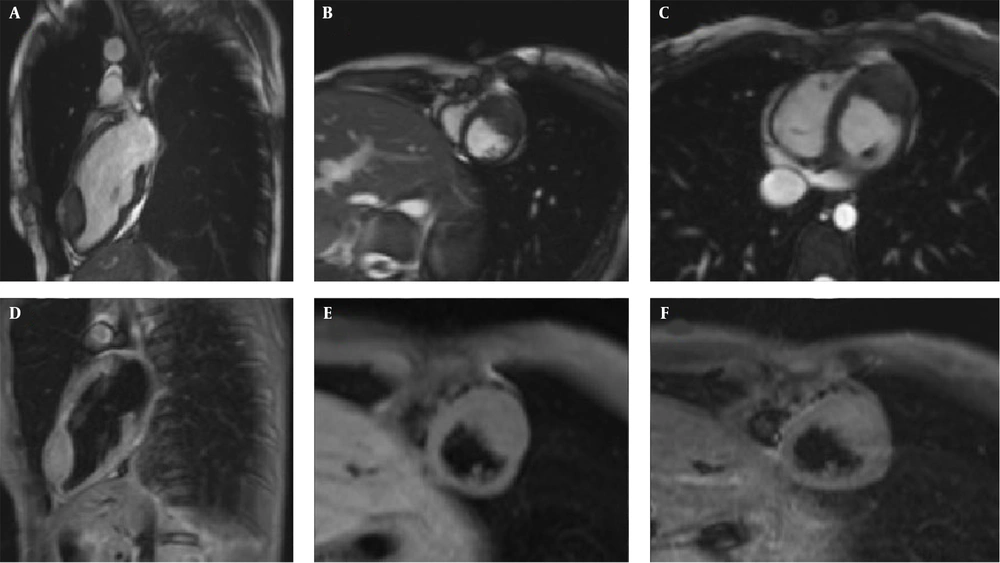
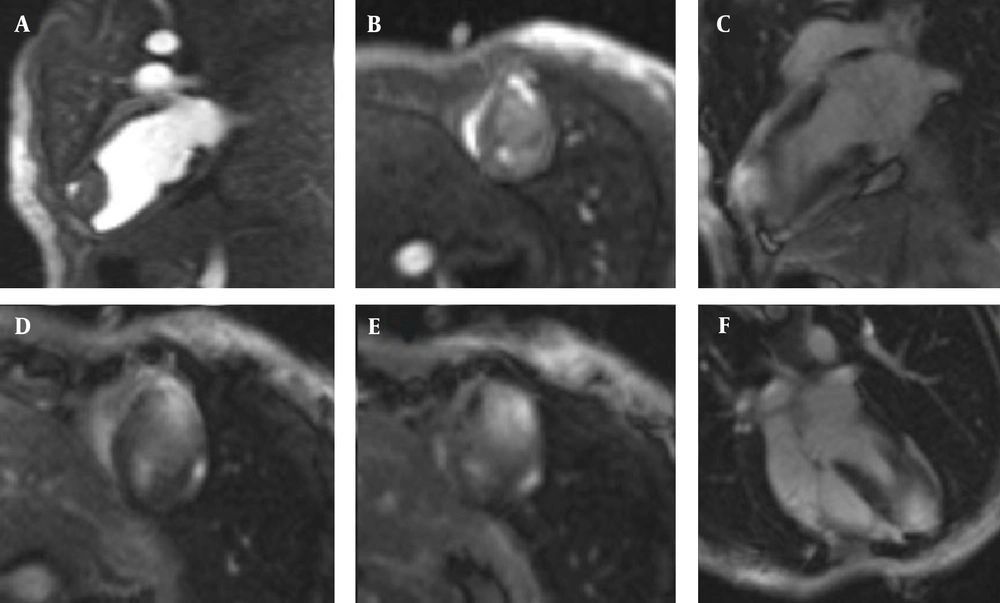
Cardiac magnetic resonance imaging (cardiac MRI) showed normal LV and RV size and function. A large mass lesion is seen in the LV apex. In the STIR/T2 weighted-sequences, the mass is ISO to high intention. In the T1 weighted-sequences with fat suppression images, the mass is ISO signal. The mass has avid perfusion during the first pass perfusion sequence. The mass is enhanced with early-enhancement imaging. The mass has been enhanced in the late-enhancement sequences. Due to MRI tissue characterization criteria: Cardiac hemangioma is the most probable diagnosis (Figures 4 and 5)
According to the evidence of cardiac hemangioma in cardiac MRI, the patient was discharged and allowed to undergo IVF.
3. Discussion
Hemangioma is caused by hyperplasia of the endothelium of blood vessels, including arterioles, tiny veins, and capillaries, and it can arise from all three layers of the endocardium, myocardium, and epicardium of the heart, but it is usually benign (2).
Imaging modalities, which include ECG and echocardiography as initial diagnostic evaluations and further computed tomography (CT), CMR, and angiography evaluations, are an essential element of its diagnosis process (8).
Some examples of ECG alterations in hemangioma have been described, which are often cases of intramuscular hemangioma and vary depending on the location of the hemangioma. For instance, in another case of hemangioma in the left ventricular apicoseptal region, the changes were in the form of T-inversion in the anterior and lateral leads (9).
In addition, echocardiography has a diagnostic accuracy of 81% for the diagnosis of cardiac tumors (8).
Ct is generally used for CMR contraindication where the mass appears as a hyper-enhanced lesion due to hyper vascularity.
Coronary angiography is seldom used for the diagnosis of hemangioma because of the appearance of tumor blush and determination of blood supply of the tumor (9, 10).
CMR plays an important role in diagnostic of hemangioma and the characteristics of signal intensity include iso-signal or hyper-signal of the mass in T1-weighted or T2-weighted imaging and rapid enhancement during the first pass-phase after gadolinium injection, indicating the high vasculature nature of the mass in favor of hemangioma, as in our patient, CMR findings were strongly in favor of hemangioma, including: In the STIR/T2 weighted-sequences, the mass is iso to high intention. In the T1 weighted-sequences with fat suppression images, the mass is iso-signal.
In the first pass perfusion sequence, the mass has an avid perfusion. And also in the early and late enhancement sequence, the mass shows enhancement.
Other tumors, however, such as pheochromocytoma, angiosarcoma, myxoma, and rhabdomyosarcoma, exhibit similar characteristics in CMR and can be identified from one another based on the patient's age, clinical manifestation, and tumor site. In addition, tumor mobility is assessed in steady-state free precession (SSFP). Therefore, according to previous studies, hemangioma can be diagnosed with CMR alone or together with other imaging methods Such as CT, echocardiography and angiography (11-13).
The natural course of hemangioma is very variable and it may be nested, stop growing or multiply. Surgery should be conducted if there are symptoms or if the diagnosis is questionable concerning the type of the tumor. Also, tumor recurrence after surgery has been reported, so follow up is required (14).
Medical treatment with radiation or corticosteroids and interferon alpha, as well as some anti-cancer drugs such as vincristine, cyclophosphamide, rapamycin, and bevacizumab, are among the treatment options for hemangioma, but the data is obviously insufficient and has not been supported by controlled studies (5, 15-17).
Since our patient was asymptomatic, a conservative management was decided upon and the patient was closely followed to inspect for symptoms and indication of surgical treatment.