1. Introduction
Digoxin is a cardiac glycoside, which is obtained from the digitalis purpurea plant. It has positive inotrope effects on heart muscles and the main indication of the drug is heart failure although it is not currently considered as the first line treatment (1). As therapeutic and toxic dosages of cardiac glycosides are almost identical, drug toxicity is common (2). Digoxin toxicity effects different parts of the body, such as the central nervous system with many side effects, such as headache, fatigue, dizziness and visual disturbances, digestive system such as nausea, vomiting, anorexia, and the cardiovascular system, such as arrhythmia (3-5). These side effects could be more dangerous in the elderly as their recuperative abilities may be inadequate as a result of numerous factors, including impaired hepatic or renal function as well as chronic disease processes (6). Intoxication with cardiac glycosides in many cases may be due to accidental intake of these substances (7, 8). Medical errors due to poor handwriting of physicians could be contributing to such mistakes (9). This case report describes a one-month consumption of the wrong medication of digoxin tablets in a none-cardiac patient.
2. Case Presentation
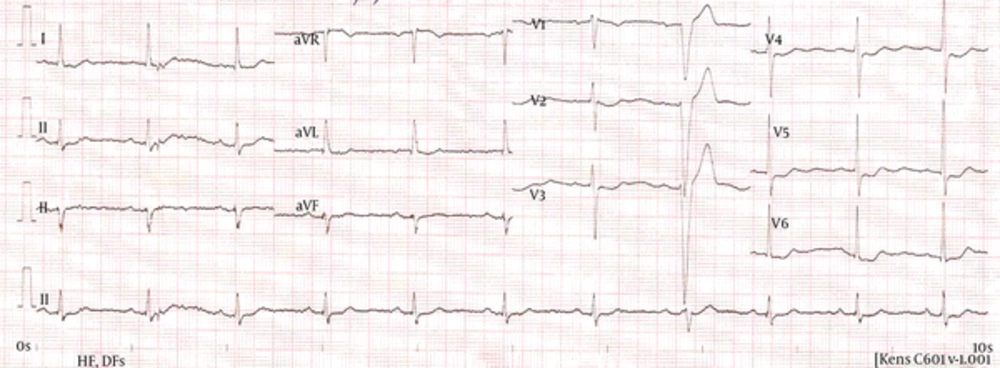
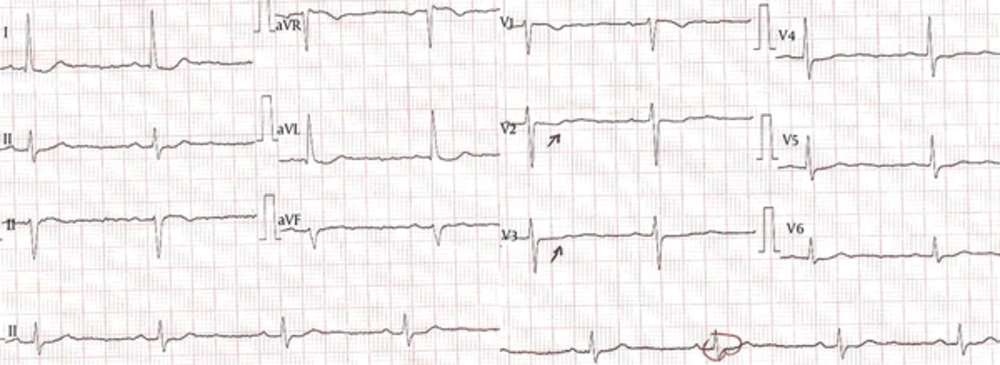
A 75-year-old female was referred to the emergency room at Valiasr Hospital of Birjand University of Medical Sciences, Iran, with gastrointestinal poisoning manifestations, nausea, and vomiting. The patient also complained about general weaknesses. She had a history of digestive problems and according to one of her family members, digestive pills have already been prescribed for her. She also had a history of hypertension and hyperthyroidism in her past medical history, which was treated with the following drugs, captopril, nitrocontin, triametern-H, amlodipine, and methimazole. Methimazole, due to hyperthyroidism control was not used at the time of admission. In reviewing her past medications with one of her family members, who is a general practitioner, it was found that instead of digestive tablets, digoxin was given to the patient mistakenly by the pharmacy operator so patient had taken 1 digoxin tablet (125 mcg), daily, for one month. Regarding the physical examination, the patient’s vital signs were as follows: systolic blood pressure = 95 mmHg, diastolic blood pressure = 65 mmHg, pulse rate = 55/minute, respiratory rate = 16/minute and temperature = 37°C. Despite usual symptoms of gastrointestinal poisoning, based on patient’s history, electrocardiogram was taken and digoxin serum concentrations were measured along with other laboratory tests, such as complete blood count and biochemical evaluation. She had bradycardia, premature ventricular contraction (PVC) and ST segment T wave changes as scooping in the initial electrocardiogram “EKG” (Figure 1). Patient’s laboratory tests were as follows: complete blood count: white blood cell = 3.2 × 1000/mm3 (Neut = 54.7%, Lymph = 43.5%, Mono = 10.8%), red blood cell = 4.22 million/mcL, hemoglobin = 12.2 g/dL, hematocrit = 37.1%, and platelet = 178 × 1000/mm3. Biochemical evaluations of blood were also as follows: blood sugar = 85 mg/dL, urea = 26 mg/dL, creatinine = 1 mg/dL, Na = 142 mEq/L, and phosphorus = 3.8 mEq/L. Serum digoxin level was 2.1 ng/mL. The patient underwent cardiac monitoring for cardiac pause and symptomatic treatments. Due to the lack of symptoms, which indicate severe digoxin toxicity (severe hypotension, lethal arrhythmias or severe bradycardia), the patient was discharged from the hospital after 4 days. Figure 2 shows patient’s EKG at discharge.
3. Discussion
Digitalis compounds were used to treat different diseases from ancient times. They are obtained from plants and increase cardiac contractility. Digoxin is one of the most important materials, which is derived from these compounds (10). Digoxin is absorbed rapidly in the digestive system and its bioavailability is between 75% and 95%. Its half-life is 3.5 to 5 days in a person with normal kidney function. Some drugs like captopril prevent the disposal of digoxin so increase its blood level (11). The patient presented in this report was also been treated by captopril due to hypertension. Digoxin inhibits sodium-potassium-activated ATPase and reduces membranous potential. This increases intracellular calcium and the activity of contractile proteins in cardiac muscles strengthens the muscle contractions (12). Chronic digoxin poisoning usually occurs in elderly people with many symptoms, such as gastrointestinal inflammation, influenza, and the alteration of consciousness. Mitchell, in a case report described evidence of ST depression and first-degree heart block in patients with nausea and vomiting (8). This shows the importance of EKG evaluation in all patients with symptoms of poisoning. Szponar et al. in another case report, presented a 45-year-old patient with typical symptoms of poisoning from gastric symptoms, nausea and vomiting to numerous severe arrhythmias and conduction disturbances (13). As in some cases, despite digoxin toxicity, normal blood levels of digoxin (< 2.8 ng/mL) have been reported (7); a careful history and physical examination are very important. Besides, due to unavailability of antidigitalis antidote and lack of methods of elimination of the drug, symptomatic treatments, correction of electrolyte disturbances and heart rate control remain effective.
Another point that should be taken into account is the physicians’ handwritings as a crucial factor for eliminating these kinds of errors. Poor handwriting undoubtedly contributes to the high incidence of medical errors, which is estimated to cause deaths of up to 30,000 people each year in Britain (9). However, ease of communication between the physician and other health care team, including nurses, could be useful in the prevention of these errors. The reason for this medication error at the pharmacy is not exactly clear but it could have been due to poor hand writing of the physician.
3.1. Conclusions
The EKG evaluation and careful examination are two essential points to exclude drug toxicity in all patients referring to the hospital with gastrointestinal symptoms, especially in elderly patients.