1. Background
The primary goal of nurses’ triage is to recognize clinical conditions significantly related to morbidity and mortality, especially in the context of overcrowding in the emergency department (ED) (1). Unfortunately, overcrowding has been a worsening problem over the past decade, and the demand for triage tools that are both accurate and efficient is increasing (2). Acute coronary syndrome (ACS) is a common complaint in ED settings, and recognizing patients with ACS in the ED remains a major challenge for clinicians. Numerous presenting symptoms and different chief complaints are attributed to different etiologies and show that significant uncertainty exists (3, 4). Nurses’ triage assessment of patients at the ED has been well documented in the literature. Cultural biases and stereotypes are reported for the triage of patients with suspicion of ACS (5-7). Unfortunately, nurses' accuracy in triaging patients with suspected ACS is as low as 54% (6-8).
The Emergency Severity Index (ESI) scale has been reported as the most commonly used scale in the triage room worldwide (9). It is used to prioritize patients based on patients’ vital signs and resource utilization in the ED (10). This tool is highly subjective because it is substantially associated with triage nurse judgment on high-risk criteria and predicting ED resource utilization (9). Thus, different scores may be assigned by different nurses based on their individual experience and knowledge (10). In addition, the ESI may be associated with poor discrimination for patients who are not high risk because nearly half of patients presenting to the ED receive an ESI score of 3 (9, 11). Furthermore, although the ESI may be used for a broad variety of chief complaints and facilitates the triage of patients regardless of their chief complaints in general hospitals, it may not be effective for triaging the specific subset of patients who are the greatest concern, such as patients with ACS (12).
Cardiac troponin-I (cTnI) can be used as a reliable diagnostic tool to help quickly identify myocardial infarction (MI) (13). This index gives more confidence to triage nurses in dealing with chest pain patients while bearing in mind that a significant proportion of chief complaints is chest pain in the ED. In 2001, Tanaka et al. showed that the sensitivity of the second-generation cTnI test for patients assessed within 3 hours after the onset, 3 - 6 h after, and more than 6h was 10, 62.5, and 75%, respectively, whereas conventional ECG diagnosis had 100% sensitivity at any time window (14). On the contrary, the specificity of the cTnI test was 100, 100, and 97.4%, whereas that of conventional ECG diagnosis was 25, 57.1, and 42.2%, respectively, for the three time windows. Patients with low-risk chest pain who probably do not have any serious underlying diseases benefit most from cTnI than ECG in the triage room.
It is worth mentioning that the newer generation of cTnI provides high specificity and specificity for the diagnosis of patients with MI in 2021. Tan et al. reported 100% sensitivity and negative predictive value (NPV) for cTnI (15). They concluded that cTnI is useful for ruling out acute coronary syndrome (ACS) with a single blood draw sample in patients presenting with chest pain in the ED (15). High specificity and NPV of cTnI make it a perfect test for prioritizing care among patients with low-risk chest pain because a positive result in a cTnI test is useful for ruling out ACS. It means the test rarely gives positive results in healthy patients. The majority of patients with low-risk chest pain (98%) will not result in short-term major cardiac events (16). In this sub-group, cTnI test is more cost-effective, less time consuming, and hypothetically more effective than ECG, especially in overcrowded triage rooms.
The original ESI handbook (ver. IV) states that immediate life-saving interventions may not be required for patients with symptoms suspicious for ACS until hemodynamic instability and acute respiratory distress (ESI level 1 criteria) are not present (10). Thus, patients with the presence of high-risk criteria for MI will be categorized into ESI level 2. In addition, “high-risk situation” criteria mentioned in the second decision point of ESI are strictly dependent on the triage nurse’s ability to find a connection between the patient’s condition and MI trajectory; thus, it contributes to the substantial bias and mistriage rate. Due to the abovementioned serious limitations in the diagnostic value of chest pain for diagnosing ACS and the specific benefits of the cTnI, adding this test to the ESI triage may be effective in prioritizing patients in the triage room. Using the cTnI is inexpensive, easy, and requires less skill and time to triage patients with ACS (8, 17).
2. Objectives
The purpose of this study was to compare the accuracy of the ESI + cTnI and ESI to triage patients with low-risk chest pain in the triage room.
3. Methods
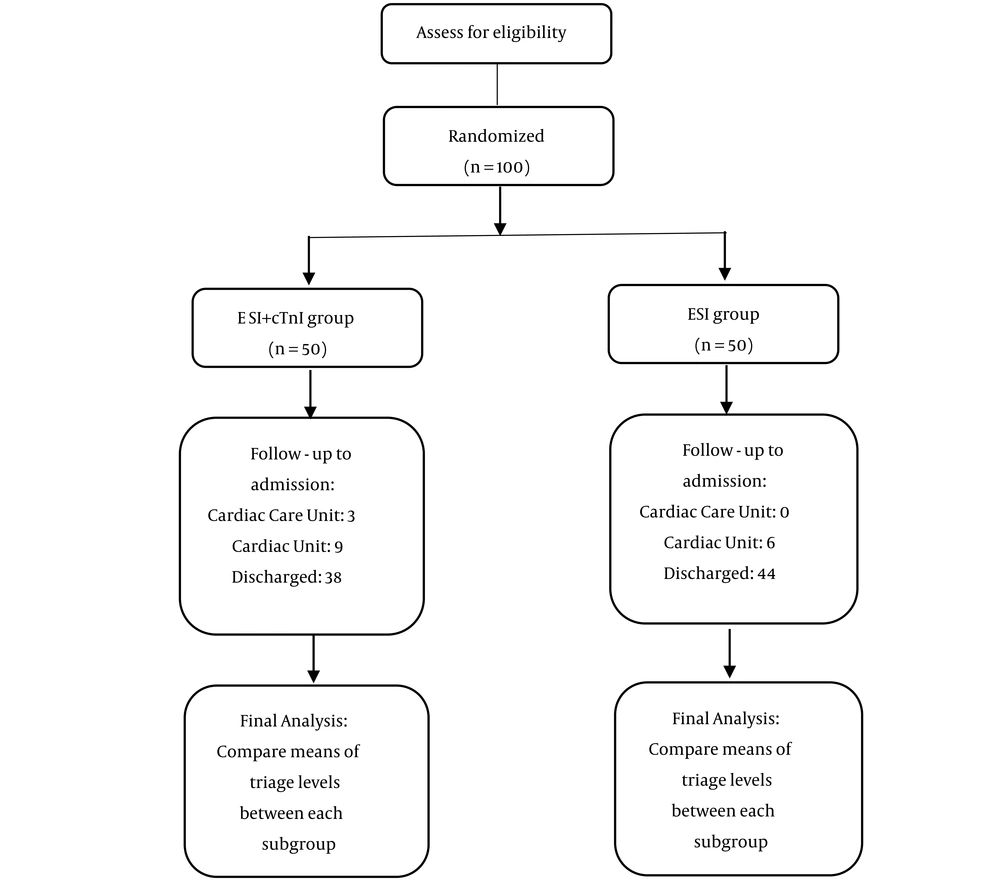
The study was conducted from January to April 2019. It was designed as a randomized clinical trial with a 6-hour follow-up to obtain short-term outcomes (Figure 1). The effects of ESI + cTnI and ESI on the mistriage of low-risk patients with acute chest pain in the ED were compared. The intervention group was composed of patients on whom the ESI + cTnI was conducted. The control group was composed of patients on whom the ESI (ver. 4) was conducted. The study was designed as a single-blind trial, and physicians and nurses in the ED were kept blind to the allocations.
3.1. Ethics
This study was conducted with the permission of the Ethics Committee of Mashhad University of Medical Sciences (IR.MUMS.NURSE.REC.1397.088). Furthermore, informed consent was obtained from patients in the ED. The study was registered at the Iranian Registry of Clinical Trials (IRCT20180410039258N1).
3.2. Setting
The study was conducted at Farabi Hospital (Mashhad, Razavi Khorasan).
3.3. Design
Patients with a chief complaint of low-risk chest pain who presented to the ED were included if: (1) at least three hours elapsed from the onset of chest pain; (2) there was absence of any high-risk criteria, such as acute onset of oppressive chest pain, crescendo quality of pain, chest pain at rest, repeated episodes of ischemic cardiac chest pain of more than 20 minutes’ duration; and (3) in case of absence of any trauma history. Patients who were initially included were randomly assigned to the intervention (ESI + cTnI) and control (ESI) groups. The enrolled patients were randomized using a computer-generated random number table. The subjects were randomized in a 1: 1 ratio to ESI + hcTnI or ESI. Sampling was conducted over weekdays, except the night shift. Triage nurses were unaware of one another’s decisions in both groups. The gender, age, triage level, vital signs [respiratory rate (RR), pulse rate (PR), and blood pressure (BP)], and clinical outcomes [ED admission, ED discharge, cardiac care unit (CCU) admission, cardiac unit (CU) admission, and number of used resources] were recorded during the first six hours of hospitalization in the ED. The door to triage room time, physician visit time, and specialist visit time were documented. The patients were excluded if: (1) diagnosed with other etiologies, including vasculitis, myocarditis, drug abuse, sepsis, pulmonary embolism, and renal failure; (2) they were transferred to another hospital; and (3) their documents were incomplete.
3.3.1. ESI + cTnI (Intervention Group)
Patients with low-risk chest pain were assigned to level 2 if their cTnI was positive; patients with negative cTnI were assigned to levels 3 to 5 based on required resources.
3.3.2. ESI (Control Group)
The validity of the ESI triage scale has already been reported in Iran (18), the ESI (ver. 4) was recruited to assign triage levels (10). Kappa statistics was used to assess reliability between two triage nurses based on 10 cases.
3.3.3. Cardiac Troponin I Rapid Test
The MoLab cardiac troponin I rapid test was used to measure the cTnI in the triage room. It is a rapid chromatographic immunoassay for the qualitative detection of human cardiac troponin I in whole blood serum or plasma as an aid in the diagnosis of myocardial infarction. A capillary tube must be used to collect finger stick whole blood specimen. The capillary tube must be filled, and approximately 100 microliter of finger stick whole blood specimen must be transferred to the specimen well of the test cassette. Then, 1 drop of buffer (approximately 40 microliter) must be added to the well of the test cassette, too. The cardiac Troponin I Rapid Test has been evaluated with a leading commercial cTnI EIA test using clinical specimens. The result is considered positive when two lines appear. One colored line should be in the control line region (C), and the other apparent colored line should be in the test line region (T). The result is considered negative when one colored line appears in the control line region (C). No line must be appeared in the test line region (T). The result is invalid if the control line fails to appear. It is reported that the sensitivity of the cardiac troponin I rapid test cassette is 99.4% (95% CI: 96.8 - 99.9%), its specificity is 99.0% (95% CI: 97.6 - 99.7%) relative to the leading EIA Test, and its accuracy is 99.1% (95% CI: 98.0 - 99.7%). Pearson's coefficient statistics was used to assess test-retest reliability based on 10 cases.
An expert panel defined mistriage as undertriage and overtriage rates. Overtriage was considered as the percentage of Troponin negative patients who had received triage level 1 or 2 in each group. Undertriage was defined as the percentage of low-risk chest pain patients who had not received a triage level and were referred to outpatient clinic out of the ED. Used resources were defined by the Emergency Severity Index (ESI) Implementation Handbook (ver. IV). The number of various types of resources, not individual tests, were counted; for example, complete blood cell count (CBC) and electrolytes equal one resource, while CBC plus chest X-ray equal two resources.
3.4. Statistical Analysis
The descriptive data were expressed as mean, standard deviation (SD), and percentage. The Mann–Whitney U test, independent t-test, and chi-square statistics compared variables between the two groups. All the analyses were performed using SPSS, version 16.0. A post hoc power analysis was performed based on the mean difference of triage levels (discharged patients from the ED: ESI + hcTnI 3.92 + 0.27; ESI 3.0 + 0.00), and it showed that our study with the effect size of 4.81 and power of greater than 0.80 had an adequate sample size.
4. Results
One hundred patients were enrolled, 50 in the ESI + cTnI group and 50 in the ESI group. The sociodemographic characteristics of the samples are shown in Table 1. Their age ranged from 21 to 91 years old. Physicians diagnosed 19.1 and 12% of the patients as having changes in ECG in the ESI + cTnI and ESI groups, respectively (chi-square: 2.43; df = 1, P = 0.118). Three patients were admitted to the CCU due to suspected changes in ECG and discharged after 24 hours without any further complications, while their troponin remained negative during admission. In the ESI + cTnI group, 70% of the patients were assigned to level 4 and others to level 3. In the ESI group, all the patients were assigned to level 3 (Table 1).
| Characteristics | All | ESI + cTnI | ESI | P-Value |
|---|---|---|---|---|
| Age (y) | 52.9 ± 13.92 | 54.8 ± 10.00 | 49.8 ± 15.6 | 0.08 |
| Gender (male) | 49 (49) | 27 (54) | 22 (44) | 0.31 |
| Triage level | 100 (100) | 50 (50) | 50 (50) | - |
| Triage level III | 65 (65) | 15 (30) | 50 (100) | 0.001 |
| Triage level IV | 35 (35) | 35 (70) | 0 (0.0) | |
| Used resources | 3.19 ± 0.849 | 3.34 ± 0.982 | 3.04 ± 0.669 | 0.49 |
| Used resources level III | 3.06 ± 0.74 | 3.13 ± 0.99 | 3.04 ± 0.669 | 0.73 |
| Used resources level IV | 3.43 ± 0.979 | 3.43 ± 0.979 | - | - |
| Dispositions | ||||
| Discharge | 82 (82) | 38 (76) | 44 (88) | 0.13 b |
| Cardiac unit (CU) | 15 (15) | 9 (18) | 6 (12) | |
| Cardiac care unit (CCU) | 3 (3) | 3 (6) | 0 (0.0) | |
| Timing indicators | ||||
| Triage time (min) | 4.71 ± 1.50 | 4.08 ± 1.32 | 5.34 ± 1.42 | 0.001 |
| Time to physician visit (min) c | 11.11 ± 3.53 | 10.86 ± 3.15 | 11.36 ± 3.89 | 0.644 |
| Time to cardiologist visit (min) c | 161.0 ± 144.0 | 46.93 ± 30 | 262.0 ± 128.0 | 0.001 |
| Time to final decision (min) | 116.0 ± 105.0 | 35.78 ± 23 | 198.0 ± 91.0 | 0.001 |
| Vital signs | ||||
| Systolic blood pressure (mmHg) c | 141.0 ± 19 | 142.0 ± 20 | 139.0 ± 18.0 | 0.452 |
| Diastolic blood Pressure (mmHg) | 86.10 ± 9.22 | 86.10 ± 9.21 | 86.10 ± 9.32 | 1.00 |
| Heart rate (bpm) c | 80.93 ± 5.71 | 81.40 ± 6.03 | 80.46 ± 5.39 | 0.414 |
| Respiratory rate (per min) c | 17.06 ± 1.22 | 17.30 ± 1.19 | 16.82 ± 1.20 | 0.049 |
| Temperature (C) | 37.1 ± 0.25 | 37.10 ± 0.19 | 37.11 ± 0.29 | 0.950 |
Comparison of Sociodemographic Characteristics between the ESI + cTnI and ESI Groups a
The triage levels assigned to the patients discharged from the ED and CU patients are shown in Table 1. The triage level was compared between the ESI + cTnI and ESI groups among CU patients and those discharged from the ED (Table 2). Triage level was significantly different between the ESI + cTnI and ESI groups (U = 375; P = 0.001). Triage level was significantly different between the ESI + cTnI and ESI groups with regard to patients discharged from the ED (U = 66.0; P = 0.001) (Table 2). Undertriage rate was 0 and 0%, and overtriage rate was 6% and 88% for the ESI + cTnI and ESI groups, respectively.
| Triage Level | All | ESI + cTnI | ESI | P-Value |
|---|---|---|---|---|
| Of whole patients | 3.35 ± 0.47 | 3.7 ± 0.46 | 3.0 ± 0.00 | 0.001 |
| Of discharged patients | 3.42 ± 0.49 | 3.92 ± 0.27 | 3.0 ± 0.00 | 0.001 |
| Of cu patients | 3.0 ± 0.00 | 3.0 ± 0.00 | 3.0 ± 0.00 | 1.0 |
| Of ccu patients | 3.0 ± 0.00 | 3.0 ± 0.00 | - | - |
| Used resources a | ||||
| In discharged patients | 3.18 ± 0.87 | 3.5 ± 1.03 | 2.91 ± 0.60 | 0.004 |
| In CU patients | 3.33 ± 0.72 | 2.89 ± 0.60 | 4.00 ± 0.60 | 1.0 |
| In CCU patients | 2.67 ± 0.57 | 2.67 ± 0.57 | - | - |
Comparison of Patients’ Characteristics between the ESI + cTnI and ESI Groups with Regard to Admission Status
The used resources were not significantly different between the ESI + cTnI and ESI groups (U = 1061; P = 0.15). The used resources were significantly different between the ESI + cTnI and ESI groups with regard to patients discharged from the ED (U = 553; P = 0.004) and CU patients (U = 3; P = 1.0). In the ESI + cTnI group, the used resources were not significantly different among triage levels (U = 206; P = 0.2). The used resources could not be compared between triage levels in the ESI group because all the patients were only assigned to level 3.
4.1. Reliability of Triage Scales
Four triage nurses in the ESI group and one triage nurse in the ESI + cTnI group triaged the patients. The mean nurses’ ED experience was 12 years for the ESI group and 14 years for the ESI + cTnI group. The kappa coefficient of reliability between the nurses was almost perfect in the ESI group. The kappa was 0.81 (CI 95%: 0.63 - 1.00). The test-retest reliability was 1, which was assessed via a Spearman's coefficient to determine the cTnI reliability.
5. Discussion
The ESI + cTnI produced significantly a higher triage level than the ESI did (3.7 vs. 3), which resulted in a more appropriate assignment of low-risk patients to the lower acuity level (3). The ESI + cTnI group was associated with 70% of patients assigned to level 4. It is critical because triage nurses may rarely assign low-risk chest pain patients to the level 4 or 5 safely.
In our study, no patient was assigned to level 4 by using the ESI triage scale alone because nurses suppose that more than two resources are needed for patients with chest pain. Patients with chest pain need oxygen therapy, cardiac monitoring, ECG, intra-venous (IV) nitroglycerin, and IV pain medications that results in a triage assignment of level 3 or less. Therefore, it is a great opportunity to reduce the burden of patients with chest pain in the ED. The ESI + cTnI group had significantly less mistriage than the ESI group. The majority of the patients (82%) were discharged from the ED. The triage level among the patients who were discharged from the ED (up to 6 hours) was significantly different between the two groups (3.92 vs. 3). Triage level 3 was assigned to 8% of the patients in the ESI + cTnI group, and 100% of the discharged patients in the ESI group were assigned to triage level 3. In fact, the ESI limits nurses to assign patients with chest pain to triage level 4 or 5 even if they are not severely ill, because the ESI strongly relies on immediate life-saving interventions, high risk situations, or probable resource consumption. As mentioned earlier, triage nurses assume that patients with chest pain need more than two resources in the ED, and therefore, they assign patients to the ESI level 3 if patients do not present with high-risk profile or hemodynamic instability. Since the study recruited patients with low-risk chest pain and excluded patients with hemodynamic instability, no patient was assigned to level 1 or 2. The ESI indicated that examples of ESI level I for cardiac patients include cardiac arrest, hypotension, or dysrhythmia with the signs of hypoperfusion and signs or symptoms of cardiogenic shock (10). However, the original ESI handbook states that patients presenting to the ED with symptoms suspicious for ACS may receive immediate life-saving interventions only if the ESI level 1 criteria are met (10). Therefore, patients with signs and symptoms suggesting high-risk criteria for MI will be assigned into ESI level II, and it is the same for patients with ECG order to rule out MI.
In this context, since ECG is a standard procedure to assess patients with chest pain, most nurses prefer to choose level II to reduce waiting time for patients with chest pain. In fact, the ESI handbook indicates that the 54-year-old obese female who complains of epigastric pain and fatigue is at high risk for ACS and should receive ESI level II-high-risk (10). It implies that cardiac risk factors other than chest pain contribute to the high-risk situation in level II. Mirhaghi et al. showed that high risk criteria in the ESI triage level II may easily be misinterpreted as a low-risk clinical condition by triage nurses (19). This can lead to an increased rate of undertriage in ESI triage system where triage nurses are not experts, but the overestimation may occur if triage nurses are expert and cautious toward patients with chest pain.
Since high-risk criteria for chest pain were excluded from the study, no patients were assigned to ESI level 2. Similarly, CU patients received the same triage levels between the two groups (3.0 vs. 3.0). All the patients were assigned to level 3 in both groups. Since the sample size was small, no solid interpretation was possible. Also, we did not reach the sample size we needed to perform statistical analysis among patients admitted to the CCU between ESI + cTnI and ESI group. All the patients admitted to the CCU had negative troponin in the triage room, ED, and CCU. They were also discharged after 24 hour without any further complications. The main reason to admit a patient to the CCU was cardiac risk factors and changes in ECG.
Mistriage is not a rare event in patients with chest pain in the triage room. The overtriage rate for cardiac patients may increase up to 5.5% using ESI triage scale in the ED (20).
Generally, undertriage is a serious concern, and it is more critical than overtriage in dealing with cardiac patients in the ED. Undertriage rate may increase up to 20% for cardiac patients using Australasian Triage Scale (ATS) in the ED (7). Sanders and DeVon reported that the emergency nurse triage accuracy using the ESI triage scale was 54% for patients with chest pain (8). The literature has generally focused on the association between undertriage and patients’ characteristics or adverse events. Atzema indicated that the quality of nurses’ triage decisions is an important factor because half of acute MI patients presenting to the ED were undertriaged using the Canadian Triage and Acuity Scale (CTAS), which contributed to substantial delays in door to ECG and to reperfusion therapy (21).
On the contrary to the abovementioned studies, this study focused on the triage of patients with low-risk chest pain to determine overtriage rate and the benefit of adding cTnI to the ESI in the ED. Overtriage of patients with low-risk chest pain is important because it inappropriately consumes scarce resources in the ED and reduces the sensitivity of triage nurses to risk stratification of cardiac patients (22). In contrast, it is highly probable that triage nurses undertriage patients with chest pain because the large number of patients with chest pain is one the main source of overcrowding in the ED. Since this study only included patients with low-risk chest pain and excluded patients with high-risk chest pain and hemodynamic instability, mistriage did not occur. However, ESI + cTnI could assign 70% of patients to the ESI triage level 4 safely.
The used resources must be correlated with the triage level in the ED. A valid triage scale results in patients receiving high acuity triage levels use a higher number of resources (23). The used resources were not significantly different between the ESI + cTnI and ESI groups (3.34 vs. 3.04). Physicians were kept blinded to patients’ assignment during the study, and they followed the treatment protocol for patients with chest pain, including oxygen therapy, cardiac monitoring, ECG, intra-venous (IV) nitroglycerin, and IV pain medications. CU patients used more resources than patients discharged from the ED (U = 519, P = 0.3). The used resources were not significantly different between CU and discharged patients in the ESI group because the CU sample size was too limited to reveal any possible significant difference between the two groups.
This study was limited to a relatively small sample of CU patients and CCU patients. However, it does not pose a risk to our study because only patients with low-risk chest pain were included in the study, and it is rare that patients with low-risk chest pain need to be admitted to CU or CCU. To our knowledge, this is the first study that used rapid cTnI test in the triage room to help nurses and provide more accurate triage decisions in the context of the ESI. Previously, rapid cTnI test has been widely used in the emergency setting to accelerate the diagnosis of myocardial infarction. Therefore, studies which were relevant to the subject of this study were rare, and therefore, the Discussion section may suffer from limited background of knowledge in triage emergency literature.
5.1. Conclusion
Nurses’ triage decisions are compromised by the complexity of signs and symptoms that are related to ACS and require enhanced triage tools to prioritize care for patients with time-sensitive conditions, allocate resources efficiently, and decrease morbidity and mortality. The ESI tool does not provide customized support to triage patients with suspected ACS, and there is a definite need for improvement in how nurses triage these patients. ESI + cTnI may provide a more accurate method for triaging patients with low-risk chest pain compared to the ESI alone. The ESI is associated with a substantial overtriage rate among patients with low-risk chest pain, and cTnI can substantially reduce this kind of triage error. The cTnI with an objective parameter provides precise information for triage nurses to triage low-risk chest pain patients with stable vital signs. Conclusively, it is recommended that triage nurses use cTnI to triage patients with low-risk chest pain in the ED.