1. Background
Understanding anxiety as the most common mental disorder in Iran and its psychological changes (1, 2) is very important. In particular, anxiety symptoms are very common during the Coronavirus disease 2019 (COVID-19) (3, 4), which can be a threat to people's mental health. People with high levels of coronavirus anxiety report more coronavirus fear, functional impairment, worry about coronavirus, maladaptive religious coping, hopelessness, and suicidal ideation (5, 6).
Also, increased anxiety level during the coronavirus pandemic has a key role in substance abuse (7) and can moderate the degree of drug craving in response to induced negative effects (8). Levels of Anxiety may be important not only for understanding drug use patterns (9, 10), but also psychiatric burden and severity of medical complaints that co-occur with drug use disorders. Regarding these relationships in a substance-abusing sample (11), it was found that increased anxiety was associated with increased medical and psychiatric complications associated with substance abuse (as assessed via the Addiction Severity Index (12). On the other hand, since substance use disorder (SUD) is associated with a variety of cardiovascular and metabolic diseases, it is probable that people with SUD are exposed to COVID-19 risk (13). Substance use is relatively high, and its overuse can cause hypoventilation and hypoxemia followed by cardiopulmonary and neurological complications and worsening COVID-19 consequences (14). In dealing with issues in acute conditions, affecting coping, adaptability, and the ability to overcome the existing problems are important (15). Therefore, it is necessary to identify factors that predict COVID-19-induced anxiety in drug users.
Research regarding the development of anxiety has focused on genetic factors (16), specific types of learning experiences (17), and attachment styles (18). The concept of attachment styles is one of the psychological factors that influence anxiety resulting from the coronavirus pandemic (19). Due to uncertainty resulting from the pandemic, people probably need more safety and security (20). However, insecurities about the sudden coronavirus outbreak may be exacerbated and make more insecure people less supportive of their position. For this reason, perceived risks from people simulate attachment motivational system. This is a common image that adults with a secure attachment style are more flexible in stressful situations and show adaptive coping strategies (15, 21). In support of this view, international studies have found that secure attachment is protective against post-traumatic stress symptoms (22). Insecure attachment is associated with increased perceived stress, somatization disorders, and negative emotions (23-25). Another study found that a secure attachment style reduces anxiety caused by coronavirus (26).
Recently, resilience has gained popularity as a protective agent in critical conditions (27). Resilience refers to keeping sustainable and healthy performance after a potentially vulnerable event and is a dynamic process that includes positive adaptation in facing adversities (28). Masten (2018) defines resilience as an apparent capacity potential of a dynamic system for successful adaptation to disorders that threaten the performance, survival, or development of the system (29). The American Psychological Association (APA) defines resilience as a process to return from difficult experiences and good adaptation against adversities, trauma, tragedy, threats, or important sources of stress (30). The importance of this concept results from its direct connection with the ability to respond effectively to sudden events (31). In a recent study, resilience and individual well-being have been identified as the most important COVID-19 anxiety predictors. Evidences from another study point to a negative relationship between resilience and COVID-19-induced anxiety (32, 33).
Expectancy is another source of adaptation and resilience that can lead to improved mental health during a health-related global crisis (34). The widest expectancy model defines this construct as a cognitive characteristic that indicates the perceived capacity to identify ways or strategies to achieve goals or incentives to follow goals of interest (35). Expectancy is conceptualized source that provides a tool to cope with conditions that seem uncontrollable (36). Studies have shown that people with high life expectancy, contrary to people with low life expectancy, probably adapt to life challenges and employ effective coping strategies against difficulties (36, 37). Accordingly, expectancy may increase positive emotion, satisfaction, and success while following goals, especially during stressful moments. Although studies on COVID-19 are completely new, at least two studies (34, 38) have shown that expectancy may be associated with flexibility in facing acute stressful factors related to the COVID-19 pandemic and can play a role in overcoming anxiety resulting from this crisis. In a prospective cohort study, researchers concluded that expectancy is associated with physical health, health behaviors, and many psychological and social dimensions (39).
Considering the long-term prevalence of COVID-19 and increased anxiety levels because of increasing drug abuse (7), it is necessary to pay attention to mental health, one of the present era (40), and its promotion in drug users.
Considering the long-term prevalence of COVID-19 epidemics, increasing the level of anxiety and consequently increasing the prevalence of drug abuse (7), it is necessary to pay more attention to mental health, which is one of the important goals of psychology in the present century (40), and the main concern is for those who are currently using drugs and those who are in the recovery period and are completely isolated from society. Feeling COVID-19-induced anxiety may even prevent addicts from going to an addiction clinic to start or continue treatment while starting or continuing treatment is key to their lives. In this regard, no study has investigated the predictive role of COVID-19-induced anxiety based on attachment, resilience, and expectancy styles of people who use drugs.
2. Objectives
The aim of this study was to predict the rate of COVID-19-induced anxiety based on attachment styles, resilience, and life expectancy in drug users.
3. Methods
3.1. Study Design
The present study is descriptive-analytical and kind of the correlation type. The statistical population of this study included all drug users in 2021 who were in the process of abstaining from drug consumption and attended narcotics anonymous (NA) sessions in Bojnurd. In total, 134 addicts were selected based on the available sampling method. In this regard, the researchers went to open sessions of NA and distributed all three questionnaires to the most accessible people who were willing to participate in the study and met the inclusion criteria. Informed consent was received from all participants, and they were allowed to withdraw from the study at any time without adverse consequences. Moreover, anonymity and privacy issues were discussed. Inclusion criteria included substance use over the last six months, being in the age range of 20 to 60 years, and no mental or medical illness, and the exclusion criteria included lack of interest in participation and random responses, and ignoring questions. Then, demographic information of all participants was gathered. Corona Disease Anxiety Scale (CDAS) by Alipour et al., Attachment Styles Questionnaire (AAQ) by Hazen and Shaver, Conner-Davidson Resilience Scale (C-DRS), and Miller Hope Scale (MHS) were used. Data were analyzed by Pearson correlation coefficient and stepwise regression using SPSS 18.
3.2. Tools
The research tools are as follows:
3.2.1. Conner-Davidson Resilience Scale (C-DRS)
This scale was designed by Conner and Davidson (2003) by reviewing resilience sources from 1991 to 1979. The response spectrum was a 5-point Likert scale from completely false "1" to completely true "5". The higher scores, the more resilient the respondent will be. This scale has 25 items and five factors of spiritual effects, individual competence, individual instinct trust, negative motion tolerance, positive change acceptance, and secure relations. To confirm validity, the correlation of each item was estimated with the total score, and then factor analysis was used. The reported validity coefficient was 0.87. The reliability coefficient resulting from Cronbach's alpha was 0.89 (41). Khorrami et al. (2020) reported the validity coefficient of this scale as 80% (42). In the current study, test reliability was 0.79 using Cronbach’s alpha.
3.2.2. Miller Hope Scale (MHS)
This questionnaire was designed by Miller and Powers (1988). This scale includes 48 questions that are scored based on a 5-point Likert scale from completely disagree “1” to completely agree “5” where 48 and 240 show complete hopelessness and expectancy, respectively. This is a diagnostic test and, for the first time, was used to assess the life expectancy of patients with heart diseases in the United States to show 48 aspects of expectancy and helplessness. Twelve items of the MHS are negative that these items receive inverse scores in assessment. Six assistant professors reconfirmed this questionnaire in the United States in terms of proposed elements for expectancy and coordination of articles, and accuracy in selecting different aspects regarding behaviors that express hope. Miller has reported the validity of this questionnaire using Cronbach's alpha as 0.80 (43). The reliability of this scale in a study by Ebadirad (44) was estimated to be 0.91 and 0.87 based on Cronbach’s alpha and bisection methods, respectively. To estimate validity, total scale and criterion question scores that were obtained simultaneously were correlated, and validity coefficients of 0.64 and 0.001 were obtained. In the current study, its reliability was 0.83 using Cronbach’s alpha method.
3.2.3. Corona Disease Anxiety Scale (CDAS)
This scale was designed by Alipour et al. (2019) to determine COVID-19-induced anxiety in a clinical sample. This scale has been designed and validated by Alipour et al. (2020) to assess anxiety resulting from coronavirus in Iran. The final version of this scale includes 18 items and two components. Items one to nine assess mental signs, and items ten to 18 assess physical signs. This scale is scored based on a 4-point Likert scale from 0 (never) to 3 (always); therefore, the maximum and minimum scores that respondents obtain are between 0 and 54. Higher scores in this questionnaire indicate a higher level of anxiety in people. In a study by Alipour et al. (2020), reliability of this scale was obtained using Cronbach’s alpha for the first and second factors as 0.87 and 0.86, respectively. Also, the correlation between this questionnaire and the Mental Health Questionnaire was from 0.26 to 0.50 (45). In the current study, its reliability was obtained 0.89 using Cronbach’s alpha method.
3.2.4. Revised Adult Attachment Scale (RAAS)
This scale was designed by Collins and Reed (1990) and revised in 1996. This scale has 18 items that respondents express their agreement or disagreement based on a 5-point Likert scale. This scale includes three scales of secure, anxious, and avoidant attachment styles. Each subscale has six phrases. Test-retest reliability coefficients for these three subscales were 0.68, 0.71, and 0.52, respectively. Cronbach's alpha in all cases was equal to or larger than 0.80 (46). In Iran, the reliability of this test was reported at the level of 0.95. Ghahremanlou et al. (2021) reported its reliability using Cronbach’s alpha for subscales of secure, avoidant, and emotional as 0.70, 0.79, and 0.80, respectively (15). In the present study, its reliability for secure, avoidant, and emotional styles were 0.75, 0.77, and 0.84, respectively.
4. Results
In Table 1, the demographic characteristics of participants in the study are presented. Moreover, using a t-test and analysis of variance, coronavirus anxiety was compared with respect to demographic characteristics.
| Variables and Groups | N | Mean ± SD | t | f | P-Value |
|---|---|---|---|---|---|
| Gender | 1.20 | - | 0.23 | ||
| Male | 92 | 28.97 ± 14.44 | |||
| Female | 42 | 25.76 ± 14.26 | |||
| Marital status | -2.39 | - | 0.018 | ||
| Single | 54 | 24.40 ± 13.81 | |||
| Married | 80 | 30.37 ± 14.38 | |||
| Education | - | 1.76 | 0.173 | ||
| Middle school and lower | 58 | 30.50 ± 16.34 | |||
| Diploma | 67 | 26.40 ± 12.48 | |||
| B.A and higher | 9 | 27.97 ± 14.41 |
Table 1 shows that married people obtained larger mean scores regarding COVID-19-induced anxiety (P < 05). No difference was observed between mean scores of COVID-19-induced anxiety by gender and education. In Table 2, descriptive characteristics of the variables and correlation test results between research variables are presented.
| Variables | COVID-19-Induced Anxiety | Mean ± SD | |
|---|---|---|---|
| r | P-Value | ||
| COVID-19-induced anxiety | - | 27.97 ± 14.41 | |
| Resilience | -0.86 | 0.001 | 71.32 ± 27.16 |
| Life expectancy | -0.552 | 0.001 | 22.07 ± 8.46 |
| Attachment styles | |||
| Secure | -0.35 | 0.001 | 13.46 ± 6.64 |
| Avoidant | 0.29 | 0.001 | 20.88 ± 6.41 |
| Ambivalent | 0.28 | 0.001 | 21.95 ± 6.97 |
As shown in Table 2, a significant negative relationship was found between COVID-19-induced anxiety and resilience (-0.86), life expectancy (-0.55), and secure attachment (-0.35) style. Also, COVID-19-induced anxiety had a significant and positive relationship with avoidant (0.29) and ambivalent (0.28) attachment styles. Then, using regression, COVID-19-induced anxiety was predicted based on attachment styles, resilience, and life expectancy. Multiple correlation coefficient was found between independent variables (attachment styles, resilience, and life expectancy) and COVID-19-induced and attachment styles, resilience, and life expectancy could predict 87% (R2) of COVID-19-induced anxiety changes. The beta coefficient of research variables is presented below in explaining dependent variable changes (Table 3).
| Variables | Beta | P-Value | R2 |
|---|---|---|---|
| Resilience | -0.83 | 0.001 | 0.87 |
| Life expectancy | -0.10 | 0.049 | |
| Attachment styles | |||
| Secure | -0.30 | 0.004 | |
| Avoidant | -0.17 | 0.03 | |
| Ambivalent | -0.21 | 0.03 |
As can be observed in Table 3, all beta coefficients of independent variables (resilience, life expectancy, avoidant, secure, ambivalent) are significant. The largest beta coefficient was related to resilience, and the smallest coefficient was related to life expectancy.
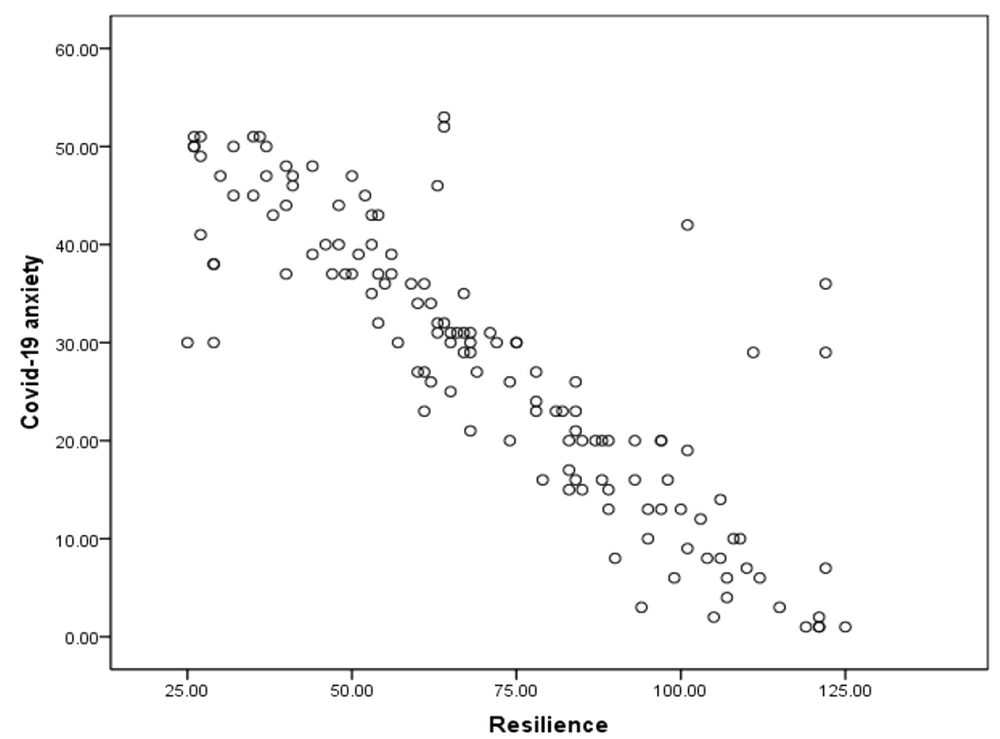
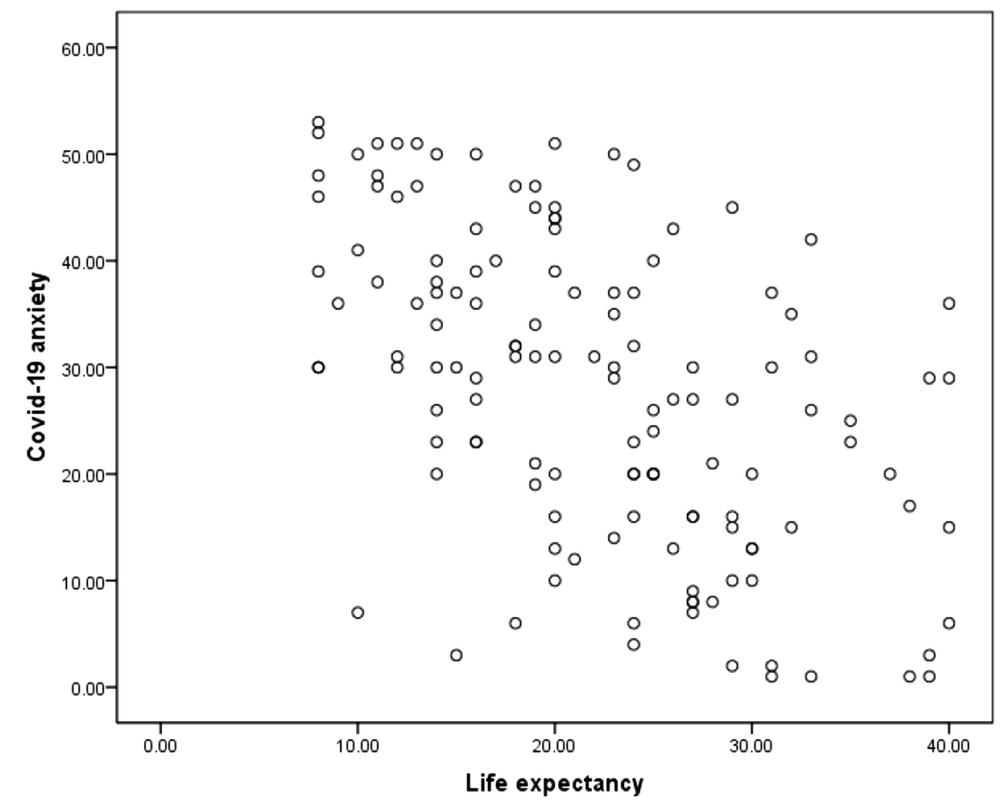
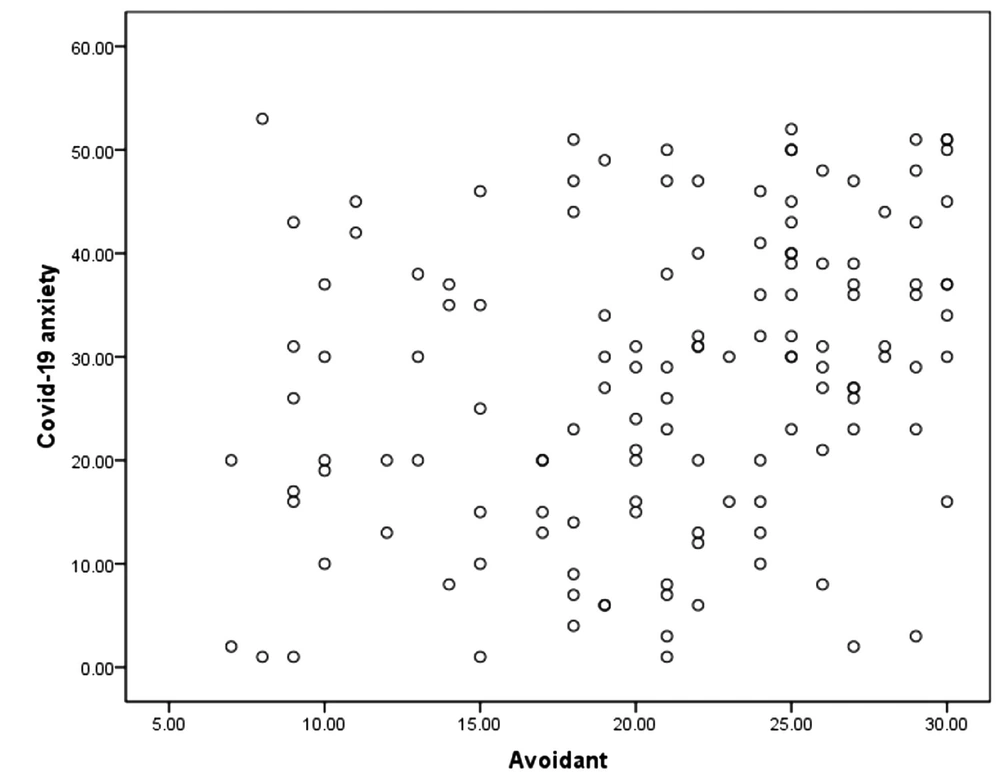
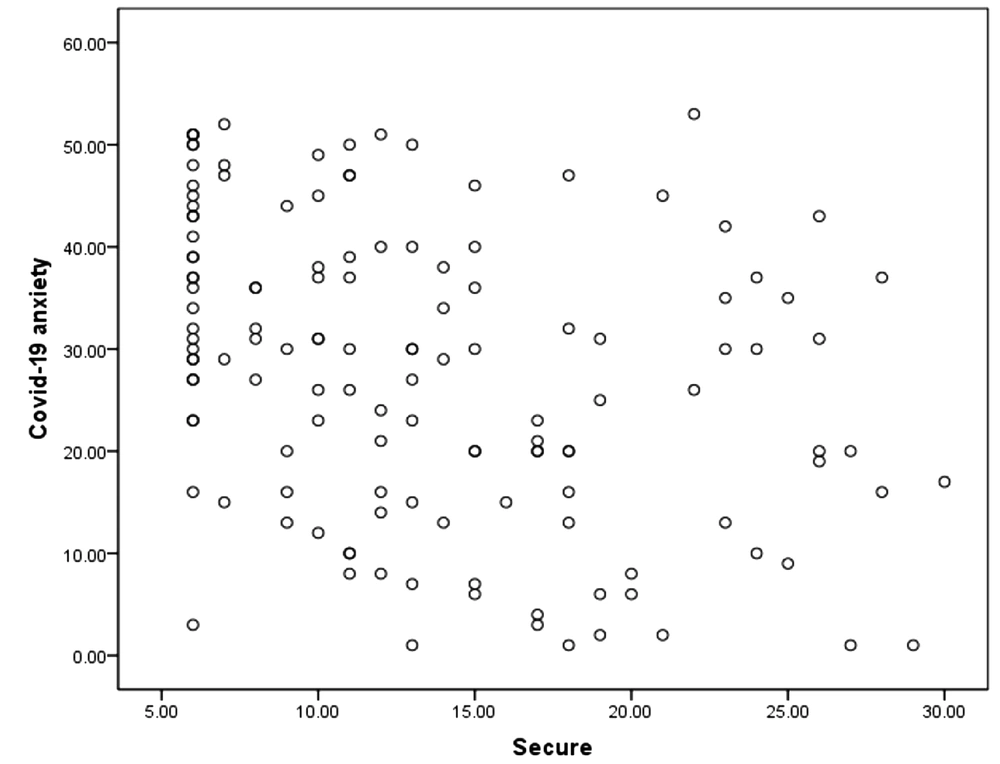
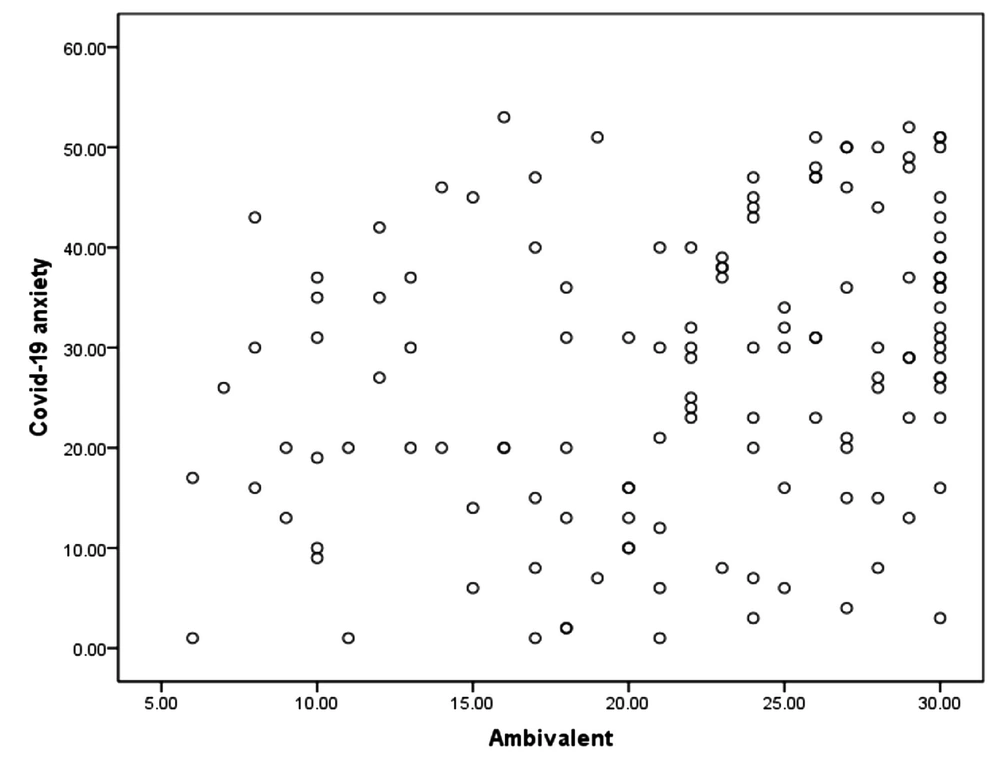
In Figures 1 to 5, the diagram of the relationship between independent and dependent variables is presented.
As can be seen in Figure 1, data related to COVID-19-induced anxiety and resilience are not dispersed and are in the same direction.
As can be seen in Figure 2, data related to COVID-19-induced anxiety and resilience are not dispersed and are in the same direction.
As can be seen in Figure 3, data related to COVID-19-induced anxiety and avoidant attachment are not dispersed and are in the same direction.
As can be seen in Figure 4, data related to COVID-19-induced anxiety and secure attachment are not dispersed and are in the same direction.
As can be seen in Figure 5, data related to COVID-19-induced anxiety and ambivalent attachment are not dispersed and are in the same direction.
5. Discussion
The purpose of this study was to investigate COVID-19-induced anxiety prediction based on attachment styles, resilience, and life expectancy in people who use drugs. The findings showed that secure attachment style is a negative predictor of COVID-19-induced anxiety and insecure, avoidant, and ambivalent attachment styles are positive predictors of COVID-19-induced anxiety. This is consistent with previous studies (22, 24-26). Silverman and Weems (1999) first raised the possibility that insecurely attached individuals could be predisposed to misinterpret benign symptoms of anxiety as being catastrophic (47). On the basis of this suggestion, Weems et al. (2002) used two student samples (viz., high school and undergraduate students) to test the hypothesis that insecurely attached individuals have higher levels of anxiety (18). Therefore, these people had secure relationships with their mothers during childhood and have generalized what they had learned. Hence, due to having a secure feeling about interactions, whether face-to-face or virtual, these people use more self-disclosure and a greater sense of intimacy and more constructive coping styles and try to lower their anxiety levels.
Another finding of this study showed that avoidance attachment style has a positive relationship with COVID-19-induced anxiety. Weems et al. (2002) believe that insecurely attached individuals may distort, selectively encode, and be more fearful of anxiety-related sensations because they think they are unable to help themselves or obtain help from others (18). For this reason, people with this style perceive the pandemic as a symbol of isolation, loneliness, and death, especially in the marginalized community of addicts who have limited connections to healthy people. Moreover, it should be said that their concerns about losing these limited connections increase their anxiety during quarantine.
In the current study, ambivalent attachment style showed a positive relationship with COVID-19-induced anxiety, but in some studies, lower levels of anxiety were found in this style. In explaining such conflicting findings, it can be said that these people, due to their attachment style, prefer to suppress their dependence on others and stay at home and quarantine themselves. In this case, they experience lower anxiety during the pandemic. In other situations where they feel isolated, greater anxiety is reported due to social distancing and quarantine. Drug users are no exception to this rule.
Another finding of this study showed that resilience is a negative predictor of COVID-19-induced anxiety. This is consistent with the results of previous studies (32, 33). In explaining this finding, since resilience is an ability to resist changes (48) and is defined as a positive potential for coping with stress (49), it can be said that it is one of the major factors in coping with the disease (50). About resilience functioning in lowering anxiety, its main components, such as competence, positive acceptance, self-confidence, control, and spiritual effects, act as a barrier against anxious situations and suppress anxiety (51). These components have central importance in treatment sessions in NA, especially when all 12-step programs of this community are around spirituality. Therefore, drug users with high resilience resist anxious and stressful situations due to high flexibility and do not suffer from psychological complications, such as anxiety and depression.
Moreover, the findings of this study showed that life expectancy is a negative and significant predictor of COVID-19-induced anxiety. This finding is consistent with previous studies (34, 38, 39). In explaining this finding, it can be said that expectancy is an important element in the therapeutic sessions of NA. This element helps people to identify goals, various ways to achieve goals, create motivation, and remove barriers through creative methods (52). Human has positive and negative dimensions, and expectancy is at the core of the positive dimension and leads to the formation of optimistic thoughts about the world and coping with challenges and their destructive effects on various life levels. Learning such a thinking style and sufficient sources to achieve goals makes life significant (42) that is an effective technique to cope with stress and anxiety. Indeed, people who use drugs in NA sessions use positive and constructive self-talk to cope with stress and learn to get prepared for the worst situations and hope for the best situations at the same time and coordinate them with their own values. Therefore, these people receive positive energy and ideas during NA sessions to learn how to use problem-oriented coping techniques, employ effective coping strategies, such as books, physical activity, and exercise and receive psychosocial support from their families instead of blame, rumination, and avoidance of problems.
Several limitations of this study need to be considered when interpreting the results. The cross-sectional nature of the study precludes drawing conclusions about the direction of relations between attachment experiences and the development of COVID-19-induced anxiety. Since substance use and deaths in Northern Khorasan province are more prevalent among men (53), the sample of this study includes a smaller percentage of women with substance use, and it is suggested to include equal male and female participants in future studies. Moreover, this study only investigated substance use and did not consider internet or behavioral addictions that may be related to COVID-19-induced anxiety. Therefore, it is suggested to investigate the relationship between COVID-19-induced anxiety and other addictions. Finally, it is suggested to consider and study gender differences based on other protective variables.
5.1. Conclusion
In summary, this study was conducted on drug users for the first time in Iranian society. The findings of the current study clearly show the predictive power of COVID-19-induced anxiety based on attachment styles, resilience, and expectancy in drug users. After comparisons with other studies conducted outside Iran, it was observed that the resulted levels and relationships in this study are different from previous studies, but at the same time, the general results of this study are consistent with previous studies. This study provides further support for the role of interpersonal factors in the development of COVID-19-induced anxiety and suggests the need for continued investigation into parental practices and childhood learning experiences as well as resilience and life expectancy of people in the development of such risk factors for psychopathology.