1. Introduction
Circle of Willis (CoW), described by Thomas Willis, is an anastomotic structure with a polygenic shape that supplies blood to the brain (1). CoW consists of the anterior cerebral artery (ACA), posterior cerebral artery (PCA), anterior communicating artery (AcoA), posterior communicating artery (PCoA), and internal carotid artery (ICA), which are arranged in a circular formation making a circle at the base of the brain (2).
Studying CoW was formerly mostly based on cadaver autopsies, but with the introduction of magnetic resonance arthrography (MRA), a non-invasive high-resolution modality was utilized for a non-contrast, non-radiating CoW evaluation. Many variations are discovered in CoW among various populations. Some of these variations present clinical significance, including increased risk of stroke and occlusion of ICA in PCoA hypoplasia or absence and transient ischemic attack (TIA) (3). In this article, we discuss the case of a 50-year-old male with a chief complaint of headache.
2. Case Presentation
A 50-year-old male presented with a chief complaint of exacerbation of headaches was referred with a sudden onset headache in the right temporal lobe. The patient reported a history of milder generalized headaches. The patient did not complain of nausea and vomiting and did not experience loss of consciousness (LOC). There was no sign of weakness or numbness in either upper or lower limbs. Moreover, there have been no signs of visual impairments, including hemianopia or diplopia. No underlying medical condition or procedure was reported. On examination, the patient was ill but not toxic. The patient was alert and oriented and had a Glasgow Coma Scale (GCS) of 15. On general examination, vital signs were normal, and there was no significant finding. Neurological examinations and muscle tone were normal. Laboratory reports revealed an elevated low-density lipoprotein (LDL) to the upper limits of the normal range, and the electrocardiogram (ECG) appeared normal.
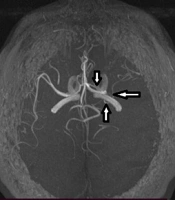
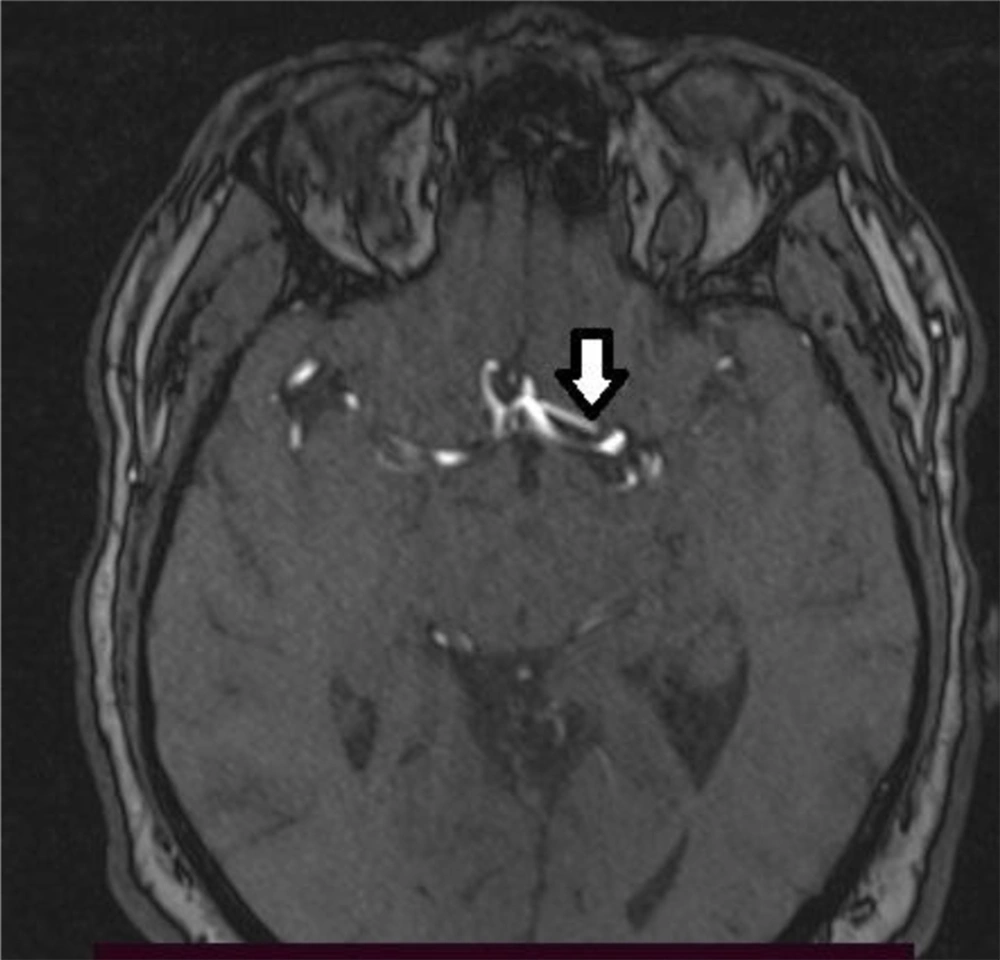
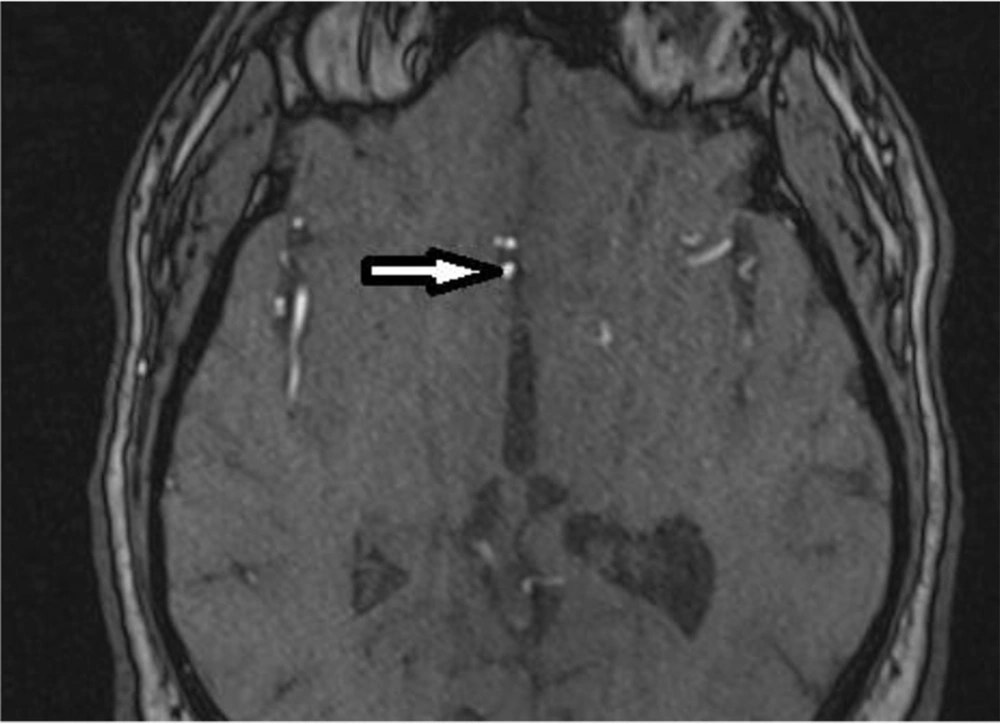
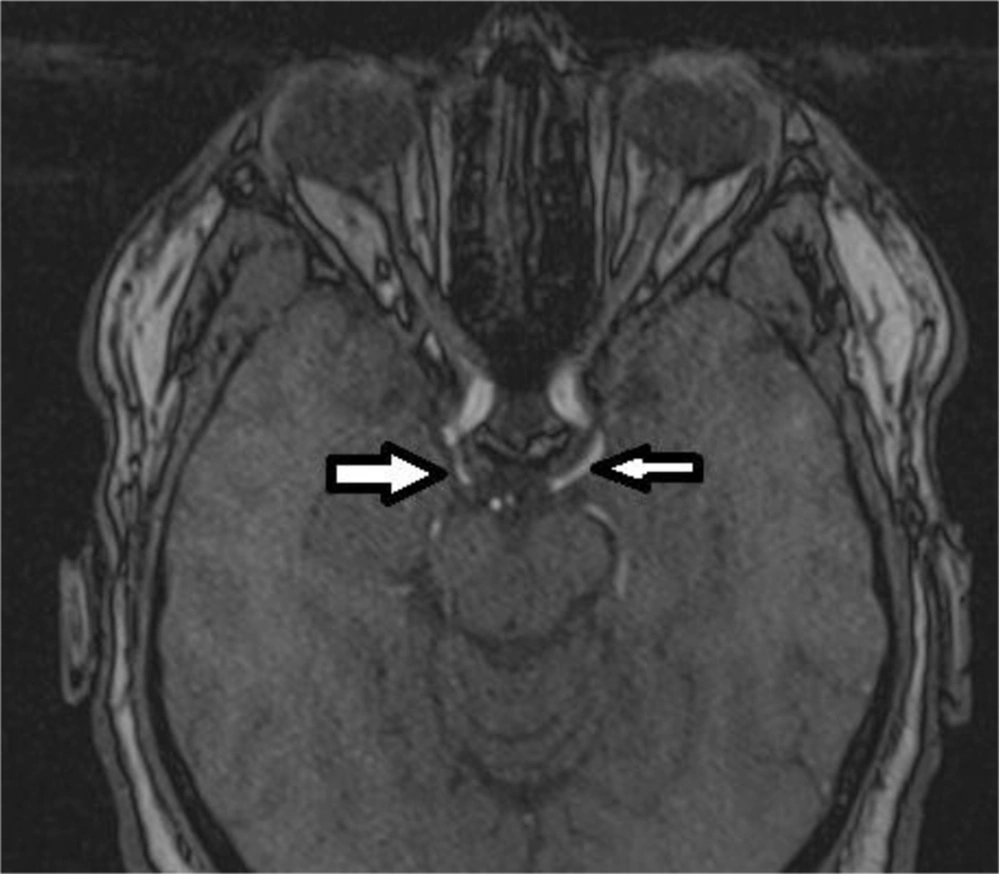
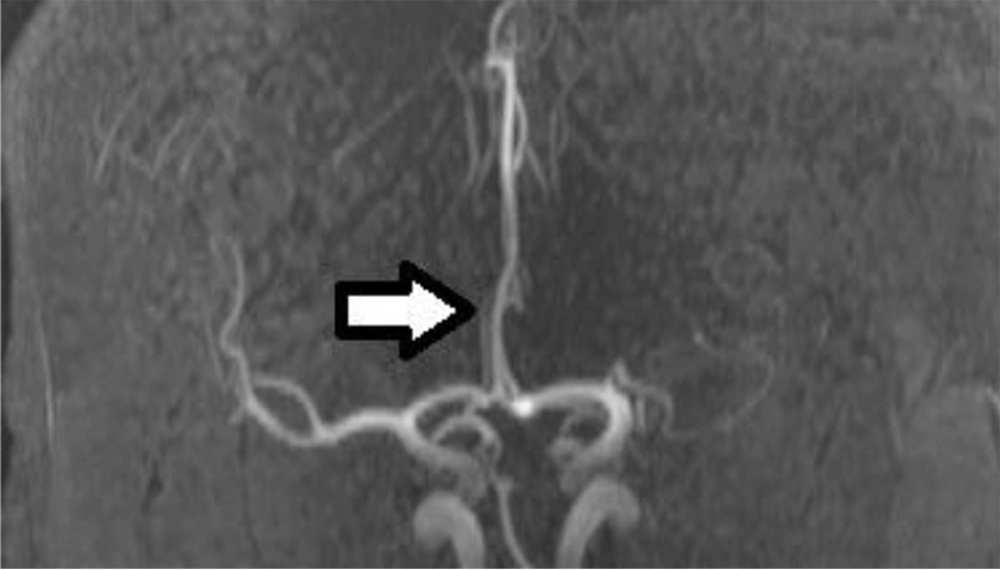
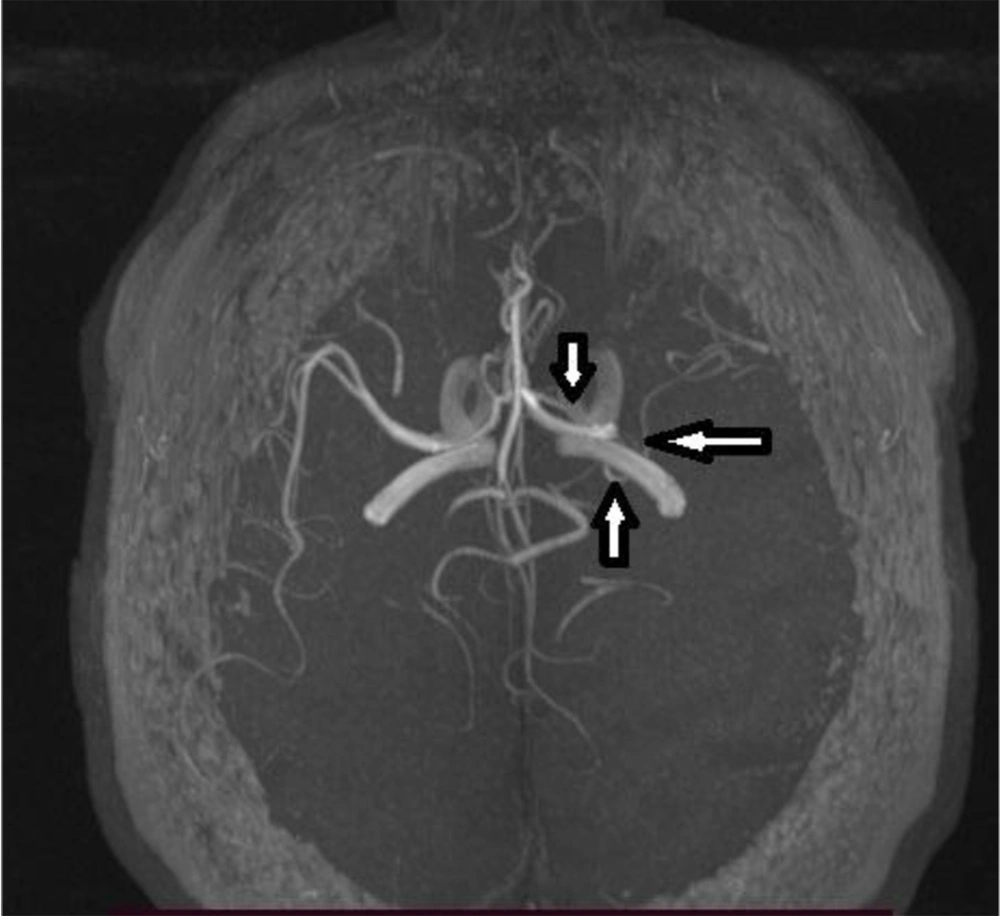
The patient was further evaluated with brain magnetic resonance imaging (MRI) (4). The patient underwent MRI and MRA using the 3D time of flow (TOF) technique with MAGNETOM Avanto (SIEMENS), and the images were processed using the maximum intensity projection (MIP) protocols with a TR and TE of 32 ms and 7.5 ms, respectively. Images revealed variation in CoW, including left Middle cerebral artery (MCA) originating from the distal segment of the A1 segment and triple A2 segment (Figures 1-5). The images also showed persistent fetal circulation via bilateral PCoA, (Figure 3) along with the presence of median callosal artery and triple ACA (Figures 2-4). The patient was observed for 48 hours and, after resolving the symptoms, discharged with aspirin and captopril. Written consent was obtained prior to the study.
3. Discussion
TIA is a predisposing factor for stroke. Patients experiencing TIA are at a higher risk for ischemic stroke, especially within 48 hours (4). CoW supplies the brain with blood and collateral blood vessels. Variations in CoW are common among the population (5), and embryonic hemodynamic changes are believed to play a role in its formation (3). Completeness of CoW is present in 80% and 20% of anterior and posterior parts, respectively (3). Anatomic variations of CoW, including agenesis, hypoplasia, or presence of arteries, in some cases, are described and categorized by Alahmari (6). Some variations in the anatomy of CoW predispose patients to a higher risk of neurovascular accidents, including TIA and stroke (3). Studies also support the role of CoW variation in migraine headaches both in anterior and posterior CoW variations (7). In this patient, exacerbation of headaches can be attributed to CoW anatomic variations, which presented with headaches.
3.1. Conclusions
Headaches can be the first presentation of CoW variation. Physicians should consider this diagnosis in patients with persistent headaches.