1. Introduction
The coronavirus disease (COVID-19) was initially declared in December 2019 in Wuhan, China (1, 2). The global spread of the disease prompted the World Health Organization (WHO) to declare this a public health emergency and international concern on January 30, 2019, and introduce a pandemic on March 12, 2020 (3). The most frequent symptoms of COVID-19 include fever, cough, and shortness of breath (4). Other possible symptoms are abdominal pain, myalgia, diarrhea, sore throat, fatigue, and loss of smell (5). The physiopathology of the disease is still unclear (6). The most common clinical symptoms of the disease are fever (84.5-92.9%), dry cough (40.8 - 74.4%), breathlessness (10.9 - 80.4%), dizziness, anorexia, and myalgia (7). Most of the reported laboratory changes due to COVID - 19 mentioned in previous studies include hypoalbuminemia (30.5 - 100%), increased C - reactive protein (CRP) (21.8 - 94.7%), increased lactate dehydrogenase (38 - 76%), lymphopenia (18.9 - 67.3%), and high erythrocyte sedimentation rate (0 - 92.8%) (4). Aggravating factors that can be fatal manifest themselves through complications, such as severe pneumonia, pulmonary edema (8), pneumothorax, hydropneumothorax, hemopneumothorax (9), pneumomediastinum, subcutaneous emphysema (10), pneumopericardium (11), and acute respiratory syndrome or multiple organ failure (4). Hemopneumothorax occurs spontaneously as an unusual complication of COVID-19 pneumonia (9). Pulmonary infection with COVID-19, and pre-existing lung diseases, can be a secondary cause of spontaneous pneumothorax in patients. Secondary spontaneous pneumothorax also occurs as a complication of an earlier disease, such as pneumonia, huge emphysema, cystic fibrosis, lung cancer, asthma, chronic obstructive pulmonary disease, and lymphangiomyomatosis, or spontaneous esophageal rupture (12). Spontaneous pneumothorax is rare in patients infected with COVID-19 and has been described in several reports (5, 13), and a retrospective study also showed that the incidence of hemopneumothorax is only one percent (8). Spontaneous hemopneumothorax is a rare disease that can occur while accumulating more than 400 mL of blood in the pleural cavity (14).
Due to the outbreak of the COVID-19 epidemic and the unknown symptoms and exact complications of this disease on infected patients, this case study was prepared and conducted after obtaining the code of ethics (IR.BUMS.REC.1400.140) from Birjand University of Medical Sciences and obtaining informed consent from the patients.
2. Case Presentation
A 21-year-old man, with no medical or surgical history, with complaints of pain in the left shoulder went to the emergency ward of a hospital in Birjand University of Medical Sciences one day before admission. During two days, he experienced increased pain in his left shoulder, which spread to the neck and low back so that he could not bend forward, and when bending, he suffered from shortness of breath and cough. The patient reported a history of chest trauma and no symptoms such as fever, cough, or gastrointestinal symptoms but had a history of smoking. His vital signs upon arrival included RR = 20, SPO2 = 98%, PR = 80, and BP = 148.95. The patient was examined by a physician and requested a chest X-ray (CXR) blood test (Table 1); an electrocardiogram (ECG) was taken, and he was admitted with a diagnosis of pneumothorax (Figure 1). According to the physician’s instructions, oxygen was fixed for the patient at 5 liters per minute through a nasal catheter. A chest tube No. 32 was inserted for the patient under local anesthesia from the fourth left-side inter-rib space and connected to the chest bottle in the emergency ward. The patient was advised to have a semi-sitting position, and CXR was performed for him. The patient was then transferred to the surgical ward. The initial discharge was 700 cc; the day after hospitalization, about 1400 cc of blood serum was drained from the patient’s thorax, and the outcome of the PCR test was positive. After worsening the symptoms of shortness of breath and shoulder pain on the second day of hospitalization, the treating physician requested a contrast-enhanced thoracic spiral computed tomography (CT), which was performed on the patient. On the patient’s CT, it was reported that the patient’s lung was completely expanded, and a small clot was evident at the lung base. Then, for two days, the Reteplase drug was injected four times by the treating physician into the patient’s chest tube, and then the chest tube was clamped for 1 hour, and the chest bottle was connected to the suction. After Reteplase was given, the treating physician requested a CXR from the patient; 4 days after implantation, the patient’s chest tube was removed, the CXR was normal, and there was no evidence of hemopneumothorax (Figure 2). After seven days of hospitalization, the patient was authorized to leave the hospital and was taught the steps of home quarantine.
| Mix | Lymph | Neut | TROPONIN | Platet | HCT | HG | RBC | WBC | PCR |
|---|---|---|---|---|---|---|---|---|---|
| 12.5% | 39.5% | 47.9% | Negative | 278 | 44.9 | 15.4 | 5.24 | 5.5 | Positive |
Laboratory Results
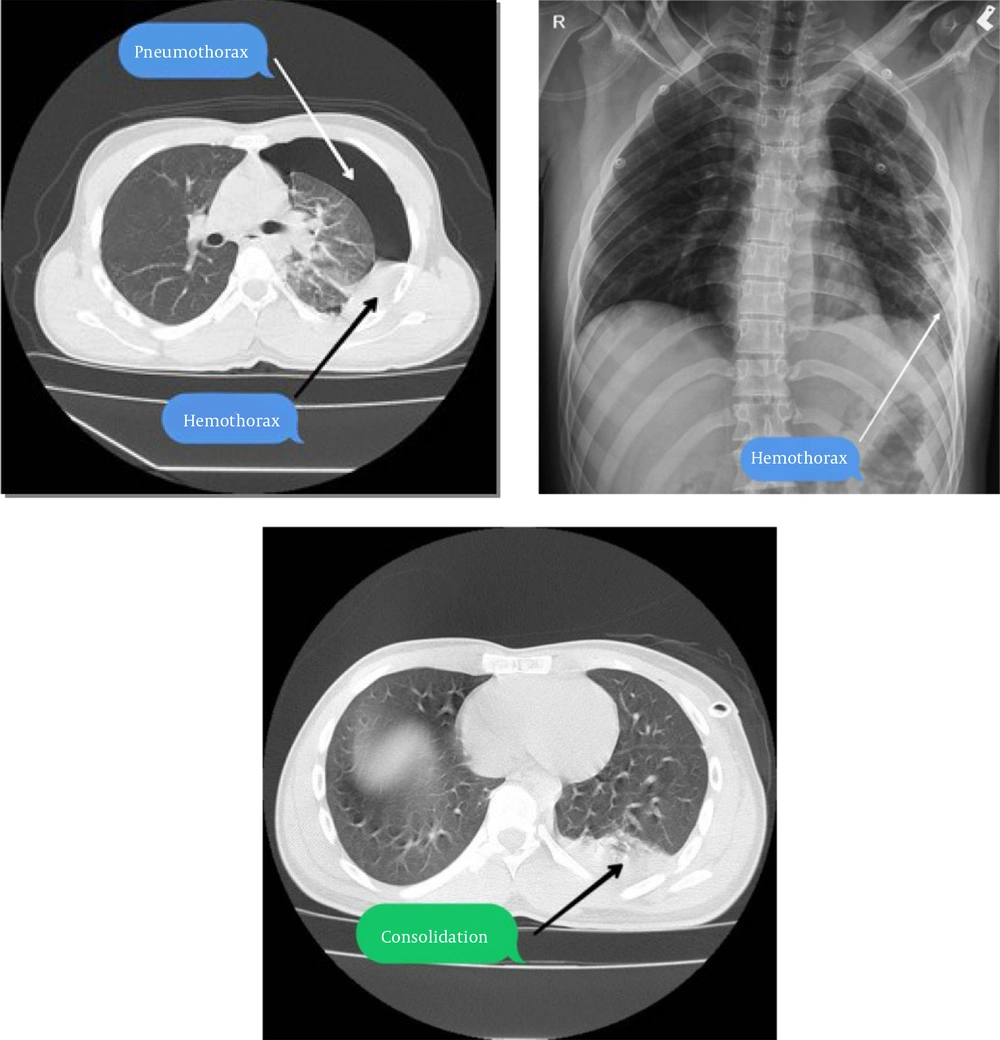
These images are related to performing diagnostic graphs before treatment to diagnose the patient with hemopneumothorax.
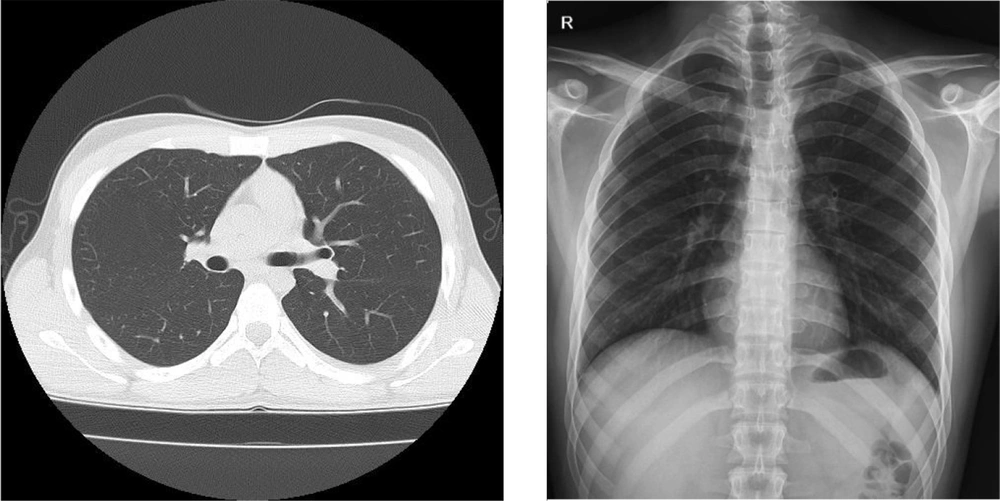
These images are related to performing diagnostic graphs after treatment procedures to diagnose the improvement of hemopneumothorax in the patient.
3. Discussion
COVID-19 is primarily transmitted by close contact with tiny droplets (5). The latent time of this disease is an average of four days (15). In most cases, benign symptoms occur, and in some cases, viral pneumonia and multiple-organ failure (5). The virus has been reported to reach cells via the ACE2 receptor, most of which is found in pulmonary type II alveolar cells. Thus, the lungs are the most vulnerable organ to COVID-19 (16).
Spontaneous pneumothorax is a rare clinical disorder, and 2 to 7.3% of patients with this disease develop hemopneumothorax. Most men afflicted with the disease are between the ages of 15 and 39. The mechanism of this disease consists of bleeding, rupture of adhesions between the parietal and visceral pleura, rupture of the vascular blisters, and rupture of congenital arterial malformation (17). Chen et al. reported that about 1% of individuals with COVID-19 developed a pneumothorax (8). A case report showed that most patients suffering from hemopneumothorax were elderly and had an underlying disease (12). Ozdemir et al. reported that the effects of age and diseases associated with pneumothorax in their study on intubated patients with COVID-19 were not significant (18). However, in our case and the case reported by Sayan et al., there were no underlying diseases prior to COVID-19 (12). A study in the United States also showed that most individuals with hemopneumothorax due to COVID-19 infection had a mean age of 60 years, and most of the samples had an underlying disease (19). In hemodynamically stable patients, tubal thoracostomy therapy is practiced in most cases (20, 21). However, in patients with persistent bleeding and who are hemodynamically unstable, video-assisted thoracoscopic surgery (VATS) or a thoracotomy is performed to control bleeding (22). In addition, in COVID-19 patients, chest CT is recommended for suspected patients with early diagnosis and follow-up (23). In the case mentioned in our study, similar to that reported in Sayan’s study, no particular cause was found for hemopneumothorax. In addition, nothing was detected in terms of anticoagulant consumption and invasive intervention. In the investigation conducted by Yang and Jung, the procedure of bubble creation, the appearance of pneumothorax, and how angiogenesis was provoked in the parietal pleura have been explained. Furthermore, it described that the bubble ruptures act as a detachment force that hurts the adjacent vascular formation and leads to spontaneous hemopneumothorax (24).
3.1. Conclusions
Spontaneous hemopneumothorax pathophysiology was not known in this case report, possibly due to being like the procedure illuminated by Yang and Jung. Also, it can be related to vascular damage resulting from COVID-19 pneumonia. While this is a rare example, it highlights a potentially life-threatening complication on top of the overall adverse respiratory effects of COVID-19. As thromboembolic events are more common in patients with COVID-19, choosing an anticoagulant strategy along with spontaneous bleeding is a challenging dilemma, and further research on coagulation and COVID-19 pneumonia will also be helpful in this regard.