1. Background
Breast cancer is the most common cancer and one of the leading causes of death among women worldwide. About 2.3 million new breast cancer cases were identified in women worldwide in 2020 (1). Breast cancer is the most common cancer in Iranian women, and its incidence has doubled from 2003 (15.96 per 100,000) to 2015 (32.63 per 100,000) (2).
Body image alteration is an important psychosocial concern during breast cancer treatment (3). Changes in the appearance and function of the body following cancer treatment cause negative perceptions, thoughts, attitudes, and feelings toward the body (4). Among the types of cancers, women with breast cancer (BC) experience the most body image alteration (5). Loss of body integrity due to mastectomy, chemotherapy-induced alopecia, difficulty in performing sexual, maternal, and housekeeping roles following lymphedema, fatigue, and other side effects of chemotherapy, hormonal and menopausal change, and negative impact on body image in women with BC. The women with BC use a variety of strategies such as information seeking, self-care, psychological empowerment, improved physical appearance, and maintaining feminine roles for coping with body image alteration (6). However, a wide range of factors affects coping with body image, including individual, therapeutic, and social factors (7). How to deal with past life crises, patterns of interaction with the spouse, family, community, self-help groups, and health professionals impact coping with body image altered (8).
Effective coping with body image promotes quality of life (9) and leads to cancer adaptation (10). Thus, one way of improving the quality of life and breast cancer adaptation is to facilitate coping with the body image altered (11). The facilitator factors for coping with altered body image in women with BC are not well understood. Research with a qualitative approach help to understand the experiences of women with BC. Because of the deep and comprehensive understanding of the unknown domains of phenomena is the mission of qualitative research (12).
2. Objectives
This study aimed to explore facilitating factors and barriers to coping with body image alteration in women with breast cancer. Understanding these factors can help design evidence-based and cultural care to promote coping with body image altered in women with breast cancer.
3. Methods
3.1. Study Design
A qualitative content analysis design was conducted. Data were collected through in-depth semi-structured interviews from March 2016 to October 2017.
3.2. Participants and Sampling Strategies
The participants were 36 women with BC who were purposively selected from healthcare centers in Karaj, Iran. The following selection criteria were used: (1) confirmed diagnosis of breast cancer; (2) 18 years of age and older; (3) interest in sharing experiences and ability to understand and speak Persian; (4) able to complete written informed consent. Sampling was based on the maximum variant approach and continued until data saturation was reached when no new categories or subcategories emerged.
3.3. Data Collection
Face-to-face semi-structured interviews (N-46) were conducted with 36 participants by one author in a private placement of the participants’ choice (e.g., participant home, private room in chemotherapy). The interview began with an open-ended question asking how their bodies changed during cancer treatment. Respondents were then asked how they cope with body image altered. The interviewer then asked more specific probing questions about the facilitators and barriers to coping with body image alteration. See Box 1 for more details about the interview topics.
| Questions |
|---|
| What changes in your body's appearance and function have occurred during treatment? |
| How did you cope with these body changes? |
| What helped you to better cope with changes in your body's appearance and function? |
| How? In what way? Give an example to better understand. What challenges and barriers did you face? Please explain more. |
The duration of interviews took approximately 50 min (ranging from 30 to 120 min). Data collection was discontinued after 43 interviews, as no new data and theoretical saturation of themes had been achieved. Three interviews were conducted to confirm saturation, and no additional codes were identified. All interviews were audiotaped and transcribed verbatim.
3.4. Data Analysis
Each interview was coded and analyzed concurrently with data collection before the next interview. Transcript data were analyzed using the conventional content analysis approach formulated by Graneheim & Lundman (13). The identification number was assigned to each participant. The tape-recorded interviews were transcribed verbatim. Statements from all participants were included in the analysis. The analysis started by identifying the units of meaning extracted from the words and statements. The initial codes with similar meanings were clustered into categories. An example of the theme coding process is shown in Box 1.
| Variables | Values |
|---|---|
| Age (y) | 41.69 ± 8.86 (24 - 64) |
| Marital status | |
| Single | 4 |
| Married | 25 |
| Divorced | 5 |
| Widow | 2 |
| Educational level | |
| Below diploma | 3 |
| Diploma | 13 |
| Bachelor degree | 11 |
| Master degree | 6 |
| PhD | 3 |
| Current occupational status | |
| Employed full-time | 8 |
| Employed part-time | 4 |
| Unemployed due to illness | 8 |
| Retired | 2 |
| Housewife | 14 |
| Number of children | |
| 0 | 6 |
| 1 | 7 |
| 2 | 19 |
| > 2 | 4 |
| Cancer stage | |
| I | 8 |
| II | 14 |
| III | 7 |
| IV | 7 |
| Surgery type | |
| Lumpectomy | 15 |
| Mastectomy | 21 |
| Patient status during the interview | |
| Surgery | 3 |
| Chemotherapy | 6 |
| Radiotherapy | 6 |
| Hormone therapy | 10 |
| Survivor | 11 |
Finally, the main theme of the study generated the coding, and categories were discussed between team researchers until a consensus was reached. Interviewing was stopped when data saturation occurred.
3.5. Rigor
We used criteria by Guba and Lincoln to establish the trustworthiness of the data's credibility, transferability, dependability, and confirmability (14). Prolonged engagement, persistent observation, members, and peer checks helped with data credibility and confirmability. In the data analysis, the involvement of two expert researchers in qualitative research (i.e., the second and the third authors) by reading the transcripts, supervising, evaluating, and confirming the interviews and analysis (coding and categories) enhanced the dependability and confirmability of the data by peer check. Maximum variation sampling increased the transferability, conformability, and credibility of the data of this research. Also, transparency has been ensured by describing every step of the research process. After the data analysis, some participants were contacted and determined whether the codes and themes matched their experiences.
4. Results
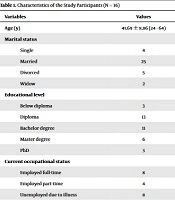
The demographic characteristics of women with BC participating in this study are presented in Table 1.
The present study showed that the facilitators in coping with body image altered in women with BC were "supportive resources" that were extracted from the four subcategories of "receive/understand spouse support," "perceived support by the family," "support for real/online peer group" and "support by non-governmental organizations (NGOs)" (Table 2).
| Main Theme | Categories | Subcategories |
|---|---|---|
| Supportive resources | Receive/understand spouse support | Emotional/psychological spouse support |
| The spouse's effort to maintain a sexual role | ||
| The instrumental support | ||
| Perceived support by the family | Children's emotional/instrumental support | |
| Family emotional/psychological support | ||
| Instrumental family support | ||
| Real/online peer groups support | Receiving emotional/psychological support | |
| Maintaining social interactions | ||
| Using peer experiences for self-care | ||
| Support of non-governmental organizations (NGOs) | Information support | |
| Instrumental support | ||
| Emotional support | ||
| Ineffective support | Failure of the health system to provide services | Lack of insurance support |
| Inappropriate professional interactions | ||
| Lack of informational and emotional support from the health staff | ||
| Unsympathetic interactions | Inappropriate reactions toward the physical and functional changes of the body | |
| Inadequate understanding of the patient's physical condition | ||
| Pity and curiosity about changes in the appearance of the body |
4.1. Receive/Understand Spouse Support
This concept was derived from the emotional/psychological support of the spouse, the spouse's effort to maintain a sexual role, and instrumental support. Married participants identified the spouse as the most important and first source of support for coping with altered body image.
"I would not have been able to continue without my husband's support because I desperately needed support at that time. Spouse support is something else and not comparable to others." [p7]
The experiences of women with BC show empathy and sympathy during mastectomy and hair loss, understanding the patient's psychological condition during treatment, maintaining normal daily interactions despite changes in body appearance, encouraging not to wear scarves, wigs, and breast prosthetics at home to maintain patient comfort, inducing aesthetics and sexual attraction to the patient, focusing on health rather than temporary physical changes, and spouses providing psychological/emotional support.
"My spouse always says you are super beautiful and sexy without hair. My husband only sees my beauty, whatever is my best choice for him. My wife made me believe that I was very beautiful, so I always had confidence. I never thought I'd lose my beauty or my femininity." [p28]
Based on the experiences of the participants, not insisting on sex during chemotherapy, expressing sexual desire and increasing the frequency of sex by the husband to show female sexual attractiveness despite hair and breast loss, flirting to create arousal and sexual desire in women, not insisting on covering the mastectomy site during sex, including the support of husbands to help women maintain their sexual roles. Accepting the responsibility to perform some of the housework and childcare duties has played an important role in maintaining the maternal and housekeeping role of women with BC. Purchasing non-heavy cookware, dishwashing machines, preparing vegetables to prevent lymphedema, providing treatment costs, and accompanying wigs and breast reconstruction were other instrumental supports by spouses.
"My husband wanted to tell me that this illness and appearance deficiency was not a problem for me, with the repeated desire to have sex. This was very effective for me." [p36]
"My husband coordinated his work so that he could go to work later in the morning and give the children breakfast and send them to school. He bought a dishwasher to prevent swelling in my hand. My husband does his homework with the kids once a week so that I don't feel pressured." [p7]
The present study showed that the facilitators in coping with body image altered in women with BC were "supportive resources" that were extracted from the four subcategories of "receive/understand spouse support," "perceived support by the family," "support for real/online peer group" and "support by non-governmental organizations (NGOs)" (Table 2).
4.2. Perceived Support by the Family
Based on the participants' experiences, empathy for family members following the change in body appearance was an important part of perceived emotional support. Family members and children did not react to changes in the appearance of the patient's body and helped in preparing cosmetics, wigs, and breast prostheses to correct the appearance defects and create a sense of belonging, beauty, acceptance, and self-esteem in women with BC. Family supports in housework, and child care played an important role in maintaining women's roles during treatment. Emotional and instrumental support by children was the most important motivating factor for mothers to continue treatment and accept physical changes.
"The day I lost my hair, my father and my niece shaved their hair completely. It was beautiful. It was a feeling of sympathy." [p10]
"My son was a little old, but he was making food, washing all the dishes, and cleaning the house. He was cooking on the balcony so that the smell of food did not make me nauseous. (Silence-crying) He said, "don't use wigs. You are so pretty. We always love you. You are the same mom you were; you made no difference". [p18]
4.3. Real/Online Peer Groups Support
The experiences of the participants showed that joining the group caused an emotional bond between the members and received empathy from their peers. The communication of the group members was similar to that of the family. Participants expressed their feelings in virtual groups at any time and received feedback from members.
For self-care and better management of treatment side effects, they used the experiences of similar patients in the group. Patients' fears and concerns about the treatment's symptoms and side effects were reduced by sharing their common experiences. Familiarity with those survivors and those who had completed their treatment increased hope for recovery, relief from treatment complications, and improved physical appearance. Group prayer strengthened the participants' spiritual dimension and contributed to the patient's psychological empowerment. Interaction with members in virtual or real groups increased their social interactions and reduced the sense of social isolation, and made them feel a sense of belonging to the group. Interaction with the group members was a distraction factor and reduced the side effects of treatment such as pain, insomnia, and nausea. Participating in group parties and group programs with peers provided good opportunities for personal growth and self-esteem by participating in social activities.
"The group played a very positive role for me, both physically and mentally. Each member of the group is like a sister and close to each other." [p4]
"I'm not going out of the house at all (during chemotherapy). I'm always online (with a smile). Although we do not see each other, we laugh, cry, and pray together. On nights when my body ached, I chatted online until morning. When I saw that I was not the only one suffering from this pain and many are like me and having pain at the same time, the pain felt less. I better deal with it. When I send a text that "I have bone pain," I get a lot of good feedback immediately." [p4]
4.4. Support of Non-governmental Organizations
The concept was derived from receiving emotional/psychological support, maintaining social interactions, and using peer experiences for self-care. Based on the experiences of the participants, participating in psychology classes, self-awareness, stress management, life skills, psychological counseling, nutrition counseling, lymph therapy, mental and practical yoga, and the art therapy provided by the support of non-governmental organizations (NGOs) were effective in psychological empowerment, self-care information enhancement, and maintaining feminine roles. Consultation with the patient's spouse and family helped them to accompany and assist the patient in the treatment process. Group programs (yoga, music therapy, art therapy), integrated classes, and services provided by the Institute of NGOs provided opportunities for interaction and emotional-informational support by peers. Trained breast cancer survivors, who were members of the NGOs, would come along with the patients at the first chemotherapy. They provide information and psychological support, prepare patients for changes in appearance, and control treatment side effects. During the course of treatment, they taught patients how to cope with changes in body function and appearance) use of wigs and scarves, breast prostheses and breast reconstruction, makeup, self-care, following a healthy lifestyle, and psychological empowerment. Breast cancer survivors in NGOs, by showing their alopecia due to their chemotherapy and mastectomy, patients were hopeful that the effects of chemotherapy would be transient and that body defects would be repaired by breast reconstruction. Creating a happy environment in chemotherapy wards through positive interactions, sharing sweet memories and music, celebrating the end of treatment, and holding social gatherings at parks, restaurants, and breast cancer conferences were other services provided. From the participants' experiences, the presence of trained breast cancer survivors in NGOs during the initial sessions of chemotherapy was a factor of encouragement and hope for the patients for the possibility of survival and recovery from the disease. They were successful role models for the transition from side effects to treatment, acceptable body appearance, and recovery for patients.
"As I look at myself and my friends, we see how much participation in the classes has made us more experienced in our lives. I had been attending classes for a month, but my husband was saying, "how much you had changed." I had never done anything for myself before, but now I don't neglect anything for myself. Now I'm the most valuable person in this world. For my body, my nutrition, my appearance, and my spirit I do whatever it takes to become better and stay better." [p27]
"When I was in classes with people like me, having or not having a breast would become a joke and have a huge impact on me. As I watched others try to overcome difficulties in order to continue living, my self-esteem increased, and my spirits improved. We became friends through classes and groups, and special energy attracts me to women with breast cancer that won't happen to my other friends. We get energy from each other. We became like a family. When we see each other, the joy and the dance and the music begin." [p31]
The present study showed that the barriers to coping with body image altered were "ineffective support" that was extracted from the two subcategories of "unsympathetic interactions" and "failure of the health system to provide services" (Table 2).
4.5. Failure of the Health System to Provide Services
This category included the subcategories of lack of insurance support, inappropriate professional interactions, and lack of informational and emotional support from the health staff. Based on women's experiences, breast reconstruction after a mastectomy is not a cosmetic procedure but a method to replace and repair body defects. There are different methods of breast reconstruction, and it requires spending a lot of money, which is impossible to pay for everyone. Only a limited number of them are covered by insurance. Each breast reconstruction method is different depending on the patient's condition and the type of surgery performed to treat malignancy, and not all breast reconstruction methods are covered by insurance.
"After the unilateral mastectomy, due to the size of the breast, one side was heavy, and my neck, vertebrae, and back hurt. They gave me a certificate saying that you have to do the reconstruction, but they didn't accept the supplementary insurance and said it was considered cosmetic surgery. Only microsurgical reconstruction and reconstruction with abdominal muscle grafts are covered by insurance. But the prosthesis is not covered by insurance. I can't take a graft from my abdominal tissue; what should I do? The authorities should understand that this is not beauty; this is amputation. I want to take one of my members and put it in its place because it has hurt me so much." [p13]
Inappropriate professional interactions included insufficient emotional support and ineffective communication by health staff. Based on the experiences of the participants, poor communication skills in the form of aggression, neglect, not listening to patients, not answering patient's questions, neglecting emotional and psychological needs, focusing on treatment, and not spending time on education and emotional support caused the patients to feel inferior.
"My wife and I went to the doctor to prescribe Herceptin to me. The doctor laughed at my husband and said, instead of Herceptin, go get another woman with this money. Imagine, I had just had her breast removed, and my chemotherapy and radiation therapy were over; how did I feel when my doctor said such a thing in front of my husband"? [p9]
Inadequate educational services were among the other shortcomings of the health service system. The patients did not consider the training received from the nurse and doctor to take care of themselves, control the side effects of the treatment, prepare to deal with the physical and functional changes of the body, and train their spouses and families to be insufficient.
"When I had a mastectomy, I asked my doctor what to do and what not to do, and he said, lady, go live your normal life. The same things you've been doing. I went home and scrubbed the toilet and bathroom every day, and it caused lymphedema." [p28]
4.6. Unsympathetic Interactions
Based on the participants' experiences, unsympathetic interactions refer to the inappropriate reactions of people, family, spouses, and those around the patient toward the physical and functional changes of the body, such as taunting and verbal and behavioral abuse in relation to changes of the body's appearance and function, inadequate understanding of the patient's physical condition, pity and curiosity about changes in the appearance of the body, such as about the artificiality of hair, eyelashes, eyebrows, and breasts.
"My mother-in-law said my poor son should live with plastic breasts instead of female ones all his life." [p12]
"People approach me for various reasons and look inside the collar of my dress to see if I have breasts or not." [p33]
5. Discussion
In this study, the facilitators in coping with body image altered in women with BC were "supportive resources," which included "receive/understand spouse support," "perceived support by the family," "peer group support" and "support by non-government organizations." Furthermore, the barriers to coping with body image altered were "unsympathetic interactions" and "failure of the health system to provide services."
The present study showed that "supportive resources" facilitated coping with altered body image. This finding was consistent with the results of Hsu et al., who showed that the lack of social support is related to increased body image distress (15). In Price's body image care model, adaptation to the altered body image is affected by the social support network, and a person's body image is the result of the balance between the body image, the environment, and the support network (16). It seems that empowering the support network and facilitating the access of patients to the support network can help patients in coping with their body image altered.
In the present study, the spouse was the most important and first source of support, and the spouse's emotional/psychological, sexual, and instrumental support played an important role in facilitating coping body image in women with BC. This finding was consistent with Brunet and his colleagues (2022) study, which showed that partner support plays a very important role in adapting to the body image altered in women with BC (17). The results of Arikan et al.'s study showed that women who did not have the support of their husbands had a lower body image (18). Spouse emotional support improves women's self-esteem and psychological status (19), and involvement in childcare helps to offset maternal and housekeeping roles (20). Emotional support and intimacy of the spouse endorse the sexual attractiveness and femininity of women (21). Probably because cancer treatments cause disturbances in the appearance of the breast and disturbances in sexual relations due to vaginal dryness and menopause, the type of interaction, companionship, acceptance, and support of the spouse plays an important role in women's adaptation.
The present study was the second most important source of support that facilitated coping with body image altered in women with BC through emotional support, self-care, role maintenance, and psychological empowerment. This finding was consistent with the results of the study by Spatuzzi and his colleagues, which showed that family support has a positive role in improving the body image of women with BC (22). The results of the study by Fang and his colleagues showed that family support accelerates the process of change in the appearance and function of the body until acceptance and normalization (23). It seems that the family's emotional, financial, and instrumental support in helping to play the role of motherhood and housekeeper when treatment complications such as fatigue and lymphedema occur can reduce the feeling of incapacity in performing female roles and help to gradually adapt to physical changes.
In the present study, support from real or virtual peer groups and receiving emotional/psychological information, and instrumental support facilitated coping with body image altered in women with BC. This finding was consistent with the results of the study by Brunet et al. that one of the influencing factors in coping with changing body image was receiving support from other women with cancer in online groups, which provided the opportunity to express concerns, fears and receive support and education (17). Being in a peer group improves body image by expressing emotion, receiving support, learning coping strategies, and improving communication skills (24). It seems that being in online groups and receiving emotional and informational support leads to learning coping strategies for better confronting with body image altered.
In the present study, women's access to non-governmental organizations (NGOs) services through multi-disciplinary team services and psychosocial services played a significant role in coping with altered body image. Several studies showed that coping with body image is affected by access to the support network (16, 17). Non-governmental organizations play a small role in providing medical services, and most of their role is support services such as family care, psychological counseling, and education (25). It seems that access to the support services of non-governmental organizations can help to cope with body image. There is restricted access to the services of non-governmental organizations for all Iranian women with BC. But identification and referral of patients to non-governmental organizations can be part of nurses' duties in body image care, especially for women with inadequate support from family and spouses.
In the present study, the failure of the health system to provide services was one of the barriers to coping with a body image altered in women with BC. This finding was consistent with the results of Shippee et al.'s study, which showed that there is a disparity in the provision of insurance coverage for breast reconstruction (26). The research results of Kim et al. showed that the health staff did not prepare the patients to deal effectively with the physical changes of the body during the treatment process (27). The results of Sodeify et al. showed that Iranian cancer patients and their families complained about the lack of support from their doctors and nurses. But nurses and doctors prioritized the physical support of patients and considered it equivalent to support (28). The results of Majadi Hezaveh & Khademi showed that despite the strong need of patients for emotional support from the medical staff when facing physical changes, proper emotional support was not received from the health staff (29). This finding can be caused by the lack of health personnel and work pressure and the inability of personnel to provide enough time for patients, the lack of a comprehensive model for providing services, and the lack of awareness of medical personnel about supportive educational interventions.
In the present study, unsympathetic interactions were one of the barriers to coping with a body image alteration in women with BC. This finding is consistent with Amini-Tehrani et al.'s study, which showed that stigma is the main source of psychological distress for women with BC, which distorts their body image (30). The study of Harcourt & Frith showed that changes in the body caused the loss of women's privacy and exposed them to the judgment, curiosity, and questioning of strangers about their appearance and body changes. By hiding changes in appearance and avoiding social situations, women keep themselves away from unintentional interaction behaviors, which causes the loss of social support (31). It seems that many people do not understand the boundary between empathic and non-empathic interactions in dealing with women with BC, with apparent changes that this defect in establishing communication skills leads to disrupting the process of coping with the body image in women with cancer.
Despite adequate sample size due to data saturation, the results from this research cannot be generalized to all breast cancer patients due to the small sample size and purposive sampling. The results of the present study explain that supportive resources were the main facilitator for coping with body image alteration in women with BC. However, it does not determine its effectiveness. Therefore, more studies are needed to assess the effect of supportive resources on coping with body image alteration in women with BC.
5.1. Conclusions
This study provided insights into the facilitators and barriers of coping with body image altered in women with BC. Identification of supportive needs related to body image and facilitating access to supportive resources, teaching communication skills and empathy for women with breast cancer, and promoting health services should be addressed in breast-cancer rehabilitation programs. The present findings can be used in designing integrated care models, designing and developing supportive guidelines, and health care policy in the field of breast cancer.