1. Context
Coronavirus Disease-19 (COVID-19) is caused by the severe acute respiratory syndrome Coronavirus 2 (SARS-CoV-2). COVID-19 pandemic has affected nearly 600 million people globally and resulted in more than 6.4 million deaths (https://covid19.who.int/). Nearly 50% of reported COVID-19 cases among young children are infants. Although COVID-19 is not severe in most newborns and infants, less than 10% of the infected infants may suffer severe disease or even die (1). The current scientific evidence has indicated that SARS-CoV-2 can be transmitted through aspiration or close contact with respiratory secretions of the infected individuals, especially those with sneeze or cough (2). Intrauterine, intrapartum, and peripartum SARS-CoV-2 transmission have also been investigated due to their crucial role in maternal and child health (3, 4).
The healthcare-related knowledge required to combat COVID-19 pandemic has increased on a daily basis (5). Breastfeeding and caring for babies are delicate topics that women with suspected or confirmed SARS-CoV-2 infection deal with (6). Breastmilk is a crucial substance for infant feeding that influences both the growth and development of an infant as well as prevents diseases during the lifetime (7). Immunoglobulins against SARS-CoV-2 have been detected in breastmilk of infected mothers. This finding may explain the reduced clinical impact of future exposures to COVID-19 among breastfed infants (8). To date, there is limited evidence regarding the transmission of SARS-CoV-2 through breastmilk. Breastfeeding has generally been accepted as desirable nutrition for infants of infected mothers. Nevertheless, cases of virus transmission from mother to infant through breastmilk have been reported (6, 8).
Although the virus behavior among pregnant women has been widely studied recently, the impact of COVID-19 on the newborn is still not completely understood. Therefore, further studies are needed to better understand this phenomenon (9).
2. Objectives
This study aimed to review the findings of recent studies regarding SARS-CoV-2 transmission from mother to infant during breastfeeding.
3. Methods
In this systematic review, all articles published from December 2019 to December 2021 and available in domestic databases, including IranMedex, SID, IranDoc, Magiran, and Iranian Registry of Clinical Trials (IRCT), as well as in international databases including PubMed, ProQuest, Scopus, Science Direct, Medline, World Health Organization (WHO) publications, and Google Scholar search engine were retrieved.
3.1. PICO Features
The problem, intervention/exposure, comparison, outcome (PICO) strategy was used to define search terms in this review. The population was pregnant women with live birth during the COVID-19 pandemic, exposure was COVID-19, comparison was uninfected pregnant mothers who had given birth to a live infant, and the outcome was COVID-19 transmission from mother to infant through breast milk.
3.2. Search Strategy
The Persian search keywords were defined based on literature search and the reported keywords of the published articles as well as their synonyms. The final keywords were "breastfeeding", "breast", "vertical transfer", "breast milk", "colostrum", "corona", "COVID-19", and "clinical trial". All possible combinations of these terms were searched in Persian databases.
As for English database search, the Latin form, synonyms, and the Medical Subject Heading (MeSH) were adopted. The search keywords included "Breast milk", "milk", "breast", "Human milk", "Breast Feeding", "Lactation", "COVID19 Infection", "COVID19 Outbreak", COVID19 pneumonia", "Severe acute respiratory Syndrome Coronavirus2", "vertical transmission", "SARS coronavirus", " SARS-COV-2 ", "coronavirus 2019", and with Boolean operators AND/OR.
Both given national and international scientific databases were searched for studies; however no time and language restrictions were introduced when conducting the search. Inclusion criteria were observational studies, including cross-sectional, cohort, case-control, case-reports, and case-series, as well as studies on pregnant COVID-19 women delivered to live infants, which had been published in peer reviewed journals. Letters to editors, commentaries, editorials, and studies with no access to their full text were excluded from our study.
3.3. Article Screening
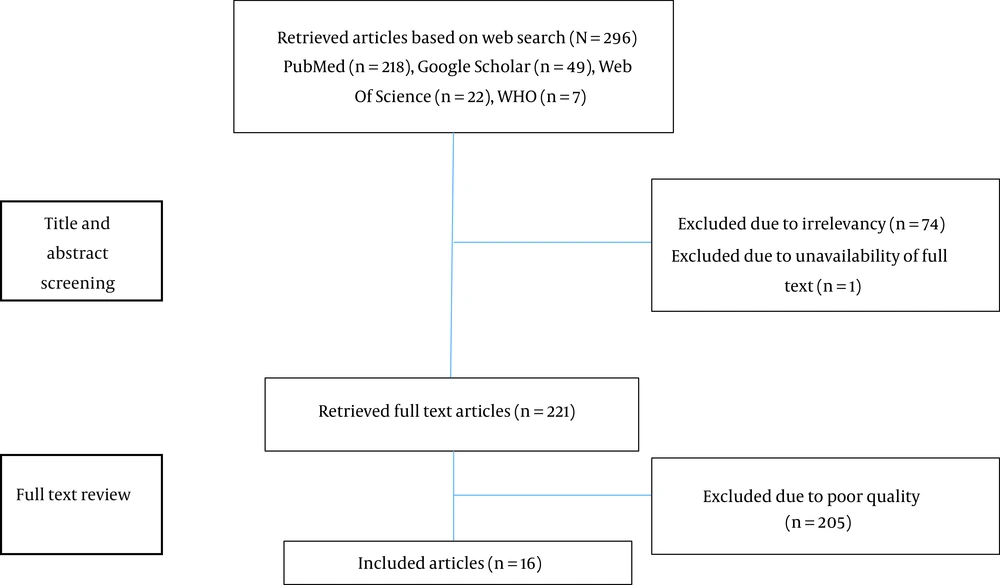
To determine the study objective and analyze the findings, we used the Preferred Reporting Items For Systematic Reviews And Meta-Analysis (PRISMA) checklist. To avoid possible bias, the search was conducted independently by two researchers. The agreement between the researchers was reviewed by a third researcher, and duplicate articles were removed. All studies irrelevant to the topic and identified as duplicated publications, as well as those with insufficient data, were excluded from the study. Then the current systematic review was carried out, and all the screening and search steps were performed and followed by two researchers independently; in case of disagreement, however, a third researcher was requested to join the group discussion in order to resolve it. In the first step, the title and abstracts of the retrieved articles were reviewed, and those articles with relevant titles were recorded. In the second stage, the full texts of articles specified in the previous step were retrieved and evaluated. In this step, the reference list of the reviewed articles was also searched manually in order to add the possible relevant studies that had not been noticed during the initial search. The third stage included evaluating the quality of the studies, when the articles with acceptable quality were selected in order for extracting the required data for the fourth step.
3.4. Data Extraction
Data extraction was performed by all researchers, which involved in checking for author names, publication year, sample size, study type, outcome measures, method for infection detection in both the mother and infant, and main outcomes (infant outcome, COVID-19 test result).
In the first stage, 296 articles were identified based on the search strategy, including 218 articles from PubMed, 49 articles from Google Scholar, 22 articles from Web of Science, and 7 articles from WHO. No unique articles were identified in the other databases. In the second stage, 75 articles were excluded based on the title and abstract. In the third stage, the full text of the remaining 221 articles were reviewed and qualitatively evaluated. Finally, 30 studies with acceptable quality were included in the study. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) checklist for cross-sectional and case control studies was used to evaluate the quality of articles. Out of 30 articles, 14 failed to meet the required quality and were excluded; therefore, only 16 articles were included in the final review. At the end of this stage, the full texts of the articles were reviewed (Figure 1).
4. Results
A total of 16 articles, including four retrospective cross-sectional articles, one cohort study, eight case reports studies, and three eligible case series, were reviewed in this study. General characteristics of eligible articles are listed in Table 1. The presence of SARS-CoV-2 was confirmed by RT-PCR test from the maternal oropharyngeal swab, while milk samples were examined using RT-PCR and considering the existence of serum antibodies (IgG and IgM) against SARS-CoV-2. A total of 208 breastmilk samples and 70 nipple swab samples were examined through providing 237 measurements for RT-PCR and 156 measurements for serum antibodies. Only one cohort study (n = 40) rejected vertical COVID-19 transmission based on negative RT-PCR in all samples (4). The study reported that serum antibodies were transmitted from mother to the newborn in 7.5% (n = 3) of the subjects (4). Among four cross-sectional studies with a total of 152 milk and 70 nipple swab samples, virus transmission was evaluated by RT-PCR and documented in one sample (8.33%), while positive serum antibodies were reported in 24 samples (63.15%) (10-14). Out of 16 milk samples examined in 11 case reports, 6 samples (37.5%) were determined positive by RT-PCR (15-26).
| References/Country | Study Design | Sample Size | Delivery Method | Tests to Assess Mother-to-Child Transmission | Tests Results | Newborn Prognosis |
|---|---|---|---|---|---|---|
| Pace et al., England (10) | Prospective study | 18 mothers | Cesarean section 33% (N = 6) | Milk samples and breast swabs RT-qPCR. Milk samples IgA and IgG antibodies | 100% negative in milk sample; 89% negative; 11% positive in breast swab | Unavailable information |
| Peng et al., China (11) | Cross sectional | 64 mothers; 66 neonates | Cesarean section 65% (N = 42) | Milk samples PCR and IgA and IgG antibodies | 100% negative in PCR; 100% negative for IgG; 55% positive for IgA (N = 21) | 25 neonates positive and 19 neonate suspects |
| Thanigainathan et al., India (12) | Cross sectional | 30 mothers unavailable information about number of neonates | Unavailable information | Milk samples RT-qPCR neonatal oropharyngeal swabs RT-qPCR | 100% negative in milk samples; 100% negative neonatal oropharyngeal swabs | All negative |
| Gao et al., China (13) | Ambispective | 14 mothers; 14 neonates | 85.7% caesarian section (N = 12) | Neonatal nasopharyngeal and oropharyngeal swab, vaginal secretion, breastmilk and stools RT-PCR IgG and IgM antibodies | All PCR tests were negative. 80% of neonatal serum IgG positive (N = 4), 40% of neonatal serum IgM positive (n = 2), and 2 mothers had positive breastmilk IgM | Discharge |
| Sinaci et al., Turkey (14) | Cross‐sectional | 48 mothers; 49 neonates | 79.1% caesarian sections (N = 38) | Placental, umbilical cord, vaginal secretion, and amniotic fluid samples and neonatal nasopharyngeal and oropharyngeal swabs RT-PCR IgM and IgG antibodies | 1 infant had positive RT-PCR. 2 infants have positive IgG, IgM. Only one placental sample and two of the vaginal secretion samples were positive. | One of 49 was hospitalized |
| Krogstad et al., United States (3) | Cohort | 110 mothers | Unavailable information | Breastmilk samples RT-PCR Culture | 7 mothers had positive RT-PCR | Unavailable information |
| Bäuerl et al., Spain (15) | Prospective study | 60 infected mothers; 13 prepandemic control | 76% vaginal section (N = 42) from infected mother 61.5% vaginal section (N = 8) form control group | Breastmilk RT-PCR and IgA, IgM, and IgG antibodies | All negative for RT-PCR. In general, 82.9 % of the milk samples were positive for at least one of the three antibody isotypes | Unavailable information |
| Hinojosa-Velasco et al., Mexico (16) | Case report | 1 mother;1 neonate | Caesarian section | Neonatal nasopharyngeal and oropharyngeal swab, stools, breastmilk sample, mother stool RT-PCR | First tests were positive, then they got negative | Hospitalized |
| Lugli et al., Italy (17) | Case report | 1 mother;1 neonate | Caesarian section | Neonatal Nasopharyngeal swab, stools, and breastmilk sample, RT-PCR Neonate IgG and IgM antibodies | Neonatal tests were 100% negative Breastmilk were 100% positive IgG and IgM were negative | Discharge |
| Gross et al., Germany (18) | Case report | 2 mothers; 2 neonates | Caesarian section | Neonatal oropharyngeal, nasopharyngeal swabs, and breastmilk sample RT-qPCR | 36% breastmilk samples positive; 60 neonates positive | All neonates were positive |
| Liu et al., China (19) | Case repoet | 1 mother; 1 neonate | Vaginal section | Neonate throat and anal swab RT-PCR | All negative | Discharge |
| Costa et al., Italy (20) | Case report | 2 mothers; 2 neonates | 2 caesarian sections | Amniotic fluid, cord blood, placental tissue, neonatal throat swab, and breastmilk samples RT-PCR | 77% negative RT-PCR tests | Discharge |
| Alzamora et al., Peru (21) | Case report | 1 mothers; 1 neonates | Caesarian section | neonatal nasopharyngeal swab RT-PCR IgG and IgM antibodies | 100% positive RT-PCR tests; 100% negative in IgG and IgM | Hospitalized |
| Peng et al., China (22) | Case report | 1 mother;1 neonate | Caesarian sections | Mother amniotic fluid, vaginal secretions, cord blood, placenta, serum, breast milk and Neonatal throat swab, anal swab, serum RT-PCR | All negative | Discharge |
| Phadke et al., India (23) | Case report | 1 mother; 1 neonate | Caesarian sections | Neonatal pharyngeal swab RT-PCR | Positive | Hospitalized |
| Tam et al., Australia (24) | Case report | 1 mother; 1 neonate | Unavailable information | Mother and neonatal nasopharyngeal and stools RT-PCR Breastmilk RT-PCR | Hospitalized | |
| Tang et al., China (25) | Case report | 2 mothers; 2 neonates | 1 caesarian section 1 vaginal section | Neonatal throat and anal swabs RT-PCR IgG and IgM serum | 100% negative infants PCR tests Positive serum IgG | Discharge |
| Wang et al., China (26) | Case report | 1 mother; 1 neonate | Caesarian sections | Placental, cord blood, breastmilk samples and neonatal pharyngeal and anal swab RT-PCR | First pharyngeal swab was positive, and others were negative | Hospitalized |
| Wu et al., China (27) | Case series | 13 mothers; 5 neonates | 4 caesarian sections; 1 natural | Vaginal secretions, stool specimens and breast milk from mother and neonatal throatand anal swabs RT-PCR | All negative except one breastmilk sample | Discharge |
This study mainly aimed to investigate the transmission of coronavirus through breastfeeding in COVID-19 positive mothers. To this end, 16 eligible studies were reviewed. Evaluations of SARS-COV-2 transmission was conducted by performing RT-PCR and obtaining serum antibodies (IgM and IgG) from breast milk samples and nipple swabs. In the study by Pace et al. (10), nipple swabs were analyzed using RT-PCR before and after breast washing. The presence of SARS-RNA before washing was documented by examining eight swabs from the nipple, and a positive sample was also provided. In this study, breastfeeding was recommended after performing nipple lavage.
Pace et al. examined 18 mothers with COVID-19 with a mean age of 34.2 ± 4.7 years. Thirty-seven milk samples and 70 breast swab samples were collected from infected mothers. All swabs and breast milk samples were tested for virus RNA (based on RT-qPCR), while breast milk samples were tested for the presence and quantity of IgG and IgA against nucleocapsid protein, receptor binding domain (RBD), and S2 subunit of SARS-CoV-2 spike protein of SARS-CoV-2. All breast milk samples were found negative based on the RT-qPCR test, although 8 out of 70 maternal breast swabs were labeled positive based on RT-qPCR. All milk contained IgA and IgG specific for SARS-CoV-2, and milk produced by infected mothers was recognized as a source of anti-SARS-CoV-2 IgA and IgG capable of neutralizing SARS-CoV-2 activity. The results from this study were supported maternal lactation during mild to moderate Covid-19 disease (10).
In the study by Peng et al., three groups of lactating mothers, including infected group (24 mothers and 25 infants), the suspected group (19 mothers and 19 infants), and uninfected group (21 mothers and 22 infants) were evaluated. A total of 44 breast milk samples were collected from 16 mothers out of 24 documented COVID-19 infected mothers at ten different time points. Samples were tested for SARS-CoV-2 nucleic acid and antibodies (IgM and IgG). All 44 milk samples were determined as negative ones based on PCR test. Antibody testing was performed to examine 38 samples from 15 infected mothers, all of which were negative for IgG, while 21 samples from 11 mothers were positive for IgA. The authors recommended breastfeeding along with using appropriate hand hygiene precautions and wearing facial masks for all pregnant women (11).
In a study by Thanigainathan et al., 30 COVID-19 mothers diagnosed based on throat swab test and having given birth to live infants and breastfed their neonates were evaluated. Breastmilk samples were collected between 48 and 72 hours after delivery. Oropharyngeal swabs were also obtained from infants on 2nd and 5th days of life and tested using RT-qPCR. All milk samples were negative, except for one sample, which was negative after repeating the test on the next day. All neonatal oropharyngeal specimens were negative and no clinical manifestations of the disease were observed in the neonates (12).
In the study by Gao et al., 14 COVID-19 infected mothers were examined before delivery. Of 14 mothers, 4 mothers agreed to breastfeed their infants. All 4 newborns were tested negative for COVID-19 based on PCR. As for 4 mothers and neonates, IgG and IgM antibodies against COVID-19 were positive in serum and breast milk of one mother, while one mother presented only IgG and IgM in serum, one mother presented only IgG in her serum and breast milk, and another one only presented IgM. Three mothers with positive IgG and IgM in serum and breast milk were found to infect neonates based on the test performed in the first 24 and 72 hours after birth. The second mother was reported to have positive IgG and negative IgM in her serum and milk, and similar results were recorded for her baby. The third mother was only IgM positive and her baby was negative regarding the two parameters. Fourth mother was IgM and IgG positive in serum and IgM negative in breast milk sample. Only IgG was positive in her infant serum (13).
In the study by Sinaci et al., COVID-19 nucleic acid test was conducted on placenta, umbilical cord, vaginal discharge, and amniotic fluid samples from mothers; nasopharyngeal and oropharyngeal swab tests as well as and serum IgG and IgM were also evaluated in their neonates. Only one placental sample and two samples of vaginal discharge were positive for SARSCoV-2. All cord blood and amniotic fluid samples were negative for SARS-CoV-2. Two infants tested positive for COVID-19 IgG and IgM within 24 hours after delivery, but their RT-PCR tests were negative. A positive RT-PCR result was observed in neonates of mothers who were negative for placenta, umbilical cord blood, amniotic fluid, and vaginal discharge (14).
In the study by Krogstad et al., 110 mothers were evaluated, out of who 65 mothers tested positive for COVID-19, 32 ones had symptoms, and 9 ones had COVID-19 symptoms along with negative test. A total of 265 breast milk samples were collected. Virus RNA was found in 7 mothers (7/110). Of these 7 mothers, 6 were positive for COVID-19. No virus was detected in the cultured samples and sgRNA was not detectable in any of the breast milk samples from the 7 mothers (3).
In the study by Bauerl et al., no RNA was found in breast milk of infected mothers (based on RT-PCR), while all the three evaluated antibodies were positive in 52.86% of the mothers and 82.9% of the mothers presented at least one of the three evaluated antibodies in their breast milk (15).
The case reports included overall 15 mothers and their neonates. The results of case report studies are summarized as follows:
Hinojosa-Velasco et al. reported a case of a 21-year-old pregnant mother who had been referred to hospital with COVID-19 symptoms at 37 weeks gestation. The mother had an emergency delivery. The oropharyngeal swap test of the neonate was positive and the neonate presented COVID-19 symptoms. The neonate had not been breastfed during the first 4 days after delivery. Other samples from stool of the neonate as well as stool and breast milk of the mother were taken on day 4, which were positive for virus. On 13th day after delivery nasopharynx, oropharynx and stool examination of the neonate were negative for SARS-CoV-2 (16).
Lugli et al. reported a case of a 33-year-old pregnant woman who had had an emergency delivery at 32 weeks gestation. Two breast milk samples were taken from mother at 3rd (without hygienic persuasions) and 6th day (with mask and gloves) after delivery. Both tests were positive for SARS-CoV-2. The infant was negative for COVID-19 based on the nasopharyngeal swabs and the evaluated IgM and IgG antibodies (17).
Gross et al. reported two cases of pregnant women with COVID-19 who had become symptomatic after delivery. Four breastmilk samples were taken from one mother, which were all negative for SARS-CoV-2, while two out of four breastmilk samples from the other mother were positive for the virus. Three more breastmilk samples were obtained from the second mother, which were negative for the virus. Nasopharyngeal swabs were taken from the neonates indicated positive results in one test for the neonate from the first mother and two positive (second and third swabs) and two negative (first and fourth swab) from the neonate from the second mother (18).
Liu et al. reported a 33-year-old pregnant woman who had breastfed her neonate four days before developing COVID-19 symptoms. Since maternal tests were positive for COVID-19, breastfeeding was stopped. All breastmilk samples from the mother were negative for SARS-CoV-2, and the neonate tests were also tested negative for the disease (19).
Costa et al. reported two pregnant women with COVID-19 symptoms who had positive tests. Amniotic and placental tissue evaluations were positive in only one mother. Six breastmilk samples were taken from both mothers, out of which three were positive in one mother and all were negative in the other mother. Both the neonates were tested negative for SARS-CoV-2 (20).
Alzamora et al. reported a pregnant woman with COVID-19 symptoms who tested positive for the disease in hospital. The delivered neonate was not breastfed and was isolated from the mother. The neonate’s chest X-ray was negative, but its PCR was positive 16 hours after delivery and remained positive till 48 hours after delivery. However, the IgM and IgG antibodies against COVID-19 were negative in the neonate. These findings indicated vertical transmission of the virus (21).
Peng et al. reported a symptomatic pregnant mother woman who was tested positive in hospital based on PCR. The evaluations of amniotic fluid, vaginal discharge, placenta, serum and breast milk of the mother as well as the nasopharyngeal and rectal swab tests of the neonate were negative for SARS-CoV-2 RNA. These findings rejected the hypothesis of vertical transmission of the virus (22).
Phadke et al. reported an asymptomatic pregnant woman whose nasopharyngeal test was positive for COVID-19. Nasopharyngeal swab test of the neonate was positive 48 hours after delivery. No breast milk sample was taken from the mother. These findings rejected the vertical transmission of COVID-19 (23).
Tam et al. reported a pregnant woman who had been admitted to hospital due to positive COVID-19 test result. The neonate became symptomatic one day after delivery. The neonate was breastfed before presenting COVID-19 symptoms. Nasopharyngeal and stool tests were conducted on the neonate after becoming symptomatic. Breastmilk evaluation was positive for virus RNA but the source of neonatal infection could not be determined (24).
Tang et al. reported two pregnant women who had become symptomatic in the second trimester of pregnancy. Their pharyngeal swab tests were negative at the time of delivery. Serum IgG and IgM were positive in one mother, while only IgG was positive in the other mother. Both the neonates were positive for IgG. Breastmilk was not evaluated in this report (25).
Wang et al. reported a COVID-19 pregnant woman delivering a live baby who was tested positive for SARS-CoV-2 based on PCR. Cord blood, placenta, and breastmilk samples were all negative for the virus. Neonatal pharyngeal and rectal swab tests became negative on 15th post-natal day, and the neonate was discharged later (26).
Wu et al. reported 13 COVID-19 mothers, out of who 5 had been infected in the third pregnancy trimester. Breastmilk samples were taken from three mothers on days 1, 6, and 27 after delivery. One neonate was positive for the disease on the first post-natal day, but was tested negative on day 3. All maternal tests, including breast milk samples, and neonatal evaluations were negative for the virus (27).
Overall, the findings of the current review showed that there was only a slight risk of COVID-19 transmission from mother to newborn through breast milk. Taking into account the benefits of breastfeeding, therefore, it was recommended that breastfeeding in symptomatic mothers should not be withheld.
5. Discussion
Due to the lack of effective treatment, the best way to deal with COVID-19 is to avoid infection and prevent its spread through implementing protective measures and personal hygiene (28). COVID-19, declared as pandemic by the World Health Organization (WHO) on March 11, 2020, has continued to spread, unfortunately (29). According to our study findings, no vertical mother-to-fetus transmission was reported, and maternal and neonatal outcomes were favorable in all studies. Furthermore, all amniotic fluid, placenta, breast milk, and vaginal discharge samples were negative for 19-COVID, and no cases of maternal death were reported (30).
Recent studies have found that the main route of SARS-CoV-2 transmission is through inhalation of infected respiratory droplets in close contact with the infected person (i.e., less than 6 steps or less than 2 meters distance) or contact with the patient's secretions (30, 31). Studies on mother-to-fetus transmission during pregnancy have shown that all COVID-19 mothers are able to deliver healthy infants.
The COVID-19 pandemic and the subsequent social distancing have affected the management of breastfeeding and, as the result, direct breastfeeding by COVID-19 mothers has been questioned. Some protocols have suggested separating the infected mother from her baby, while others considered breastfeeding to be safe.
The reviewed study results showed that the breastmilk of mothers with confirmed COVID-19 was negative for SARS-CoV-2 nucleic acid (15-17). According to the CDC report, no SARS-CoV-2 has been found in the breastmilk of mothers with COVID-19; however, antibodies against COVID-19 have been detected in breast milk (18). A previous case report found a newborn with high levels of IgM antibodies against SARS-CoV-2, who was born from a mother with COVID-19.
Separating mother from newborn seems to be the best option in case of severe maternal infection. In such cases, milking should be conducted in order to maintain milk production. Considering the fact that breastfeeding improves the emotional relationship between mother and baby, increases the quality of breastfeeding, reduces maternal stress, and has a proven positive role in the health of mother and baby, it is extremely important to be aware of the effects of COVID-19 pandemics on the ability of infected mothers to breastfeed. Studies have identified numerous barriers to breastfeeding due to the pandemics, which, in some cases, have resulted in the cessation of breastfeeding despite the mother's desire. WHO recommends mother-infant contact and breastfeeding immediately after birth. Despite the fact that many countries follow WHO guidelines, other countries implement infection control and prevention policies by separating mother and baby after delivery as well as by restricting direct breastfeeding or using infected mother’s breast milk for feeding newborns. Based on the data from the studies on COVID-19, it has been determined that the course of the disease in children is mild, although there is a potential for severe disease in infants. It is now a generally-accepted fact that separating mother from newborn causes irreparable damage, including the cessation of breastfeeding, reduced immunity against infectious diseases, and need to use breast milk substitutes. It has also been suggested that mother-newborn isolation does not guarantee the reduction of exposure to the virus during hospitalization and post-discharge. In general, conservative policies negatively affect mothers and their infants and may increase preventable disease rates in infants. According to the reviewed study findings concerning the benefits and disadvantages of breastfeeding, the benefits of breastfeeding outweighed its disadvantages, and therefore, it was recommended that breastfeeding should be practiced after following the health protocols.
According to the CDC, breast milk is the best source of nutrition for the newborn and protects the newborn against many diseases. If the infected mother is in a general, favorable condition and is willing to breastfeed her baby, she may do so after washing her hands with soap and water and wearing a face mask. If the infected mother has severe symptoms and cannot take care of her baby in person, her breast milk can be used for feeding the newborn. In such case, it is recommended that a separate milking device should be used to help mother. Hands should be washed with water and soap for 40 to 60 seconds before and after milking, as well as before contacting the milking pump and milk bottle. All parts of the pump being in contact with breast milk should be washed thoroughly. WHO breastfeeding guidelines released during the COVID-19 pandemic states that breast milk strengthens baby's immune system and protects it against infectious diseases by transmitting antibodies directly from mother to baby. In all cases of confirmed or suspected maternal COVID-19, therefore, mothers are encouraged to breastfeed their babies after following the principles of hygiene and respiratory precautions; they are also advised to wash their hands thoroughly with soap and water or disinfectant solution before and after the contact with the baby and wear a medical mask. In case of severe symptoms, breastfeeding should be continued using pumped milk or donated milk when the mother is not willing to breastfeed her baby (20).
In sum, if the general condition of the infected mother is good and she does not have severe symptoms, breastfeeding should be considered after following health tips and precautions. If the mother is suspected or has COVID-19, she can take care of her baby, and both of them can be placed in the same room. However, it is recommended that the baby should be distanced for at least two meters from mother, and the mother should wash her hands and wear face mask.
COVID-19 management guidelines are constantly modified; however, published studies on breastfeeding women have not reported conclusive results regarding the clinical course, maternal and perinatal outcomes, and the effectiveness of COVID-19 treatments in lactating women. This may have been considered a limitation for our study.
One of the strengths of our study lies in the fact that a comprehensive search was conducted to identify relevant information sources without imposing time limit and reviewing all known factors in previous research, which may have been used in breastfeeding planning for mothers due to the importance of breastfeeding.
One of the limitations of this review was the language barrier. In this review, only published articles in English and Persian medical databases were reviewed. The other limitation of this study was the lack of information about the duration and extent of breastfeeding (i.e., exclusive breastfeeding vs. combined breastmilk and formula feeding) in some studies. Therefore, it was recommended that further studies should be carried out to evaluate the relationship between frequency and duration of breastfeeding and COVID-19 transmission to infants.