1. Background
The coronavirus first appeared in Wuhan, China, in 2019, and it brought many physical, psychological, social, economic, and political problems over the last two years (1). One of the measures to prevent and control COVID-19 was home quarantine, which was associated with many consequences, including increased anxiety and psychological stress (2). Due to the COVID-19 pandemic and nationwide quarantine, many businesses, schools, and universities were closed and continued to operate electronically. This issue posed many problems to many students due to their being far from friends and society. One of the most important problems was COVID-19 anxiety in students (3). These strict restrictions have had many positive and negative consequences. Some positive outcomes was breaking the disease chain among people. However, the main negative consequences were the feelings of loneliness and psychological disorders such as anxiety, depression, and stress (4). Faisal et al. (5) reported 40% anxiety, 72% depression symptoms, and 53% low mental health during COVID-19 pandemic. Landi et al. (6) showed that students with high levels of cognitive flexibility had higher mental health during COVID-19.
Post-traumatic stress disorder (PTSD) is a mental disorder that potentially occurs following an experienced or witnessed event, a threat to his life, or serious injury caused by fear, anxiety, and tension (7). During COVID-19, many people suffered PTSD significantly due to the high spread of the disease, the death of many people, and the fear of disease infection (8). Matalon et al. (9) investigated PTSD, depression, and anxiety in patients with COVID-19 and reported that in the early days of infection with COVID-19, people had high levels of anxiety and depression. In a review study, Cenat et al. (10) reported the prevalence of depression, anxiety, insomnia, PTSD, and psychological distress during COVID-19 to be 97.15, 15.15, 23.87, 21.94, and 13.29%, respectively.
Obsessive-compulsive disorder (OCD) involves a recurring thought or feeling and a conscious behavioral compulsion such as counting, checking, or avoidance, which increases anxiety in individuals (11). Due to the observance of personal hygiene, the observance of home quarantine rules, and the closure of many businesses and universities, it many individuals are expected to be at risk of developing OCD signs and symptoms (12). According to Wheaton et al. (13), OCD symptoms increased in 76.2% of people after COVID-19. Hassoulas et al. (14) showed that people with high levels of OCD and health anxiety experienced COVID-19-related thoughts and behaviors more frequently, which aggravated the symptoms of the disease among these individuals.
Cognitive-behavioral therapy (CBT), one of the most experimental approaches to explaining anxiety disorders, believes that most anxiety symptoms are caused by ineffective beliefs leading to a vicious cycle of stress, discomfort, depression, and fear (15). Liu et al. (16) investigated the effectiveness of ICBT for depression and anxiety in patients with COVID-19. The obtained results showed that the depression and anxiety decreased significantly in the experimental group after receiving ICBT.
2. Objectives
Since the COVID-19 pandemic, many people have been suffering from various psychological problems affecting their performance and social relations. The present study aimed to measure the efficacy of ICBT for mental health, PTSD, and OCD in students with COVID-19 anxiety.
3. Methods
This semi-experimental study was as a pre-/post-test with a control group. The Tarbiat Modares University’s students were used to collect the required data in the academic year 2021. To identify students with COVID-19 anxiety, 30 students were randomly selected from among the students who scored > 28 on the COVID-19 anxiety scale. Then the students were randomly assigned to the experimental (n = 15) and control (n = 15) groups (17). Inclusion criteria were access to the Internet, not suffering from a serious illness, not using psychiatric drugs, and personal satisfaction. Exclusion criteria were failure to answer the questions, aggravated anxiety intensity, and being absence for more than two therapy sessions.
3.1. Coronavirus Anxiety Scale
The Coronavirus Anxiety Scale was developed and standardized in Iran (18). This questionnaire contains 18 questions scored on a Likert scale ranging from never (0) to always (3), with higher scores indicating the individuals’ suffering from COVID-19 anxiety. In the present study, those with scores > 28 were classified as students with COVID-19 anxiety. To check the reliability of the questionnaire, Alipour et al. (18) reported Cronbach's coefficient of 0.91. In this study, Cronbach's alpha coefficient was 0.86.
3.2. Short Form of Mental Health Questionnaire
This questionnaire consists of 14 items scored on a six-point Likert scale ranging from never (1) to every day (6) to measure mental health. Minimum and maximum scores of the questionnaire are 14 and 84, respectively. In Keyes' study (19), the validity and internal consistency of the questionnaire were 0.80, and its Cronbach's alpha was 0.73. In Iran, Bagheri Sheykhangafshe et al. (20) reported the Cronbach's alpha of the mental health questionnaire to be 0.85. Cronbach's alpha was 0.87 in this study.
3.3. Post-Traumatic Stress Questionnaire
This scale investigates PTSD and has 39 items. It is scored on a Likert scale ranging from 1 to 5 for each item. Total scores can range from 39 to 195. Regarding the validity of this questionnaire, its sensitivity coefficient for distinguishing groups with disorders and groups with no disorders was 0.93 (21). In Iran, the validity of the test was confirmed using the internal consistency method and the dichotomization method (0.92), and it was 0.91 in retesting following a one-week interval (22). Researchers in this study also reported Cronbach's alpha coefficient of 0.81 for the whole PTSD scale.
3.4. Obsessive-Compulsive Disorder Questionnaire
The Padova Questionnaire was developed by Sanavio (23) in Italy, which contained 60 items and was used to evaluate the severity of OCD symptoms in clinical and normal participants. Each item was scored from 0 to 4 regarding the degree of disturbance. The Padova questionnaire is a self-report scale differentiating obsessive thoughts from practical obsessions. In the Iranian population, Goodarzi and Firoozabadi (24) calculated Cronbach's alpha coefficient of the obsession scale to be 0.95. In this study, Cronbach's alpha coefficient of 0.86 was reported for the OCD scale.
ICBT protocol: The ICBT of the present study was based on protocols used for health anxiety (25). Before implementing the treatment, the questionnaires were administered to the students as a self-report (pre-test). Then, the experimental group performed the group ICBT via Skype during eight 90-minute sessions for 2 months, with one session per week (Table 1).
| Session | Target | Topic | Homework |
|---|---|---|---|
| 1 | Familiarity with group rules and generalities of ICBT | Introducing and explaining the content of intervention sessions, Challenging anxiety-causing automatic thoughts about COVID-19, and reducing persistence. | Writing a list of negative and ineffective thoughts. |
| 2 | Increasing body awareness | Reducing the exaggeration of physical and psychological symptoms with an emphasis on increasing awareness regarding the symptoms of COVID-19 as well as the symptoms of disease anxiety | Doing sports activities and breathing exercises |
| 3 | Cognitive flexibility about health anxiety | Awareness and education about cognitive errors that increase disease anxiety, encouraging controlled and reasonable attention to physical symptoms. | Facing cognitive errors and evaluating their consequences. |
| 4 | Challenging thoughts and behaviors associated with health anxiety | Providing and teaching alternative explanations for physical symptoms, paying attention to shift training; Reducing excessive checking behavior | Reading some books about anxiety and obsessive thoughts. |
| 5 | Conscious control over the mind and prevention of rumination | Training to have times free of mental rumination about COVID-19 and contracting the disease. | Not following news on COVID-19 pandemic. |
| 6 | Increasing emotion regulation and pain management strategies | Increasing positive evaluation, non-catastrophic beliefs, and less threatening explanations; Mindfulness exercises. | Consciously performing daily activities. |
| 7 | Introducing techniques for calming the mind and soul | Training and reinforcing methods to cope with disease anxiety, relaxation training and practice. | Not paying attention to the disease symptoms and entertaining yourself with other issues |
| 8 | Increasing media literacy and health and preventing extreme search | Reducing excessive search for medical information, reducing false security-seeking behaviors such as visiting doctors several times. | Confirming the test results and the doctor's opinion. |
Abbreviation: ICBT, internet-based cognitive-behavioral therapy.
4. Results
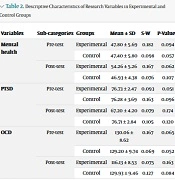
Table 2 presents the mean and standard deviation of pre-test and post-test scores of mental health, PTSD, and OCD in patients with COVID-19 anxiety in the two groups. The Shapiro-Wilks (S-W) normality test results also indicate that the variances in the two groups are normal (Table 2).
| Variables | Sub-categories | Groups | Mean ± SD | S-W | P-Value a |
|---|---|---|---|---|---|
| Mental health | Pre-test | Experimental | 47.80 ± 5.69 | 0.182 | 0.094 |
| Control | 47.40 ± 5.80 | 0.098 | 0.057 | ||
| Post-test | Experimental | 54.26 ± 5.26 | 0.167 | 0.062 | |
| Control | 46.93 ± 4.38 | 0.076 | 0.107 | ||
| PTSD | Pre-test | Experimental | 76.73 ± 2.47 | 0.093 | 0.051 |
| Control | 76.28 ± 3.69 | 0.163 | 0.096 | ||
| Post-test | Experimental | 67.20 ± 4.20 | 0.079 | 0.174 | |
| Control | 76.71 ± 2.84 | 0.105 | 0.120 | ||
| OCD | Pre-test | Experimental | 130.06 ± 8.62 | 0.167 | 0.065 |
| Control | 129.20 ± 9.74 | 0.069 | 0.052 | ||
| Post-test | Experimental | 116.13 ± 8.53 | 0.075 | 0.163 | |
| Control | 129.93 ± 9.46 | 0.127 | 0.084 |
Abbreviations: OCD, obsessive-compulsive disorder; PTSD, post-traumatic stress disorder.
a Shapiro-Wilk test.
The of the Levin test results regarding the homogeneity of variance in dependent variables confirmed homogeneity for mental health (F = 4.07, P = 0.533), PTSD (F = 2.84, P = 1.641), and OCD (F = 1.74, P = 0.596) in the groups. Moreover, other presumptions of the analysis of covariance test, such as Box M (Box M = 8.19, F = 1.20, P = 0.300) and Bartlett's chi-square test, are met for the two groups (χ2 = 29.16, dF = 5, P < 0.05). Accordingly, the multivariate analysis of covariance (MANCOVA) was allowed. Then MANCOVA was run to detect the differences between the groups. The results (Wilks Lambda= 0.255, F = 22.34, P = 0.001, and ETA=0.74) showed the impartial impact of the variable on the dependent variables.
| Variables | SS | DF | MS | F | Effect Value | P-Value |
|---|---|---|---|---|---|---|
| Mental health | 366.961 | 1 | 366.961 | 33.38 | 0.57 | 0.001 |
| PTSD | 733.668 | 1 | 733.668 | 30.43 | 0.55 | 0.001 |
| OCD | 1690.357 | 1 | 1690.357 | 19.11 | 0.43 | 0.001 |
Abbreviations: OCD, obsessive-compulsive disorder; PTSD, post-traumatic stress disorder.
In Table 3, F-statistic is meaningful for mental health (F = 33.38), PTSD (F = 30.43), and OCD (F = 19.11) at P = 0.001. These findings imply a significant difference between the groups in these variables. Moreover, in line with the calculated effect size, 57% of mental health, 55% of PTSD, and 43% of OCD were independent of the effect of the variable, suggesting that ICBT significantly increases mental health and decreases PTSD and OCD in students with COVID-19 anxiety.
5. Discussion
The study aimed to measure the efficacy of ICBT for mental health, PTSD, and OCD in students with COVID-19 anxiety. The findings revealed that ICBT increased students' mental health with COVID-19 anxiety. These findings are in line with previous studies (6-8).
Regarding the decrease in the participants’ mental health following an increase in anxiety, it can be explained that this relationship is a combination of several factors. First, it caused the unknown nature of the disease, the widespread mutation of the virus, quarantine, and its uncertain duration expose individuals to feelings of insecurity about themselves and their surroundings, anxiety, and stress (7). Sine a person’s efforts alone cannot establish this security, and news tell about a new group of infections daily, one can see himself and those surrounding him in constant danger and experience constant failure. This failure can significantly increase the symptoms of anxiety, depression, and stress among individuals (2-4).
The findings showed that ICBT reduced PTSD in students with COVID-19 anxiety. These findings are consistent with previous studies (9, 10). In explaining these findings, it can be acknowledged that during the outbreak of COVID-19, many individuals witnessed the death of their family, friends, and relatives worldwide. Due to the lack of specific treatment, there was a lot of fear and worry about contracting COVID-19, all of which made individuals suffer from remarkable stress (8). During the COVID-19 pandemic, the presence of various factors such as living in quarantine, staying away from the community, closing schools and universities, experiencing death anxiety, having unexpressed mourning, and hearing global death news caused widespread psychological problems (9). If they are not considered in time, we will observe the spread of PTSD in many regions of the world (10). Karatzias et al. (8) investigated the symptoms and severity of PTSD during the COVID-19 pandemic. Their findings confirmed that 17.7% of people had PTSD syndrome, which had a high correlation with anxiety and depression.
Moreover, the findings of this research indicated that ICBT reduced OCD in students suffering from COVID-19 anxiety. These findings are consistent with previous studies (13, 14). Because COVID-19 has symptoms similar to a cold, many people become sensitive to their physical symptoms and constantly check themselves (11). After hearing a variety of news about the number of infected, deaths, and common symptoms of COVID-19, concerns about COVID-19 among people were not far from expectation (12). On the other hand, the World Health Organization (WHO) has provided health recommendations such as wearing masks and gloves, washing hands and face, disinfecting surfaces, maintaining social distancing, and taking vitamins to avoid COVID-19. However, these cases may cause problems for individuals with OCD symptoms or those who are prone to it (13). During the outbreak of COVID-19, many people became sensitive to their physical symptoms, trying to get more information about the new symptoms of COVID-19, the mutations of the virus, and the number of the infected (14).
The statistical population of this research encompassed the students of the Tarbiat Modares University in 2021; hence, there should be caution in generalizing the findings to other groups and regions. Self-reporting and online questionnaires were the limitation of the present study. In this regard, it is suggested to distribute the research questionnaires face-to-face in future studies while observing social distancing and health precautions. On the other hand, according to the long-term consequences of the COVID-19 epidemic on individuals’ psychological health, some measures should be adopted to identify students with COVID-19 anxiety, improve their mental health, and promote their performance.
5.1. Conclusions
ICBT, as an efficient and low-cost treatment, can prevent many psychological and physical outcomes. Since the patient's ineffective beliefs and cognitive dimensions are one of the reasons for the aggravation of the COVID-19 anxiety symptoms, improving their mental health plays a critical role in preventing and controlling the disease. For this purpose, it is necessary to detect high-risk groups and adopt cognitive-behavioral interventions for these patients. Given that during the COVID-19 epidemic, many psychological service centers were closed and did not have the necessary facilities to provide virtual consultations, psychological and treatment centers can now provide the necessary equipment and services to patients who, for different reasons, cannot visit a psychologist or a doctor in person.