1. Background
The outbreak of SARS-CoV-2 rapidly turned into a critical global health issue. In March 2020, the World Health Organization (WHO) proclaimed this situation a pandemic (1), indicating its importance. The COVID-19 outbreak has many side effects on routine human life, such as social withdrawal, financial imbalance, fear, and uncertainty. Besides, the anxiety of being affected by the virus and its related issues, such as stigma and death, has offered too many stressors and stress to the daily life of human beings (2).
Studies on COVID-19 have shown its adverse psychological effects on the general population (3-6). These adverse effects were investigated in many subgroups of society, such as university students (7) and medical health workers (8, 9). These effects varied based on stress, depression, sleep problems, fear, anxiety, post-traumatic stress, burnout, and frustration (10-12). These conditions could interfere with everyday personal and interpersonal relationships and a sense of well-being, leading to dysfunction in different areas of routine activities such as occupation and education (2).
Meanwhile, only a few studies have investigated the psychological status of faculty members of universities during the COVID-19 pandemic, reporting some psychological experiences of this group, such as exhaustion, frustration, depression, post-traumatic stress, anxiety (13, 14), and a decline in the mental health status (15). However, according to some limited studies, the psychological condition of faculty members has not been reported as favorable before the COVID-19 pandemic according to less job satisfaction due to heavy workload, the high number of students, extended working hours, and absence of work-life harmony (15).
On the other hand, resilience refers to the degree of flexibility and ability to adjust to undesirable changes, which can vary during the life course based on one’s psychological characteristics (16). The preventive role of resilience against the formation or aggravation of various psychopathologies was addressed in different scientific lectures (17, 18). Therefore, resilience might be crucial in protecting one’s mental and functional stability against a conflictual and complex situation, such as the COVID-19 outbreak (19).
2. Objectives
Although the psychological state of many subgroups of society has been analyzed in different studies after the COVID-19 outbreak, research on the psychological state of faculty members of medical universities, as part of society responsible for training students in various fields of medical sciences, following the coronavirus pandemic has been somehow neglected. The importance of this issue becomes apparent when we consider the indirect effects of this training on society’s health by educating and graduating medical students. Therefore, this study aimed to assess the psychological status of faculty members of Birjand University of Medical Sciences, Iran, regarding the COVID-19 outbreak, from May 2020 to December 2020.
3. Methods
With the method of convenience sampling, 122 faculty members of Birjand University of Medical Sciences, Iran, from May 2020 to December 2020, completed an online questionnaire containing demographic information along with two standard scales of Depression, Anxiety, and Stress-21 (DASS-21) and Connor-Davidson Resilience Scale-25 (CDRISC-25). The online questionnaire was made at Porsline, and its link was sent to the Birjand University of Medical Sciences faculty members. Demographic information can be seen in Table 1. The inclusion criteria were being a faculty member of Birjand University of Medical Sciences and being willing to complete the electronic questionnaires. Those electronic questionnaires, which were left uncompleted, were excluded.
| Demographic Variables | Frequency (%) |
|---|---|
| Sex | |
| Female | 81 (66.4) |
| Male | 41 (33.6) |
| Marital status | |
| Single | 26 (21.3) |
| Married | 90 (73.8) |
| Divorced | 5 (4.1) |
| Widowed | 1 (0.8) |
| Having a child | |
| Yes | 42 (34.4) |
| No | 80 (65.6) |
| Grade | |
| MA | 34 (27.9) |
| Ph.D. | 35 (28.7) |
| Post-doctorate | 2 (1.6) |
| Specialty | 47 (38.5) |
| Subspecialty | 4 (3.3) |
| Academic rank | |
| Lecturer | 39 (32.0) |
| Assistant professor | 61 (50.0) |
| Associate professor | 17 (13.9) |
| Professor | 5 (4.1) |
| Work experience (y) | |
| < 5 | 52 (42.6) |
| 5 - 10 | 29 (23.8) |
| 10 - 20 | (17.2) |
| > 20 | 22 (16.4) |
| A family member who needs permanent care | |
| Yes | 24 (19.7) |
| No | 98 (80.3) |
| Administrative position | |
| Yes | 61 (50.0) |
| No | 61 (50.0) |
| Consumption of sedative drugs for more than three consecutive months | |
| Yes | 11 (9.0) |
| No | 111 (91.0) |
3.1. Tools
3.1.1. Depression, Anxiety, and Stress Scale-21
Lovibond and Lovibond developed this scale in 1995 to measure post-traumatic stress, anxiety, and depression, which involves 21 items with a Likert scale, from zero (did not apply to me at all.) to 3 (extremely applied to me). The range of scores is 0 - 63 (20). In one study, internal consistency for the total scale of DASS was reported as 0.89. Item-total correlations varied from 0.51 to 0.75. Split-half and test-retest reliability coefficients were reported as 0.96 and 0.99, respectively. The study revealed that DASS is a valid and reliable instrument (21). The translated Persian version of this questionnaire showed satisfactory reliability and validity in target groups (22, 23). The Cronbach’s alpha coefficients of depression, anxiety, and stress in the present study were 0.87, 0.75, and 0.78, respectively.
3.1.2. Connor-Davidson Resilience Scale-25
This scale was developed in 2003 and consisted of 25 items with a Likert scale, from 0 (completely incorrect) to 4 (always correct). The range of scores is 0 - 100. Cronbach’s alpha for the total scale was reported to be 0.89, and item-total correlations varied from 0.30 to 0.70. The test-retest reliability correlation coefficient was 0.87 (24). A higher mean score indicated a higher level of resilience. This questionnaire was translated into Persian, and its reliability coefficient using Cronbach’s alpha was reported to be 0.89 (25). The Cronbach’s alpha of this scale in the present study was 0.90.
3.2. Statistical Analysis
SPSS version 19 was used for statistical analysis. Qualitative variables were presented as percentages. Quantitative variables were presented as mean and standard deviation. The Kolmogorov-Smirnov test was applied to check normal distribution. Independent t-test (Mann-Whitney U test for non-normally distributed data) and analysis of variance (ANOVA) (Kruskal-Wallis test for non-normally distributed data) were used to compare the variables between the groups. Pearson’s correlation coefficient measured the power of the relationship between variables. The P-value below 0.05 was considered statistically significant.
4. Results
This study enrolled 122 faculty members of Birjand University of Medical Sciences. Their mean age was 40.6 ± 8.35 years. Eighty-one (66.4%) participants were women. Ninety (73.8%) participants were married, and 80 (65.6%) participants had children. Regarding education, most participants had Ph.D. degrees (28.7%) or were specialists (38.5%). Ninety-eight (80.3%) participants did not deal with a family member who needed permanent care. Fifty-two (42.6%) participants had less than five years of work experience. Also, 111 (91%) participants had no history of taking sedative drugs (Table 1).
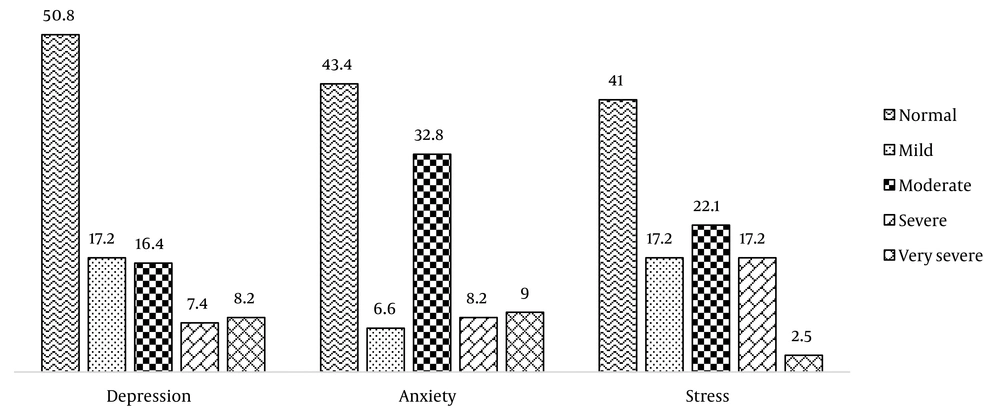
According to Figure 1, during the COVID-19 outbreak, the prevalence of moderate to very severe depression, anxiety, and stress in the target group was 32%, 50%, and 41.8%, respectively. As seen in Table 2, faculty members with administrative positions had significantly higher resilience levels than others (P < 0.001). There was a significant difference between the resilience scores of the participants based on academic rank (P = 0.03); according to Tukey’s Post Hoc test, the difference was between the lecturer and assistant professor ranks. Work experience also had a significant effect on resilience (P = 0.02). People with a history of 5 - 10 years had significantly lower resilience levels than people with a history of 10 - 20. Also, people who did not use sedative drugs revealed more resilience than those who used sedatives (P = 0.03).
| Demographic Variables | Mean ± SD | P-Value |
|---|---|---|
| Resilience | ||
| Administrative position | < 0.001 a | |
| Yes | 72.62 ± 10.41 | |
| No | 65.95 ± 11.18 | |
| Academic rank | 0.03 b | |
| Lecturer | 65.41 ± 9.24 | |
| Assistant professor | 71.30 ± 11.85 | |
| Professor or associate professor | 70.59 ± 11.58 | |
| Work experience | 0.02 b | |
| < 5 | 68.81 ± 11.10 | |
| 5 - 10 | 65.21 ± 12.32 | |
| 10 - 20 | 75.05 ± 10.18 | |
| > 20 | 70.40 ± 8.98 | |
| Taking sedative drugs | 0.03 a | |
| Yes | 62.27 ± 10.05 | |
| No | 69.98 ± 11.18 | |
| Depression | ||
| Marital status | 0.011 c | |
| Single | 14.53 ± 9.74 | |
| Married | 9.70 ± 9.17 | |
| Administrative positions | 0.006 c | |
| Yes | 8.33 ± 7.97 | |
| No | 13.14 ± 10.25 | |
| Education | 0.046 d | |
| MA | 13.94 ± 10.03 | |
| Ph.D. or post-doctorate | 9.56 ± 8.22 | |
| Specialty or subspecialty | 9.45 ± 9.59 | |
| A family member who needs permanent care | 0.047 c | |
| Yes | 15.75 ± 12.87 | |
| No | 9.51 ± 8.04 | |
| Taking sedatives | 0.001 a | |
| Yes | 23.45 ± 13.02 | |
| No | 9.47 ± 8.08 | |
| Anxiety | ||
| Education | 0.009 d | |
| MA | 12.70 ± 7.67 | |
| Ph.D. or post-doctorate | 8.21 ± 5.22 | |
| Specialty or subspecialty | 8.43 ± 6.96 | |
| Stress | ||
| Marital status | 0.036 c | |
| Single | 20.61 ± 7.68 | |
| Married | 16.16 ± 9.04 | |
| Administrative Position | 0.002 c | |
| Yes | 14.59 ± 8.24 | |
| No | 19.63 ± 8.93 | |
| A family member who needs permanent care | 0.013 c | |
| Yes | 21.0 ± 9.95 | |
| No | 16.16 ± 8.44 | |
| Taking sedatives | 0.024 c | |
| Yes | 23.45 ± 10.47 | |
| No | 16.48 ± 8.56 | |
at-test.
b Analysis of variance (ANOVA).
c Mann-Whitney U test.
d Kruskal-Wallis.
The mean score of depression was significantly different between single and married individuals, so single participants had a higher score of depression (P = 0.011). Faculty members with administrative positions revealed lower depression scores than others (P = 0.006). Also, faculty members with master’s degrees showed more depression than specialists and subspecialists (P = 0.046). Also, individuals with a family member who needed permanent care (P = 0.047) and individuals who took sedative drugs (P = 0.001) had significantly higher scores of depression compared to related groups.
The anxiety scores of faculty members with master’s degrees were significantly higher than that of other groups of specialty and subspecialty, Ph.D., and post-doctorate holders (P = 0.009).
In our study, single participants experienced significantly higher stress than married ones (P = 0.036). Participants with administrative positions reported less stress than others (P = 0.002). Also, participants with a family member who needed permanent care (P = 0.013) and sedative drug consumption (P = 0.024) experienced significantly higher stress levels.
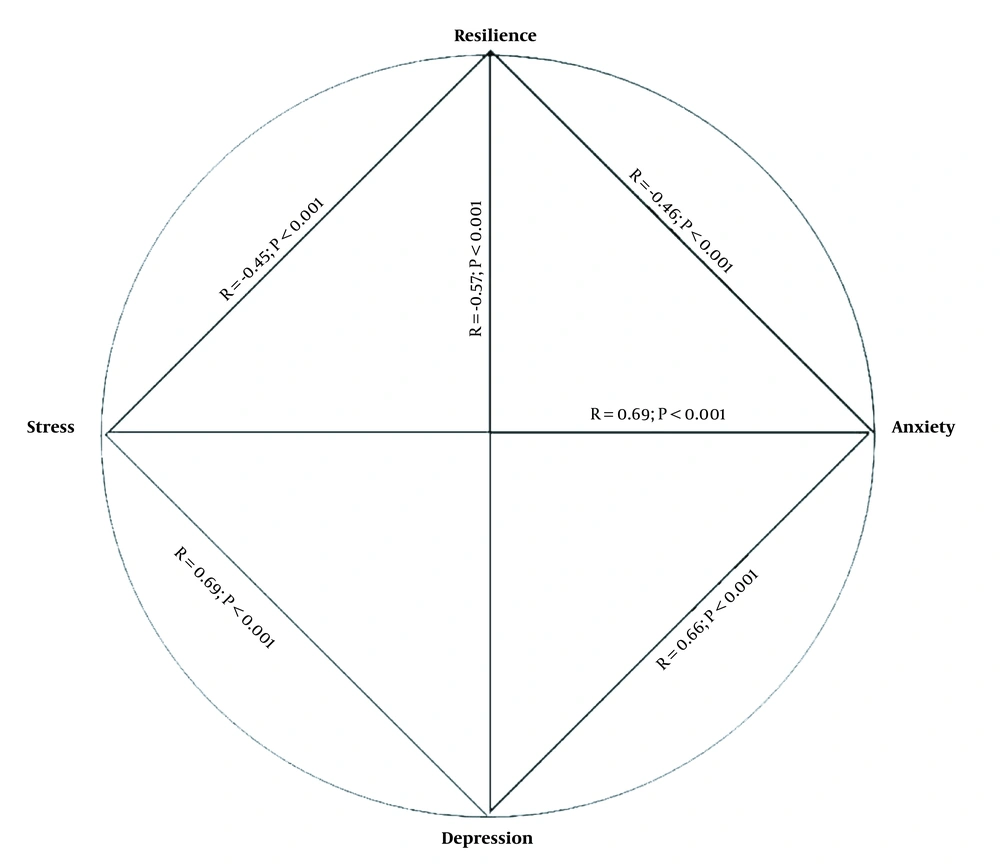
Figure 2 represents a relationship between resilience, anxiety, depression, and stress. Our results revealed a significant negative association of stress (r = -0.45, P < 0.001), depression (r = -0.57, P < 0.001), and anxiety (r = -0.46, P < 0.001) with resilience.
5. Discussion
In the present study, some psychological factors of faculty members of Birjand University of Medical Sciences, Iran, following the COVID-19 outbreak were assessed by an online self-reported questionnaire. Although there was a considerable number of studies about the impact of the COVID-19 outbreak on the mental health of the general population and many different subgroups with various types of psychopathologies such as depression, anxiety, and stress (26-32), the severe lack of studies focusing on faculty members’ mental health was observed. One study, compatible with our results, indicated that a substantial portion of university employees, more than 50%, experienced high levels of mood disturbances, anxiety, and stress in the early stage of the COVID-19 pandemic (33). Another study described the experiences of Canadian faculty members during the COVID-19 pandemic as overwhelming and exhausting (14). The findings of another research about the different experiences of faculty members emphasized frustration, depression, post-traumatic stress, and anxiety in this influential health educational group during the COVID-19 outbreak (13).
On the other hand, parallel with our study, the protective role of resilience against the formation or aggravation of different psychopathologies (17, 18) and its positive impact on mental health (34, 35) were frequently reported in scientific literature. Regarding the academic degree and faculty members’ ranks, some studies reported that individuals with a higher academic degree experienced lower stress levels (36, 37). Also, several studies in line with our findings revealed that as the years of work experience increase, experiencing mental distress decreases, which could be described by resilience levels upraise and adaptation to the environment (38-41).
Although we could not find any paper about the administrative positions during the COVID-19 outbreak in target groups, we hypothesize that obtaining administrative experience by increasing the coping strategies and resilience level could decrease mental distress; inversely, possessing some acceptable characteristics in coping strategies, resilience, collaboration, teamwork, and the lower degree of mental distress lead to select one individual for an administrative position.
Compatible with our results, one study showed that being single could predict common mental disorders in faculty members (42). Furthermore, the necessity to take permanent care of a family member during the pandemic could be a significant stressor leading to some mental distress in the caregivers, as our study and several other studies revealed (43-45). Additionally, suffering from previous pathologies was reported as a risk for higher levels of mental distress such as depression, anxiety, and stress in some studies (32, 46-48), which could be considered somehow consistent with our results about previous usage of sedative drugs and its association with depression and stress.
5.1. Conclusions
Our results revealed that the prevalence of depression, anxiety, and stress in the target group was considerable, and strengthening resilience with its protective role could be considered an effective solution. We suggest further studies in enormous scope and different medical and non-medical universities to investigate the effectiveness of resilience-strengthening methods in promoting faculty members’ mental health.