1. Background
The World Health Organization (WHO) has underlined that as an important component of antenatal care, preparation for labor plays an important role in reducing maternal mortality and improving women's birth experience (1). Readiness for childbirth can be defined as feeling ready for birth both physically and psychologically. Childbirth readiness (CR) is an important factor in pregnancy and delivery. Studies have reported that variables such as pregnant women’s duration of marriage, hyperemesis gravidarum, being between the ages of 30 and 44, and having two or more pregnancies are influential on CR (2).
Fear of childbirth (FC) is defined as anxiety and worry about childbirth (3). Fear of childbirth, an international phenomenon, is an uncomfortable feeling experienced during pregnancy (4).
It is known that pregnant women fear childbirth due to reasons such as being alone in a foreign environment, having a baby with a malformation or having a baby with damage during delivery, a feeling of uncertainty about how the birth will progress, lack of contractions, loss of control during the birth process, and distrust of obstetrical staff (5).
Different factors are listed in the literature as the cause of FC. Low education level, young age, lack of spousal support and abortion history, family type (nucleus-extended family), gestational week, and number of live births are some of the factors affecting the fear levels of pregnant women (6, 7). In addition, the absence of social support, parity, previous delivery methods, lack of knowledge, and depression also affect the fear of childbirth in pregnant women (8). Listening to negative birth experiences, age, education level, number of pregnancies, whether the pregnancy is planned, getting information about childbirth, and taking prenatal follow-up are cited as the other factors associated with FC (9).
The effects of multiple pregnancies on FC and CR were not addressed in previous studies. Multiple pregnancies are associated with adverse maternal and fetal outcomes. Maternal outcomes may be driven by hemodynamic changes that are more pronounced compared to singleton pregnancies. Maternal complications such as pregnancy-related hypertension, preeclampsia, gestational diabetes, intrahepatic cholestasis, or iron deficiency anemia are more common in multiple pregnancies than in singleton pregnancies (10). The incidence of multiple pregnancy is 1 - 3%. The rate of spontaneous multiple pregnancy has not changed and is 1/80 (11). This rate is 3.1% in Turkey (2019). Of these births, 96.4% were twins, 3.4% were triplets, and 0.2% were quadruplets or more (12). The use of assisted reproductive technologies (ART) due to infertility has increased over time, and it has led to an increase in the rates of multiple pregnancies (11).
Studies on multiple pregnancies have begun to increase over the years in parallel to this increasing trend. However, there is no data on both the CR and FC in multiple pregnancies. As far as we know, this is the first study to investigate the childbirth readiness and fear of childbirth in multiple pregnancies and the factors affecting CR and FC. We hope that the results of this study will address the data gap in the literature and stimulate future studies.
2. Objectives
This study aimed to determine the childbirth readiness and fear of childbirth in multiple pregnancies and investigate factors affecting CR and FC.
3. Methods
3.1. Type of Research
This cross-sectional descriptive study was conducted from April to November 2022.
3.2. Participants
The sample consisted of women aged 18 and over who agreed to participate in the study. Informed consent forms were shared among the groups after obtaining permission from the admins of the mothers of twins and triplets, twins and super mothers, and mother support team groups. Among these, 71 women with multiple pregnancies who filled out the questionnaire completely and returned it were included in the study. Six participants who were included in the study but whose data were missing were excluded. Since the number of women with multiple pregnancies in Turkey is not reported by state statistical institutions, the population size is unknown. Therefore, the sample size was calculated as 384 with the “sample calculation formula with the unknown population". The sample participants were reached through social media using the purposive sampling method. The study sample consisted of 71 women who voluntarily agreed to participate. At the end of the study, a “post hoc" power analysis was conducted to evaluate whether the sample was sufficient. The effect value of the study was calculated as 0.35, and the result of the “post hoc" power analysis performed by taking ἀ = 0.05 was found to be 0.794. A power between 0.70 - 0.90 was considered appropriate.
Inclusion criteria: (i) being 18 or older; (ii) volunteering to participate in the study; (iii) ability to read and write in Turkish; (iv) ability to use social media, smartphone, or computer.
Exclusion criteria: (i) having advanced reading comprehension problems; (ii) having any psychological problems.
3.3. Data Collection
The data was collected by the researchers from women who consented to participate in the study in relevant Facebook groups in Turkey. The participants who agreed to participate in the study and the researchers communicated via Facebook messenger. A survey link was sent to the participant whose compliance with the inclusion and exclusion criteria was evaluated. The researchers accompanied the participants during and after the questionnaire filling process and answered their questions.
The study data were collected using an online questionnaire created using Google Forms and the CR (10 items) and FC (10 items) sub-dimensions of the Prenatal Self-evaluation Questionnaire.
Online Questionnaire Form: The form prepared by the researchers in line with the literature (13-15) included a total of 15 questions about participants’ socio-demographic characteristics (age, marital status, educational status, place of residence, occupation, employment status, having a child and economic status), obstetric characteristics (number of pregnancies, number of births, number of children), how they conceived, how they wanted to give birth and status of getting information about pregnancy.
Prenatal Self-evaluation Questionnaire: This scale, developed by Lederman to evaluate the adaptation of women in the prenatal period to motherhood, is a 4-point Likert-type scale with a total of 79 items in seven sub-dimensions (16). Each sub-dimension contains 10 to 15 items. The sub-dimensions are as follows: “Acceptance of pregnancy”, “identification with a motherhood role, “relationship with mother”, “relationship with partner”, “readiness and preparation for labor (CR)”, “fear of pain, helplessness, and loss of control in labor (FC)”, and “well-being of self and baby”. The validity and reliability study of the scale in Turkey was conducted by Taşci Beydağ and Mete (17). The Cronbach alpha value was found to be 0.84 for the total scale, and its suitability for Turkish society was already demonstrated. Childbirth readiness and FC sub-dimensions of the Prenatal Self-evaluation Questionnaire were used in this study. Taşci Beydağ and Mete found Cronbach's alpha value for the “CR” and for the “FC” sub-dimensions as 0.84 and 0.72, respectively. The internal consistency coefficient found in this study was 0.76 for “CR” and 0.80 for “FC”. Each of these two sub-dimensions consists of 10 items with a minimum of 10 and a maximum of 40 points as scores. As the score obtained from the sub-dimensions increases, FC increases while CR decreases (17).
3.4. Statistical Analysis
Data analysis was performed using the SPSS 25 statistical package program. Normality control of the data was evaluated with the Kolmogorov-Smirnov test. Descriptive statistics were expressed as mean, standard deviation (SD), minimum and maximum values. Student t-test was used for independent means in the comparison of the childbirth readiness and FC sub-dimension mean scores for two independent groups, and one-way analysis of variance (ANOVA) was used for more than two independent groups. Tukey test was used to determine the group that generated the difference signal with the result of the one-way analysis of variance. The significance level was set as P < 0.05. Multiple linear regression analysis was performed to determine to what extent the variables affected CR and FC. In the study, a multiple regression model was established. Since there were multiple independent variables in this theoretical model, it was analyzed with the backward modeling of SPSS to establish a meaningful model. In the study, the presence of multiple collinearity, which is defined as a high level of correlation between independent variables, was checked. In this direction, variance inflation factor (VIF) values of the independent variables were examined. It was found to be below 10 for all variables.
3.5. Ethical Approval
The study was approved by the Non-interventional Clinical Research Ethics Committee at a university in Turkey (decision no: 776/756) and performed in accordance with the Helsinki Declaration. The participants first read the informed consent text explaining the purpose and rationale of the study in the link sent online. After being informed about the study, the volunteers filled out the questionnaire after answering "yes or no" to the question "would you like to participate in the study voluntarily?" at the end of the text. They were informed that they could withdraw from the study at any time without stating a reason.
4. Results
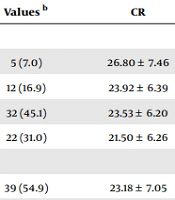
The mean age of the women participating in the study was 31.38 ± 4.48 (min: 21, max: 46) years, and their educational status was generally high school (45.1%) and university (31.0%). Among the participants, 54.9% were employed, and the majority (57.7%) expressed their income as moderate. Regarding the manner of conception of the 47.9% of the participating women with their first pregnancy, 46.5% became pregnant naturally, while 45.1% became pregnant with the in vitro fertilization methods. The mean gestational week of the pregnant women in the present study was 25.04 ± 6.75. It was determined that almost all of them (90.1%) had planned pregnancies, and the mean CR score was 23.19 ± 6.35, and the mean FC score was 26.54 ± 5.68 (Table 1).
| Characteristics | Values b | CR | Analysis (P-Value) | FC | Analysis (P-Value) |
|---|---|---|---|---|---|
| Level of education | F = 1.148; P = 0.336 | F = 0.062; P = 0.980 | |||
| Primary | 5 (7.0) | 26.80 ± 7.46 | 27.00 ± 2.92 | ||
| Secondary | 12 (16.9) | 23.92 ± 6.39 | 27.08 ± 5.04 | ||
| High school | 32 (45.1) | 23.53 ± 6.20 | 26.31 ± 5.90 | ||
| University | 22 (31.0) | 21.50 ± 6.26 | 26.50 ± 6.42 | ||
| Employment status | T = 3.915; P = 0.052 | T = 0.217; P = 0.643 | |||
| Yes | 39 (54.9) | 23.18 ± 7.05 | 27.23 ± 5.51 | ||
| No | 32 (45.1) | 23.22 ± 5.49 | 25.72 ± 5.88 | ||
| Family type | T = 0.017; P = 0.897 | T = 2.492; P = 0.119 | |||
| Nuclear family | 66 (93.0) | 23.14 ± 6.33 | 26.71 ± 5.84 | ||
| Extended family | 5 (7.0) | 24.00 ± 7.35 | 24.40 ± 2.30 | ||
| Income status | F = 2.157; P = 0.124 | F = 0.497; P = 0.611 | |||
| Good | 8 (11.3) | 25.13 ± 7.81 | 24.88 ± 6.98 | ||
| Moderate | 41 (57.7) | 24.02 ± 5.55 | 26.51 ± 5.70 | ||
| Low | 22 (31.0) | 20.95 ± 6.89 | 27.23 ± 5.31 | ||
| Wanting the pregnancy | T = 0.253; P = 0.617 | T = 0.006; P = 0.937 | |||
| Yes | 64 (90.1) | 22.61 ± 6.21 | 26.75 ± 5.72 | ||
| No | 7 (9.9) | 28.57 ± 5.26 | 24.71 ± 5.41 | ||
| Scale Score | |||||
| CR | |||||
| Mean ± SD | 23.19 ± 6.35 | ||||
| Min. | 10.00 | ||||
| Max. | 37.00 | ||||
| FC | |||||
| Mean ± SD | 26.53 ± 5.68 | ||||
| Min. | 16.00 | ||||
| Max. | 40.00 |
a F: One-way ANOVA; T: Student t-test.
b Values are presented as No. (%) unless otherwise indicated.
The comparison of the women’s CR mean scores and their socio-demographic characteristics showed that those with extended family structure and those who did not want to be pregnant had a higher CR total score, that the CR score average decreased as the education level increased, and that the women who reported their income as good had a higher CR score than those who assessed their income as moderate or low, and that these differences were not statistically significant (P > 0.05). The comparison of women’s FC mean scores and their socio-demographic characteristics showed that employed women, women with nuclear families, and those who wanted to be pregnant had higher total FC mean scores, and FC scores decreased as the education level increased. The women who reported their income as low had higher FC scores than those who assessed their income as moderate or good. It was determined that these differences were not statistically significant (P > 0.05) (Table 1). The mean week of gestation of the women participating in the study was 25.04 ± 6.75. It was found that half of the women (50.7%) had 1 as the number of gravidae, generally (78.9%) did not experience childbirth, 46.5% conceived naturally, and 45.1% conceived through in vitro fertilization (IVF) (Table 2).
| Characteristics | No. (%) | CR | Analysis (P-Value) | FC | Analysis (P-Value) |
|---|---|---|---|---|---|
| Gestational week | F = 0.568; P = 0.569 | F = 1.577; P = 0.214 | |||
| 1. Trimester (1 - 13 weeks) | 3 (4.2) | 22.00 ± 5.29 | 27.00 ± 2.00 | ||
| 2. Teamster (14 - 26 weeks) | 38 (53.5) | 23.94 ± 6.04 | 27.61 ± 5.89 | ||
| 3. Trimester (27 - 41 weeks) | 30 (42.3) | 22.36 ± 6.87 | 25.17 ± 5.48 | ||
| Gravida | F = 1.112; P = 0.351 | F = 1.285; P = 0.287 | |||
| 1 | 36 (50.7) | 21.74 ± 6.83 | 25.50 ± 5.60 | ||
| 2 | 18 (25.4) | 24.83 ± 5.83 | 28.61 ± 7.00 | ||
| 3 | 16 (22.5) | 23.94 ± 6.06 | 26.50 ± 4.21 | ||
| 4 | 1 (1.4) | 26.00 ± .001 | 23.00 ± .001 | ||
| Parity | F = 1.164; P = 0.318 | F = 1.860; P = 0.164 | |||
| 0 | 56 (78.9) | 23.05 ± 6.29 | 27.21 ± 5.85 | ||
| 1 | 11 (15.5) | 22.27 ± 6.96 | 24.00 ± 4.82 | ||
| 2 | 4 (5.6) | 27.75 ± 4.86 | 24.25 ± 3.40 | ||
| Manner of conception | F = 1.329; P = 0.272 | F = 7.702; P = 0.001 | |||
| Natural | 33 (46.5) | 23.52 ± 6.59 | 23.97 ± 4.16 | ||
| IVF | 32 (45.1) | 22.22 ± 5.60 | 28.59 ± 5.72 | ||
| ICSI | 6 (8.4) | 26.67 ± 8.43 | 29.83 ± 7.41 |
a F: One-way ANOVA; T: P < 0.01.
A comparison of the obstetrical characteristics of the participating women with the total CR mean scores showed that as the number of gravida and parity increased, the total CR mean scores increased. The CR mean score of those who became pregnant by intra-ctoplasmic sperm injection (ICSI: Vaccination) was higher than those who got pregnant naturally and via IVF. It was determined that there was no significant difference between them (P > 0.05) (Table 2).
A comparison of the obstetrical characteristics of the participating women with the total FC mean scores showed that as the number of gravid and parity increased, the mean FC score decreased. Still, there was no statistically significant difference between them (P > 0.05). Comparing the manner of conception and the total FC mean score demonstrated that those who got pregnant with IVF and ICSI had a higher mean FC score than those who got pregnant naturally. This difference was statistically significant (P < 0.01) (Table 2).
4.1. The Method of Obtaining Information About Pregnancy
The study concluded that 35.2% of the women wanted to have general anaesthesia cesarean, 21.1% painless normal birth, 19.7% with epidural anesthesia caesarean section, and 23.9% wanted to have a normal delivery. It was determined that 69.0% of the women received information about pregnancy from a health professional. The study concluded that there was no statistically significant difference between the birth preferences of the women and the total CR and FC mean scores (P > 0.05). A comparison of receiving information from a health professional with total CR and FC mean scores showed that the women with multiple pregnancies had higher CR and FC mean scores compared to those who received no training, with no significant difference between them (P > 0.05).
According to the Pearson correlation performed to compare the mean CR score and the mean FC score of the women participating in the present study, there was a significant and direct linear relationship between them (r = 0.42, P = 0.000).
As demonstrated in Table 3, the multiple linear regression analysis performed to determine the effect of factors on childbirth readiness was found to be statistically significant (F (24.533) = 12.270, P < 0001). The independent variables in the model explained 42% of the total variance in CR. According to our study, the reference category of the income level variable was “poor". Women with good and moderate incomes were 3.8 times less ready for delivery than women with poor incomes. Women with multiple pregnancies who wanted pregnancy were 6.9 times less ready for delivery than women who did not want pregnancy. The reference category for the duration of marriage was being married for less than 5 years. Accordingly, plural pregnant women who had been married for five years or more were 1.3 times less ready for delivery than pregnant women who had been married for less than 5 years. Accordingly, there was a negative significant relationship between the duration of marriage and income as the independent variables and the childbirth readiness score and a positive significant relationship between the state of wanting the pregnancy and the mean FC score (R2 = 0.426, P < 0.001).
| Model | B | SE | Beta | t | Sig |
|---|---|---|---|---|---|
| Fixed | 6.635 | 3.944 | 1.682 | 0.097 | |
| Income level | -3.875 | 1.298 | -0.284 | -2.986 | 0.004 |
| Whether the pregnancy is wanted | 6.992 | 2.004 | 0.331 | 3.489 | 0.001 |
| Duration of marriage | -1.327 | 0.423 | -0.297 | -3.138 | 0.003 |
| FC total score | 0.528 | 0.105 | 0.473 | 5.033 | 0.000 |
a Dependent variable: Readiness for childbirth score, R2 = 0.426, F (24.533) = 12.270, P = 0.000.
As demonstrated in Table 4, the multiple linear regression analysis performed to determine the effect of factors on FC was found to be statistically significant F (24.382) = 6.709, P < 0001. Accordingly, the reference category of the variable of wanting pregnancy was not wanting pregnancy, and multiples who wanted pregnancy experienced fear of childbirth 5 times more than those who did not want pregnancy. Hence, there was a significant positive correlation between the independent variable of the manner of conception, the mean CR score, and FC (R2 = 0.289, P < 0.001).
| Model | B | SE | Beta | t | Sig |
|---|---|---|---|---|---|
| Fixed | 16.976 | 3.429 | 4.951 | 0.000 | |
| Income level | 2.645 | 1.339 | 0.217 | 1.975 | 0.052 |
| Whether the pregnancy is wanted | -5.035 | 2.084 | -0.266 | -2.416 | 0.018 |
| Duration of marriage | 0.709 | 0.443 | 0.177 | 1.598 | 0.115 |
| CR total score | 0.525 | 0.104 | 0.586 | 5.033 | 0.000 |
a Dependent variable: Fear of childbirth score, R2 = 0.289, F (24.382) = 6.709, P = 0.000.
5. Discussion
This study, which examined the CR and FC status of women with multiple pregnancies and the factors affecting CR and FC, found that the mean CR score of the pregnant women was 23.19 ± 6.35, and the mean FC score was 26.54 ± 5.68. A study conducted by Mete et al. to examine the effect of participating in childbirth preparation classes on women’s CR and FC concluded that their mean CR score was 23.26 ± 5.55 before the training and 20.63 ± 10.68 at the end of the training (18). In the present study, which was similar to the pre-training CR total scores of the pregnant women, it can be argued that the CR levels of the women with multiple pregnancies, who were considered risky pregnancies, were not sufficient. The finding of a total CR score of 20.00 ± 4.8 in the study conducted by Akcayüzlü and Nazik (19) with 70 pregnant women with a diagnosis of hyperemesis gravidarum and many studies in the literature (2, 20-22) confirming lower levels of CR compared to the CR level found in this study confirms this finding. Although having low CR levels during multiple pregnancies is regarded as an expected result, this result obtained in this study regarding multiple pregnancies is the first in the literature to the best of our knowledge. Based on this, it can be argued that there is a need to develop interventions and practices that can positively affect childbirth readiness in multiple pregnancies. The World Health Organization considers preparation for childbirth and being prepared for pregnancy, delivery, and postpartum complications as an essential element of the antenatal care package (23).
In this study, the mean FC score of the pregnant women was found to be 26.53 ± 5.68. In studies using the same scale, the mean FC scores of healthy pregnant women ranged from 20 to 29 (2, 24, 25), while the mean total FC scores of high-risk pregnant women ranged from 22 to 28 (21, 22, 25, 26). In their study, Mete et al. (18) found the mean FC score as 24.24 ± 6.09 before the childbirth birth preparation training and 23.10 ± 8.80 after the training. The study conducted by Bulut and Özdemir (26) on pregnant women with hyperemesis gravidarum reported this value as 27.5 ± 5.4. This result was evaluated as quite high when compared to healthy and risky pregnant women who had a single pregnancy with a condition such as FC affecting childbirth. Although it is an expected result, it is the first contribution to the existing literature on multiple pregnancies.
Examination of the factors affecting the CR and FC of women with multiple pregnancies in this study showed that the average week of gestation of the pregnant women was 25.04 ± 6.75, a value almost twice as high as in the study of Akcayüzlü and Nazik (19). It is reported in the literature that as the week of gestation increases, the mean CR score decreases, and the acceptance of pregnancy increases (15). However, both this study and the study conducted by Eker and Aydin Besen examining the effect of adapting to pregnancy on breastfeeding self-efficacy found that the mean CR score of the pregnant women at 28 to 40 gestational weeks was higher (27). This result suggests that as the gestational week increases, the pregnant women are less ready for delivery. Therefore, providing birth preparation classes in the later weeks of pregnancy may be a solution, especially for risky pregnancies.
Coskuner Potur's et al. study reported that FC scores increased based on the week of gestation; FC scores changed between 28 and 32, and although there seemed to be an increase in FC based on the week of gestation, there was no significant difference (28). Güneş Tokgöz reported that the mean FC scores in the first and third trimesters were higher compared to the mean FC score in the second trimester (29). However, when we analyze the data on multiple pregnancies obtained in the present study, it is striking to see that the FC score decreased as the week of gestation increased. It can be suggested that more studies are needed on the FC in women with multiple pregnancies to interpret this result better, which is different from the literature.
This study concluded that the factors affecting CR were income status, duration of marriage, wanting the pregnancy, and FC. Unlike this study, Letose et al. reported a positive relationship between childbirth readiness and factors such as a history of obstetric complications, knowing the danger signs, having a positive attitude towards childbirth, starting antenatal care visits within the first 3 months of pregnancy, completing at least four antenatal care visits, residing in the city, having a profession and being in the high wealth bracket (30). The reason for this difference may be due to the demographic, cultural, and economic characteristics of the sample group in which the studies were conducted. This reveals the importance of conducting similar studies in different populations. On the other hand, Tilahun and Sinaga reported different variables affecting childbirth readiness, such as having antenatal follow-up in the first 4 months, having a high level of literacy, and having a partner with a high level of literacy and having knowledge about obstetric danger symptoms (31). Similar to the present study, Güneş Tokgöz’s study (29) reported that becoming pregnant voluntarily was associated with childbirth readiness, while Demirbas and Kadioglu reported that the duration of the marriage was related to childbirth readiness (2).
The factors affecting the fear of childbirth were determined as the method of conception and the level of CR. No correlation was found between socio-demographic characteristics and obstetric characteristics and factors such as wanting the pregnancy and the education level. Dencker et al. reviewed 21 articles in a systematic review of causes and consequences in DC research (32). Accordingly, the factors presented both in this study and other studies were not found to be associated with FC. Again, a study conducted by Soltani et al. in Iran found a positive relationship between education level, income status, and previous birth experience and FC (33), while the study conducted by Hildingsson et al. reported that pregnant women who did not receive information about pregnancy and those who had less than a year between two pregnancies experienced more fear (34). Mazúchová et al. found that the previous birth experience was especially related to FC (14). Güneş Tokgöz, on the other hand, reported that FC was related to the readiness to care for a baby and the state of getting information about pregnancy (29). Fear of childbirth may differ from culture to culture, depending on multiple pregnancy statuses. So far, no comparable data can be found, as the relationship between multiple pregnancies and FC has not been examined. However, even this result indicates that the issue should be investigated in more depth.
5.1. Limitations
In this study, we point out a few limitations inherent in descriptive and cross-sectional studies that would be useful to consider in future research. Since the data obtained in the study were obtained from social media groups, the results cannot be generalized to the whole society. However, the fact that women were from all regions of the country provided the opportunity to generalize to multiple pregnancies across the nation. In our study, we addressed the factors affecting fear of childbirth and readiness for childbirth suggested in the literature. This explains 28% to 42% of the established model. This result should be taken into consideration in future studies.
5.2. Conclusions
This study concluded that the majority of women wanted to have a cesarean section under general anesthesia, their CR scores and FC scores were above the average, and the factors affecting the CR status were income status, wanting the pregnancy, duration of the marriage, and FC.
It was determined that the factors affecting FC were the method of conception and readiness for childbirth. The CR and FC levels in this study were higher than the rates in the literature, and there was a positive relationship between them. As can be seen, both the childbirth readiness and the fear of childbirth in multiple pregnancies are different from singleton pregnancies. Childbirth readiness and FC are included as positive or negative triggers during pregnancy. For this reason, it is recommended that women with multiple pregnancies should be more thoroughly evaluated compared to those with a single pregnancy due to both high-risk and wanted pregnancies. The results of multiple pregnancies should be evaluated by conducting quantitative and qualitative studies on CR and FC.