1. Background
Good interprofessional (IP) collaboration and teamwork in the clinical environment are important factors for improving the skills of healthcare team members and providing healthcare services (1). Interprofessional collaboration is a process in which different health professionals with different specialties work alongside the patient and their families with an interaction based on mutual recognition, dependence, trust, understanding, and respect to set goals and share information, responsibilities, and power in decision-making and problem-solving in order to achieve the best and most effective outcomes for the patient and the family (2). Effective IP collaboration is necessary for ensuring the safety of patients and their recovery (3). Successful IP collaboration depends greatly on effective IP communication, which is described as sharing information verbally, in written form, etc., between health professionals of different specialties in order to achieve positive patient care outcomes, where these communications can be either intentional or unintentional (4).
Improving the effectiveness of IP communications between healthcare workers is a global priority because ineffective communications in this area lead to delayed treatment, misdiagnosis, medication errors, patient injuries, or death (5). Conflicts between healthcare professionals are increasing in hospitals. Kim et al. showed that more than 80% of healthcare professionals in South Korea experienced disagreements with their peers more than once a year (3). Conflicts between healthcare professionals who deal with patients’ lives can have gruesome effects on their performance and interfere with the decision-making process, which can finally cause harm to patients (3).
In order to establish IP communications between the members of the healthcare team, mutual understanding, respecting personal roles, and sharing goals and values are important (6). Also, people with various professions are trained differently in terms of communication style, and these differences can lead to conflict. For example, nurses are trained in such a way to share details when establishing communication, and on the other hand, physicians are trained to be brief (5). In this regard, studies emphasize the need for specifying people’s roles in the healthcare team, training healthcare workers on their roles, team building, management, clinical, collaboration, and teamwork skills, clarifying the goals of communication, assessing programs and organizational protocols to guard teamwork, and effective interprofessional communications (7, 8).
Since nurses pursue the requests of paraclinical services of inpatients and make coordination for carrying out these services, such as lab tests, requests for radiology, ultrasonography, echocardiography, etc., it is essential to pay attention to the communication of nurses with other paramedics. However, there have not been enough studies on the IP communications of nurses with paramedics, and most of existing studies have used quantitative approaches to assess communication between nurses and physicians (9, 10). Meanwhile, qualitative research can have an effective role in clarifying ambiguous concepts and illuminating unknown areas (11). Divulging the opinions and experiences of nurses and paramedics and their perception of the challenges of IP communications by qualitative analysis can provide valuable data for removing existing problems and, hence, ensuring the quality of healthcare services provided to patients via solving available challenges and improving IP communications. It should also be noted that the obstacles to IP communication between nurses and paramedics can vary depending on the research environment and the financial and human resources of health systems in different societies.
2. Objectives
This study was conducted with a qualitative approach in order to explain the obstacles to IP communication between nurses and paramedics.
3. Methods
3.1. Study Design
This qualitative study was conducted using the content analysis method.
3.2. Participants
The main participants of this study were 11 nurses and paramedics selected by purposeful sampling among the personnel working in the teaching hospitals affiliated with the Jahrom University of Medical Sciences, Iran. The data were gathered from May to September 2022. The participants of this study were selected among those who were willing to participate in the study, had at least one year of work experience, and held a bachelor’s degree or higher.
3.3. Data Acquisition
Data was collected by conducting semi-structured, individual, and in-depth interviews. A total of 11 interviews were carried out by the first author. The participants were interviewed one by one and face-to-face in a quiet place. The participants determined the time and place of the interview. The interviews were started with general questions, such as “Based on your experiences, what communication challenges do you face?” and were continued with detailed questions, such as “What are your communication challenges with paramedics (nursing) staff?”, “What factors do affect your professional communications with paramedics (nursing) staff?” and “According to your professional communication experience with paramedics staff, what obstacles exist in this area?”. Next, probing questions such as “What do you mean?” or “Can you give an example?” were asked. Each interview lasted between 30 to 60 minutes.
3.4. Data Analysis
All interviews were recorded by a digital voice recorder. Immediately after the interviews, the voices were listened to by the main researcher several times, transcribed, and analyzed at the same time. Data analyses were carried out using the conventional content analysis method and the Graneheim and Lundman approach. The interviews were transcribed verbatim, and the texts were read through several times to make sense of the entire transcription. The text was disintegrated into meaningful units and then condensed for clarity and brevity. The condensed meaning units were abridged and labeled with codes. The codes were then sorted into subcategories based on their similarities and differences according to constant comparative analysis. Themes, as the expression of the latent content of the text, were finally extracted (12). The interviews were continued until reaching data saturation (i.e., the emergence of no new codes).
3.5. Rigor
In order to assess the rigor and trustworthiness of the data, Lincoln and Guba’s criteria were used (13). In this regard, in order to ensure the accuracy of findings, prolonged engagement of researchers with the topic and paying attention to the analysis of negative cases were considered. In order to increase confirmability, the texts of selected interviews and their codes were provided to colleagues experienced in qualitative studies (peer debriefing). In order to gain transferability, the study’s steps (i.e., sampling, subjects’ specifications, and appropriate quotations) were reported in detail (thick description). Bracketing, peer-checking, and moving back and forth from data collection to data analysis helped to ensure dependability, which was assessed through data triangulation by selecting different individuals (i.e., diversity in age, gender, education, and position).
3.6. Ethical Considerations
The current study was carried out by observing the revised principles of the Declaration of Helsinki, a statement on the ethical principles that guide physicians and other health professionals in conducting medical research related to humans. In order to observe ethical considerations, the objectives of the research were explained to interviewees, and written consent was obtained from them. Participation in this research was voluntary; all research content and recorded data were reminded confidential, and participants’ anonymity was ensured (ethical approval code: IR.JUMS.REC.1398.004).
4. Results
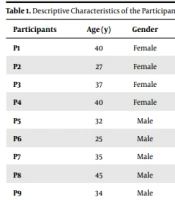
The participants of this study comprised 1 supervisor, 3 head nurses, 5 nurses working in different wards, the head of the radiology department, and 1 laboratory personnel. Seven (63.6%) of the participants were males. The means of age and work experience of the participants were 34.00 ± 6.14 and 12.18 ± 6.52 years, respectively (Table 1).
| Participants | Age (y) | Gender | Education Level | Job Position | Work Experience (y) |
|---|---|---|---|---|---|
| P1 | 40 | Female | Bachelor’s degree in nursing | Head nurse | 18 |
| P2 | 27 | Female | Bachelor’s degree in nursing | Nurse | 4 |
| P3 | 37 | Female | Master’s degree in nursing | Head nurse | 15 |
| P4 | 40 | Female | Bachelor’s degree in nursing | Laboratory science technician | 15 |
| P5 | 32 | Male | Bachelor’s degree in nursing | Nurse | 12 |
| P6 | 25 | Male | Master’s degree in nursing | Nursing supervisor | 3 |
| P7 | 35 | Male | Bachelor’s degree in nursing | Nurse | 13 |
| P8 | 45 | Male | Bachelor’s degree in nursing | Head of the radiology department | 25 |
| P9 | 34 | Male | Master’s degree in nursing | Head nurse | 12 |
| P10 | 30 | Male | Bachelor’s degree in nursing | Nurse | 8 |
| P11 | 29 | Male | Bachelor’s degree in nursing | Nurse | 7 |
The 3 main themes were “human resources challenges,” “lack of coordination between paramedics and nursing departments,” and “emergency situations.” Themes and subthemes are displayed in Table 2.
| Themes | Subthemes | Meaning Units |
|---|---|---|
| Human resources challenges | Personnel shortage | Shortage of paramedics |
| Shortage of nursing staff | ||
| Insufficient experience and knowledge of personnel | Inadequate knowledge of personnel | |
| Inadequate experience of personnel | ||
| Personnel errors during carrying out professional duties | Failure to complete duties timely | |
| Failure to complete duties carefully and patiently | ||
| Lack of coordination between departments | Lack of coordination of interdepartmental programs | Lack of coordination of programs within the department |
| Lack of coordination of extra-organizational rules | ||
| Shortage of tools and equipment in departments | Lack of equipment | |
| Lack of consumables | ||
| Challenges in emergency situations | Different perceptions of personnel from emergency situations | Different interpretations of an emergency patient |
| Inadequate understanding of emergency situations | ||
| Referral of emergency patients to paraclinical units for follow-up testing | Referral of emergency patients to paraclinical departments | |
| Time limitations in receiving the results of paraclinical tests |
4.1. Human Resources Challenges
The first theme was human resources challenges, which included personnel shortages, insufficient knowledge and experience of personnel, and personnel errors during carrying out professional duties.
4.1.1. Personnel Shortage
From the point of view of the participants, one of the challenges of IP communication between nurses and paramedics was the shortage of personnel, hampering the provision of diagnostic-therapeutic services and leading to time limitations for service provision. One of the participants declared:
“One of our problems is that in evening and night shifts, the number of personnel in departments such as radiology, laboratory, etc., is reduced, and the work process slows down, which leads to conflicts between nursing personnel and paramedics with regard to processing the patient’s condition.” (P6)
4.1.2. Insufficient Knowledge and Experience of Personnel
Insufficient knowledge and experience of some personnel rendered a potential factor that sometimes could lead to challenges between nurses and paramedics. One of the participants explained:
“In one of the paraclinical departments, they had employed a new and inexperienced personnel who was not familiar with the routines and work process, which made us nervous.” (P2)
4.1.3. Personnel’s Errors in Carrying Out Professional Duties
From the point of view of the participants of this study, personnel errors and mistakes were another factor leading to communicational challenges between nurses and paramedics. One of the participants explained:
“Once, a patient’s BUN was reported as 1.2 and creatinine as 12. The nurses checked and reported that it did not match with other tests. I checked and realized that the problem was in reporting the lab results and that our lab personnel placed the decimal point in the wrong place.” (P4)
4.2. Lack of Coordination Between Departments
The second main theme in this study was the lack of coordination between nursing and paramedics departments. This theme is comprised of the lack of coordination between rules, programs, and routines in the nursing and paraclinical departments and the shortage of devices and equipment in paraclinical departments respective to the needs of nursing departments.
4.2.1. Lack of Coordination Between Interdepartmental Programs
The participants of the current study presumed the lack of coordination between the rules, programs, and routines of the nursing and paramedical departments as one of the factors leading to tension between nurses and paramedics. In fact, this issue was noted as a cause for delay and time wastage during carrying out activities, increasing healthcare tasks with regard to patient follow-up. Participants stated:
“Sometimes, physiotherapy personnel take leave without informing other departments and assigning replacement staff; therefore, there is no one to handle patients’ tasks…” (P3)
“Laboratory personnel have defined a routine for themselves. For example, they say that the number of samplings carried out by laboratory personnel in inpatient wards should not exceed 100 samples in the morning shift, and whenever the number of blood samples reaches 100, they stop sampling whether there are patients remaining or not, so we should take the rest of samples ourselves.” (P9)
4.2.2. Shortage of Tools and Equipment in the Departments
Another issue that the nurses participating in this study considered to be a challenge for communication between paramedical staff and themselves was a shortage of devices and equipment, leading to delays in reporting paramedical tests’ results and, as a result, taking more time for tasks to be accomplished. In some cases, this issue may even lead to communication tensions between nurses and paraclinical staff. One of the participants explained:
“Laboratory personnel do not provide the results of the tests requested in the night shift sooner than 9 a.m. and, on the other hand, they even ignore performing some tests at nights … they always justify by saying that a device is broken…” (P1)
“There is no eye examination equipment for monitoring the vision of premature babies in the NICU or in the ophthalmology department of the hospital, and the baby shall be transferred to a specialized clinic outside the hospital, which makes coordination in this regard time-consuming and exhausting.” (P11)
4.3. Challenges in Emergency Situations
The third main theme was challenges in emergencies, which included different understandings of an emergency situation and transferring the responsibility of emergency patients to paraclinical departments.
4.3.1. Different Perceptions of Personnel from Emergency Situations
In several cases, paraclinical personnel were not able to distinguish an emergency situation from a non-emergency situation, leading to tension between nurses and paraclinical staff. One of the nurses participating in this research stated:
“A nurse really knows the importance of a medical test result or a CT scan result of a patient suffering from chest pain or brain concussion, but laboratory and radiology personnel are not fully aware of the sensitivity of these cases. We sometimes argue about these cases…” (P7)
4.3.2. Referral of Emergency Patients to Paraclinical Departments for Follow-up Testing
People referring to medical centers and hospitals are generally patients or companions of patients who sometimes have requests beyond the rules and regulations of hospitals. This is because they are occasionally unaware of the processes of admission and treatment or do not have enough patience. In many cases, the continuation of the treatment process depends on receiving the results of medical tests from paraclinical departments. The delayed arrival of these results makes nurses upset, compelling them to transfer the pressure from themselves to paraclinical staff, which consequently leads to paraclinical staff complaints. One of the participants explained:
“Companions of emergency patients want to receive answers very quickly. So, sometimes, nursing personnel have to send them to paraclinical departments to pursue the patient’s test results, conveying pressure on these departments. This issue creates tension...” (P8)
5. Discussion
The current study aimed to explain the obstacles to IP communication between nurses and paramedics. The main themes identified were human resources challenges, lack of coordination between the nursing and paramedical departments, and challenges in emergency situations. Most previous studies have focused on interactions between physicians and nurses (14, 15) or nurses and nurses (16), and there was no study assessing IP communication between nurses and paramedics.
Based on the experiences of our participants, human resources challenges were among the important issues pertaining to IP communication. The shortage of staff is considered one of the most important challenges in health fields (17). The lack of human resources is a problem that can be seen in clinical environments, leading to extra workload that affects intradisciplinary and interdisciplinary collaboration and the quality of services (18, 19).
In Shohani et al.’s study, among the important factors affecting IP collaboration between nurses were human resources problems, including the accountability of nurses for imposed activities, as well as disproportionate nursing staff and workload (20). The shortage of workforce is not limited to nurses but also exists in other health-related sectors (21).
Newly graduated health personnel, lack of interpersonal skills, and other factors related to the lack of experience have been reported as the most common barriers to effective IP communication (22). Interprofessional collaboration depends on knowledge and skills, as well as the ability to adapt them appropriately by the parties of communication. Jafari et al. noted that the clinical skills and experience of nurses were the basic factors required for effective IP communication (23). Among other factors have been personal attitudes and opinions on collaboration, teamwork, personal traits, personal experiences, and personal problems of personnel (20, 24). In order to improve IP communication between nurses and paramedics, it is suggested to hold training courses on communication skills and methods for paramedics and nursing students to improve their interpersonal relationships and communication abilities. Regarding the impact of individuals’ attitudes toward IP collaboration and effective communication, it is advisable to assess and improve nurses’ and paramedics’ attitudes toward IP collaboration (25). Also, officials need to pay more attention to paramedics’ and nurses’ personal life problems, improve their welfare, and reduce their workload via recruiting sufficient numbers of personnel and balanced apportioning of duties (21, 26). In the process of IP collaboration, the clarification of team structure is a necessary item. Interprofessional collaboration is affected by the qualification of team members. Therefore, effective training shall include the expansion of communication skills of team members, understanding of organizational objectives, and achieving the sources required for this collaboration (27).
According to the participants in this study, the theme of the lack of coordination between the nursing and paramedic departments included the shortage of devices and equipment in paraclinical departments disproportionate to the needs of nursing departments and the lack of coordination between the rules, routines, and programs of the nursing and paraclinical departments. These discrepancies are believed to create tension, disagreements, and disputes between nurses and paramedics in the working environment.
In support of these findings, access to resources and facilities by paramedical departments is very important for their ability to fulfill the requirements of nurses. Also, nurses with higher access to resources, equipment, and facilities feel more empowered to deliver quality patient care (28). Shohani declared that the lack of facilities in any form would lead to undesirable patient care, wasting the time of nurses, and the inability of nurses to help their coworkers in urgent conditions (21). This finding was consistent with the results of other studies (29, 30). Sajadi and Zaboli also indicated that coordination in teamwork was the main key and a requirement for the success of hospitals in dealing with crises (31).
The participants of this study believed that the lack of coordination between intra-department rules and regulations and the general rules of the organization or the disciplines of other departments could lead to misunderstanding and tension between paramedics and nurses. Although these notions seem to be basic and obvious, we could not find studies supporting this argument. Therefore, our observations can be considered new findings that need more research and assessments in future studies.
Another source of tension between nurses and the paraclinical staff was identified to rise during emergency situations. Up-to-date knowledge and skills are necessary for managing interactions and the establishment of effective IP collaboration and communication, particularly in emergencies. Therefore, making use of communication skills by nurses and paramedics is essential. However, other researchers have not explicitly addressed occupational relations in emergencies as factors that can create occupational tensions. Nobahar identified that delayed reporting of the results of paraclinical studies was a barrier to professional communication in CCUs (32). The results of Winsett et al.’s study showed that communication failure during emergency situations could compromise effective nursing care (33).
5.1. Limitations
Individual interviews were used in this study to gather the data required. It is suggested to use other methods, such as focus group interviews, in future studies.
5.2. Conclusions
Nurses and paramedics face numerous challenges in their IP communication, including a shortage of human resources, a lack of coordination between departments, and challenges during emergency situations. These challenges are influenced by different human and managerial factors, and identifying them is a significant step toward improving IP communication between nurses and paramedics. Hospital managers can use the findings of this study to improve the quality of IP communications in all aspects by planning and taking action to remove these challenges and prepare the context for more effective IP communications and teamwork. Since medical education centers are considered a place for both providing health services to patients and training students in different health fields, it is further suggested to assess the challenges of professional communication between nurses and students of different health disciplines (medical, nursing, etc.).